This paper changed my life: Shane Liddelow on two papers that upended astrocyte research
A game-changing cell culture method developed in Ben Barres’ lab completely transformed the way we study astrocytes and helped me build a career studying their reactive substates.
Answers have been edited for length and clarity.
What papers changed your life?:
Development of a method for the purification and culture of rodent astrocytes. Foo L.C., Allen N.J., Bushong E.A., Ventura P.B., Chung W.S., Zhou L., Cahoy J.D., Daneman R., Zong H., Ellisman M.H. and Barres B.A. Neuron (2011); and Genomic analysis of reactive astrogliosis. Zamanian J.L., Xu L., Foo L.C., Nouri N., Zhou L., Giffard R.G. and Barres B.A. Journal of Neuroscience (2012)
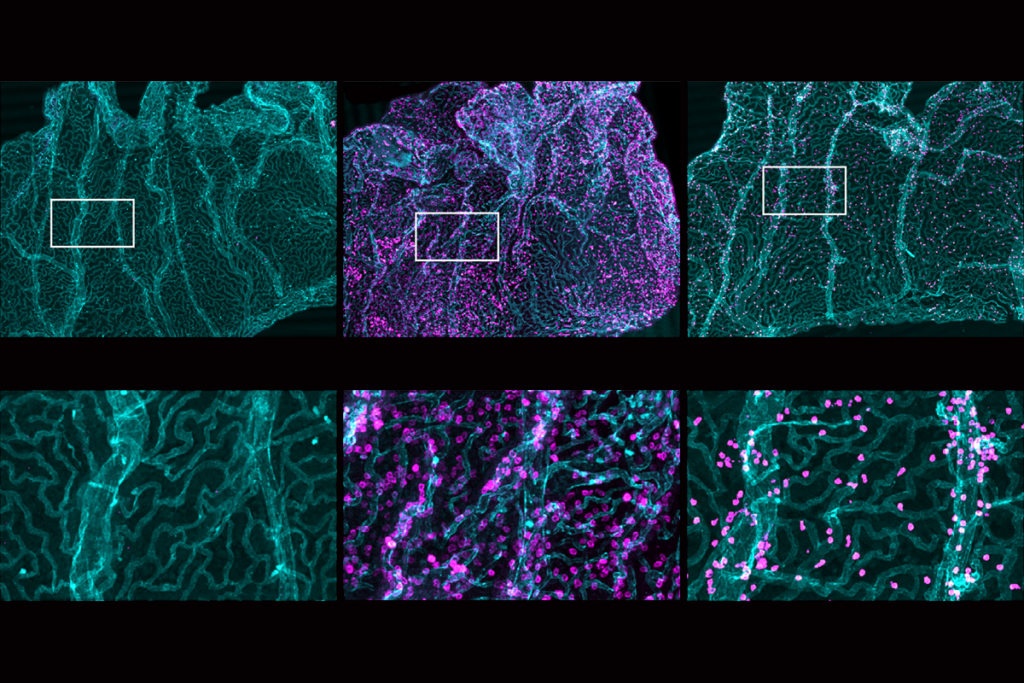
These two papers from the late Ben Barres’ lab at Stanford University pushed forward the field’s understanding of astrocyte function—under both normal physiological and disease conditions. In the 2011 Neuron paper, Barres and his colleagues developed a new method to culture rat and mouse brain astrocytes in serum-free conditions. This was an essential breakthrough because up to that point, culturing astrocytes required serum-containing media, a highly non-physiological environment (most serum proteins don’t cross the blood-brain barrier). What happens when you have blood in your brain? A stroke! Which is a bad thing.
In a separate paper a year later, the researchers demonstrated for the first time that astrocytes show highly distinct genetic profiles in response to specific injury, suggesting the existence of multiple unique reactive substates. They isolated astrocytes from mice that had undergone one of two different immune stresses—an ischemic stroke or neuroinflammation—and found that gene expression in these cells, dubbed “reactive astrocytes,” differed depending on the stressor. The findings provided a glimpse of the cells’ function in the brain: playing a key role in neuronal survival in health and disease.
When did you first encounter these papers?
I was fortunate enough to learn about these papers right before they were published, when I was interviewing for a postdoctoral position in Barres’ lab. I remember sitting in the sun outside the Sherman Fairchild Science Building, having coffee while chatting with the two lead authors, Jennifer Zamanian and Lynette Foo, about their results and thinking to myself, “This is cool. I could do so much with this.”
Why are these papers meaningful to you?
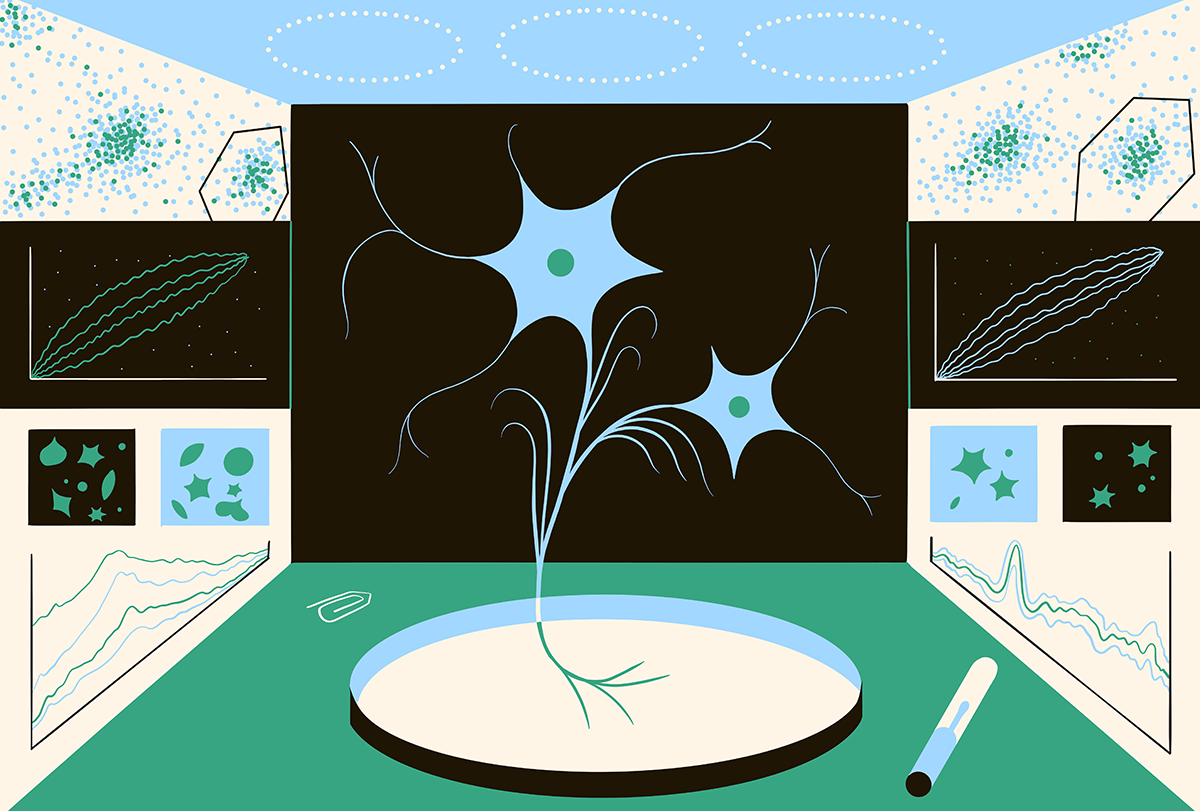
This work was among the first to suggest to me that there could be more than one type of reactive astrocyte. I saw the cell signatures described in Jennifer’s paper as a “road map” of sorts. If we could recapitulate this gene-expression signature in a dish, we would be able to finally complete a full functional characterization of a substate of reactive astrocytes. Given that serum caused non-physiological reactive gene-expression changes in astrocytes, this would not have been possible without the innovative astrocyte culture protocol that Lynette established in her paper.
How did these papers change how you think about neuroscience or challenge your previous assumptions?
The idea of reactive astrocytes was not new and had been described as early as the 1800s by multiple German pathologists. Since then, the field of astrocyte biology had made great strides in understanding what it is that astrocytes do—they promote synapse formation and regulate synaptic pruning, modulate blood-brain barrier trafficking and recycle neurotransmitters to limit excitotoxicity. These are integral functions of astrocytes in the normal physiological brain, but it was unclear if astrocytes could no longer perform these functions when reactive. For most of the history of reactive astrocytes studies, we lacked tools to carefully dissect the function of these disease-associated cells. At the time these two papers came out, there were sparring ideas about whether reactive astrocytes were harmful or helpful. These findings helped make it more apparent that the truth lay somewhere between these two extremes.
How did this research influence your career path?
Having completed a Ph.D. in pharmacology focused on the transport of serum proteins across the choroid plexus of the developing gray short-tailed South American opossum, my jump to cell and glial biology was a big one. These two papers from the Barres Lab were published just as I was changing fields; without them, I am not sure I would have been able to build a career digging deep into the intricacies of reactive astrocyte biology. The genetic signatures of reactivity the Barres Lab described using purified astrocyte cultures enabled everything we have discovered in glia research since.
I used serum-free astrocyte cultures during my postdoc to identify that TNF, IL1a and C1q are required and sufficient to induce neurotoxic reactive astrocytes (just one of many reactive astrocytes substates). This helped us identify that neurotoxic reactive astrocytes induce neuron cell death by secreting long-chain saturated free fatty acids. When my lab repeated Jennifer’s experiments using scRNAseq, we discovered even more substates of reactive astrocytes and again used Lynette’s serum-free culture methods to develop a cocktail to induce what we now refer to as “interferon-responsive reactive astrocytes.” We continue to use these methods to find new reactive signatures and combine these road maps with serum-free cultures to study specific astrocyte substate functions.
Is there an underappreciated aspect of the papers you think other neuroscientists should know about?
The importance of using serum-free conditions for culturing central nervous system cells is frequently overlooked. Before the Barres Lab established this method, astrocyte cultures required serum-containing media. Studies using this method led to some important findings, such as astrocyte’s role in synapse formation and their function as immune cells. However, serum conditions remained largely inappropriate for the study of reactivity and astrocytes in disease. Translatable discoveries in this space had been limited because serum components irreversibly alter the gene expression, morphology and function of astrocytes and microglia. The protocol Lynette developed completely changed the way we study astrocytes. Serum-free methods have since been developed for many central nervous system cells, driving exciting discoveries in other cell types as they have for us in astrocyte biology.
What paper changed your life?
Recommended reading
This paper changed my Life: Bill Newsome reflects on a quadrilogy of classic visual perception studies
Explore more from The Transmitter
Imagining the ultimate systems neuroscience paper