Even though a remarkable 21 percent of adults in the United States will experience a mood disorder at some point in their lives, we do not fully understand what causes them, and existing treatments do not work for everyone. How can we best move toward an impactful understanding of mood and mood disorders, with the longer-term goal of helping these people? What, if anything, makes mood fundamentally different from, say, memory? The answer turns out to be complex and nuanced—here, I hope to unpack it. I also ask brain and mind researchers with diverse perspectives to chime in.
A
mong contemporary brain and mind researchers, I have yet to find any whose position is driven by the notion that some force in the universe beyond the brain, like a nonmaterial soul, gives rise to mood. Rather, the researchers generally agree that our brains mediate
all mental function. If everyone agrees that both memory and mood disorders follow from things that happen in the brain, why would the former but not the latter qualify as “brain disorders”?
For many researchers, the debate centers on the level of focus: Does the brain or the mind cause fluctuations in mood? By analogy, consider Huntington’s disease, a neurodegenerative disorder caused by a mutation in a single gene. We regard Huntington’s as a genetically inherited brain disorder, not a subatomic particle disorder. The genetic mutation is, in fact, caused by a rearrangement of subatomic particles. But that’s not a helpful way to think about the causes of Huntington’s, insofar as our goal is to treat and cure it; it’s simply the wrong level. Likewise, some researchers argue that the brain is not a useful level to think about the causes of mood and mood disorders insofar as we want to understand and treat them.
To elaborate a bit more, consider the phrase “insomnia causes fatigue.” No one disputes it. But what do we mean by it? There’s not a physical thing in the world, insomnia, that acts directly on another physical thing, fatigue. Rather, we mean that a lack of sleep causes the brain state that leads to the mind state of fatigue; in this case, insomnia and fatigue are not physical things but abstractions. If we want to help someone with insomnia, the most obvious way to intervene is not to determine the configuration of that person’s ion channels or which of their brain areas are underactive, but rather to help them figure out how to get some sleep. By extension, some researchers propose that understanding mood at the psychological level, such as how a person experiences rewards, punishments and surprises relative to their expectations and beliefs, will have the greatest impact. Likewise, they argue that the most effective treatments will also be deployed at that level, in the form of behavioral interventions, such as cognitive behavioral therapy, mindfulness and other forms of psychotherapy. This is what researchers are referring to when they describe depression as psychological, not biological. By this logic, mood is different from at least some types of memory impairment, because behavioral interventions, such as memory training, cannot halt the progression of Alzheimer’s disease.
An extension of this idea emphasizes the critical role that our environment plays in our mental health. We know that trauma and stress can trigger mood and other types of mental disorders, and that poverty and depression have a bidirectional, causal relationship. To that end, some argue that the most effective way to improve mental health will be through the social and environmental interventions that we already know work. Likewise, they argue that research into environmental causes and interventions is as important, perhaps even more important, than brain research. You might be surprised by some proponents of this position, including the neuroscientists Peter Sterling and Michael Platt and the former director of the National Institute of Mental Health, Thomas Insel.
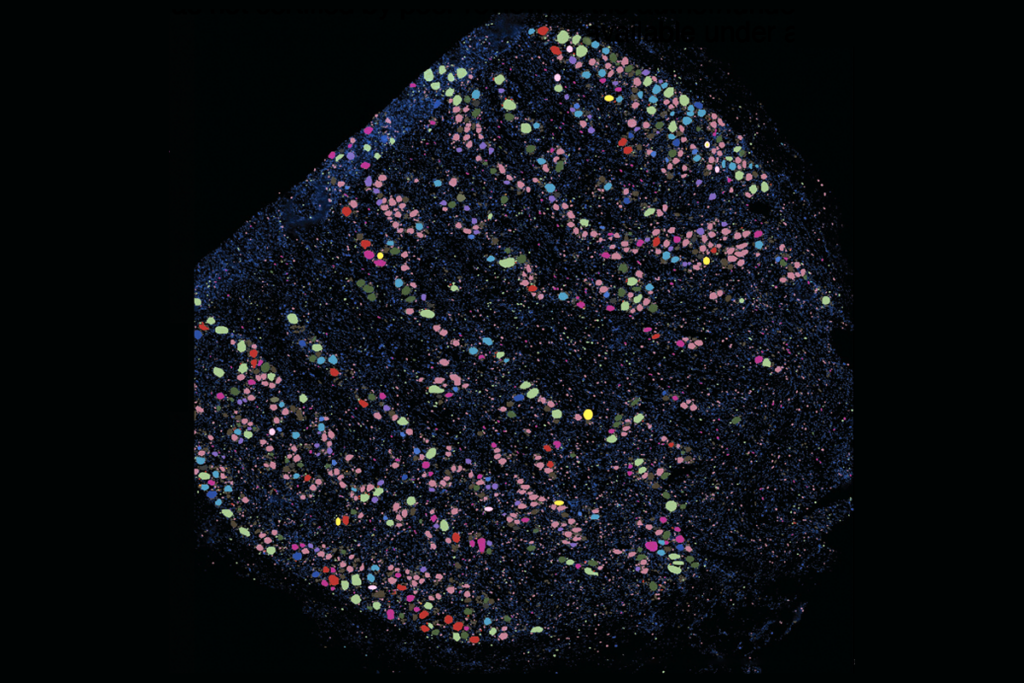
On the other end of the spectrum are those who argue that all mood disorders are brain disorders. Researchers who adopt this position acknowledge that, though environmental factors play a role, the same is true for people with memory impairment or even diabetes; in this view, memory is conceptually no different from mood. Advocates concede that, yes, of course, we should research the psychological and social factors that exacerbate these conditions, as we do for memory and diabetes research. But the bulk of our research efforts and dollars should focus on the biological phenomenon that mediates disease—in the case of diabetes, the pancreas and insulin; in the case of memory and mood disorders, the brain.
Some advocates of this position argue that because psychological variables are not physical—as in the insomnia “causes” fatigue example—it may be exceedingly difficult or impossible to establish cause and effect without investigating their physical correlates in the brain. Finally, advocates of this position point to evidence that brain- and body-based interventions, including antidepressants and exercise, as well as noninvasive and deep brain stimulation, work for at least some people with mood disorders. Given how little we know about mood in the brain, it only makes sense to do more research on mood in the brain to determine if we can improve upon the brain-based therapies that already exist.
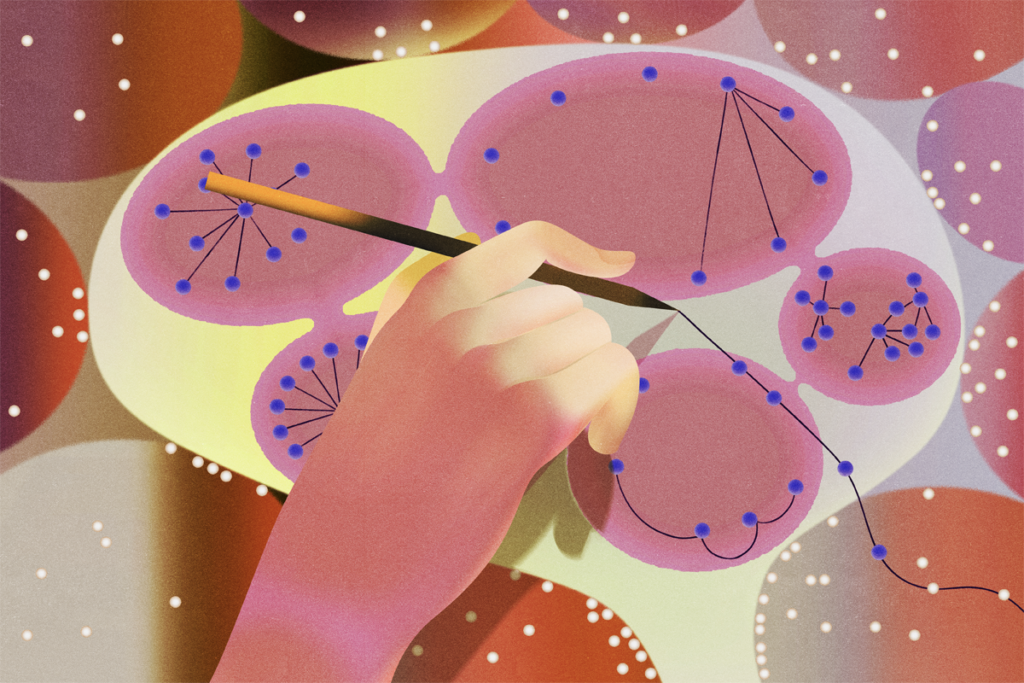
Many psychiatrists adopt a more nuanced position, in which the best level to explain the causes of mood and to target interventions for mood disorders depends on many factors, which can vary from person to person. For mood disorders, both medicine and behavioral therapies, most notably cognitive behavioral therapy, can be effective. By contrast, behavioral interventions are not effective for memory disorders to the same degree. And the most effective treatment strategy will differ for different people. Many who adopt this position advocate for more research at both the biological and psychological levels, and the interaction between the two, emphasizing the need to figure out how to predict the treatments that will work best for specific people.
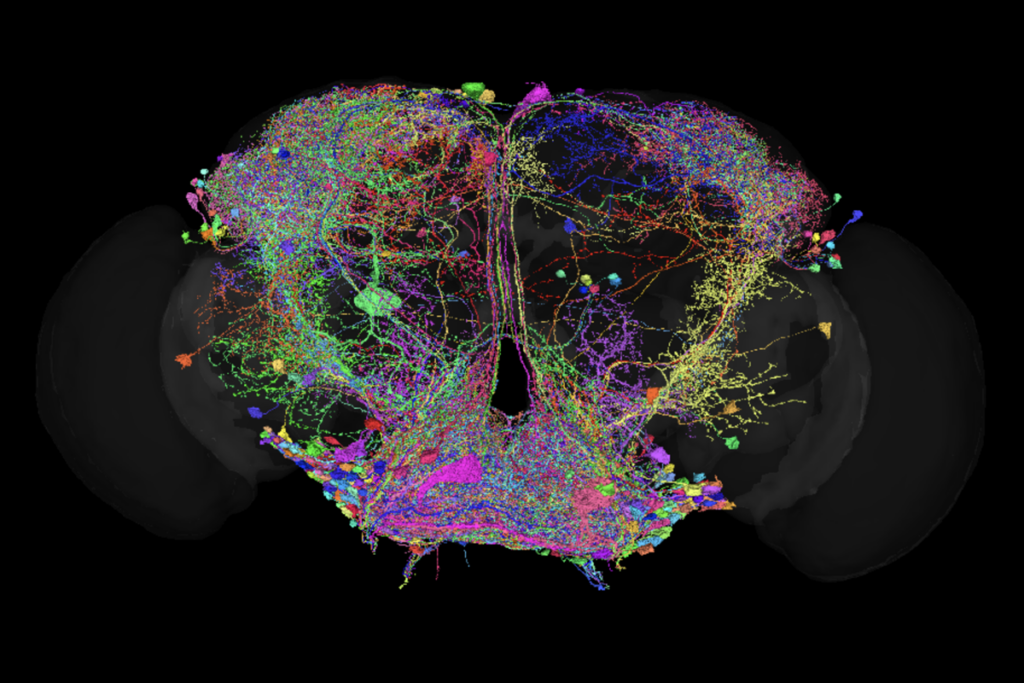
A final, more up-and-coming position draws from notions in physics, emphasizing the need to acknowledge that mood is an emergent property of a complex system. Proponents of this idea point to the innumerable feedback loops within and among the brain, the mind and the environment, and their parallels to other complex dynamical systems, such as the weather and ecosystems. They argue that because complex systems cannot be understood by deconstructing them into their parts, mood must be understood holistically and simultaneously across levels, applying what some call a biopsychosocial approach. Here, the gist is that interactions between the brain, mind and environment must be investigated simultaneously to understand mood and treat mood disorders. In complex systems with emergent properties, the properties of higher levels cannot be inferred from lower ones. Consequently, if mood is an emergent property of the brain, it cannot be understood by studying the brain alone. Similar ideas exist for memory, though they are less pervasive.
To better understand the different ways brain and mind researchers are thinking about this topic, I asked them: What do you see as the most effective path forward for mood research? How does it compare with the path forward for memory? I was struck by the diversity of these viewpoints, all rational but also quite different. All five of the perspectives I’ve just described (setting aside the sixth, a nonmaterial soul) are reflected in these responses.