Researchers uncover new drug target for fragile X
Deleting an enzyme that regulates protein synthesis reverses some of the molecular and behavioral deficits in a mouse model of fragile X syndrome, according to research published 2 October in Neuron.
-
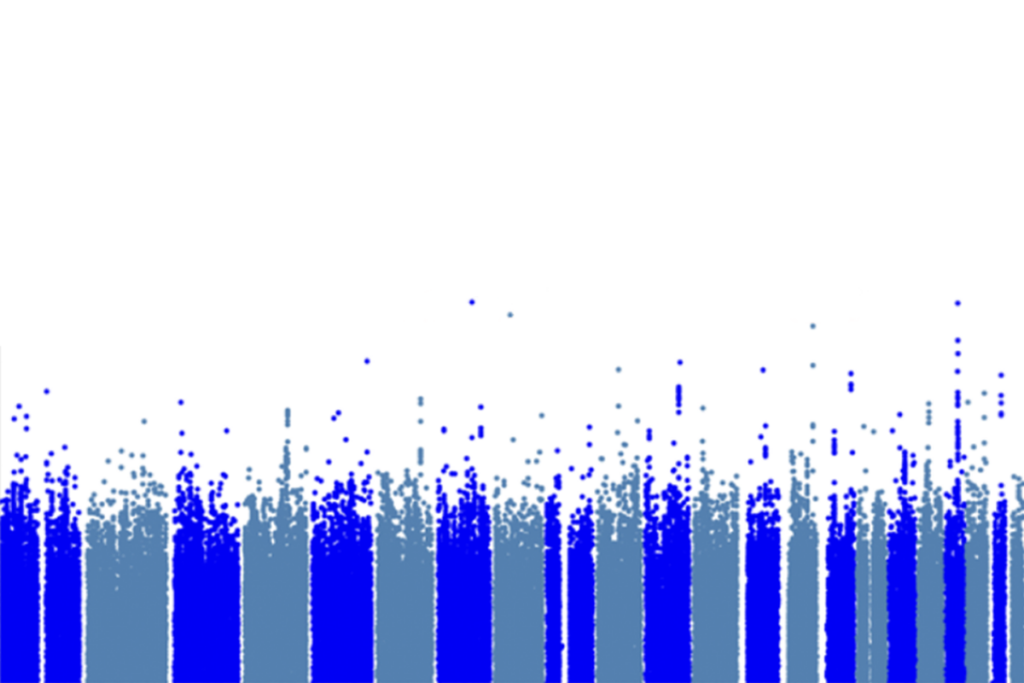
Protein profusion: Mice lacking the fragile X gene make more protein (top) than controls do (center). Deleting an enzyme called S6K1 (bottom) brings proteins back to normal levels.
Deleting an enzyme that regulates protein synthesis reverses some of the molecular and behavioral deficits in a mouse model of fragile X syndrome, according to research published 3 October in Neuron1.
Overproduction of proteins at synapses, the junctions between brain cells, is thought to be a molecular hallmark of fragile X syndrome, an inherited form of intellectual disability that’s often accompanied by autism. The same phenomenon may play a role in autism as well.
The enzyme, called S6 kinase 1, or S6K1, represents a new drug target for treating fragile X syndrome and, possibly, autism.
“For certain classes of mutations that cause autism in people, this is a potential good target,” says Eric Klann, professor of neural science at New York University’s Center for Neural Science. “It’s hard to know whether that would be true [for all types of autism].”
Klann and his team are testing in mice a drug that inhibits the S6K1 enzyme, but don’t yet know whether it is effective.
Because compounds that target the enzyme work differently than drugs under development for fragile X syndrome, the different approaches could be used together, several researchers say.
For example, a study published 25 September in Nature Communications found that targeting the endocannabinoid system — which responds to molecules that resemble the active ingredient in marijuana — may also help treat fragile X syndrome2.
Mice modeling the syndrome lack FMRP protein, which normally suppresses protein synthesis. As a result, the mice have an overabundance of proteins.
Clinical trials that are under way aim to cut down this protein production indirectly via a chemical signaling pathway, says Gary J. Bassell, professor of cell biology and neurology at Emory University School of Medicine in Atlanta, who was not involved in the new study.
Blocking S6K1 directly targets the molecular machinery that produces proteins, Bassell says. “It’s very clever and effective.”
Reversal of fate:
Fragile X syndrome is caused by a mutation in the FMR1 gene that blocks production of FMRP. Like people with the syndrome, the model mice have problems in motor coordination and memory.
In addition to excess protein synthesis, the mice have more so-called dendritic spines, tiny neuronal protrusions that help transmit brain signals, and more immature ones, than control mice do. Signaling through a receptor called mGluR5 is also overactive in the mice.
Deleting the S6K1 gene in these mice reverses all these traits, the researchers found. It decreases the number of spines, and improves performance on tests of motor coordination, learning and behavioral flexibility, such as the mouse’s willingness to go the wrong way in a maze. The mice also get better at recognizing unfamiliar mice or objects.
However, these mice continue to show repetitive behaviors and abnormal production of some proteins, suggesting that a drug that limits S6K1 would not be a cure-all for fragile X.
There are drugs, including one developed by pharmaceutical giant Pfizer, that dampen S6K1 activity, says Klann.
The Pfizer compound was developed to target the mTOR pathway, believed to be involved in many cancers, as well as autism and the related disorder tuberous sclerosis.
One potential concern about using the compound to treat fragile X syndrome is whether it can dampen enough S6K1 activity. For unknown reasons, fragile X mice missing just one copy of the S6K1 gene have too much S6K1 activity rather than too little.
So a drug that dampens but doesn’t eliminate S6K1 activity might create more problems than it solves, Klann says. “You’re not going to be able to inhibit 100 percent of enzyme activity. So how much are you going to have to [inhibit to] be able to get any kind of reversal [of symptoms]?” Klann says.
It’s also unclear whether a drug inhibiting S6K1 would work if given in childhood, because the mice in the study lacked S6K1 from conception, Klann says. However, several studies of autism-related conditions have suggested that symptoms can be reversed later in life.
Treating fragile X syndrome and autism may require a combination of different strategies to return protein production to normal levels, Bassell says.
A pair of studies published 19 September in Science Translational Medicine suggests that the drug arbaclofen may effectively treat the social deficits that often accompany fragile X and autism.
Because S6K1 functions earlier in the protein synthesis cascade than other drugs being developed for fragile X, it may be more broadly effective in people with autism, Bassell says.
However, S6K1 has effects outside the brain — meaning that blocking it could have side effects elsewhere in the body, notes Mark Bear, professor of neuroscience at the Massachusetts Institute of Technology, who helped develop arbaclofen and mGluR5-based drugs.
“But this is true for all approaches,” says Bear, who launched Seaside Therapeutics, a Massachusetts-based company developing several fragile X drugs. “The goal is to maximize therapeutic benefit and minimize unwanted side effects.”
Klann says the potential side effect he’s primarily concerned about is catalepsy, a trance-like state in which people don’t respond to their environment. That’s because mice that lack S6K1 (but not FMRP) have abnormally low activity levels, as well as slowed growth during adolescence.
Correction: This article has been modified from the original. It has been changed to reflect that signaling through the receptor mGluR5 is overactive, rather than the receptor itself.
References:
1: Bhattacharya A. et al. Neuron Epub ahead of print (2012)
2: Jung K.M. et al. Nat. Commun. 3, 1080 (2012) PubMed
Explore more from The Transmitter