Tangles of tau protein track with cognitive impairments in Alzheimer’s disease. But even though tau is expressed throughout the brain, it clumps mainly in specific regions, such as the cortex and hippocampus. Other areas, such as the cerebellum and brainstem, are largely spared.
Why tau aggregates this way has remained a mystery, but the answer may have to do with a previously overlooked, oversized and naturally occurring variant of the protein called “big tau,” according to a preprint posted 31 July on bioRxiv.
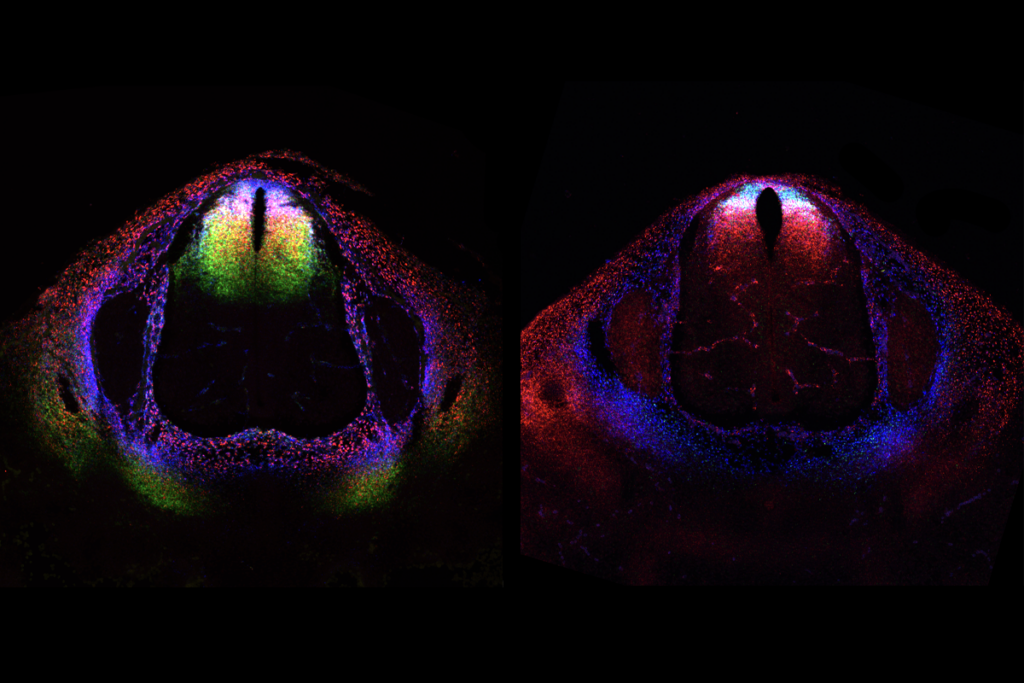
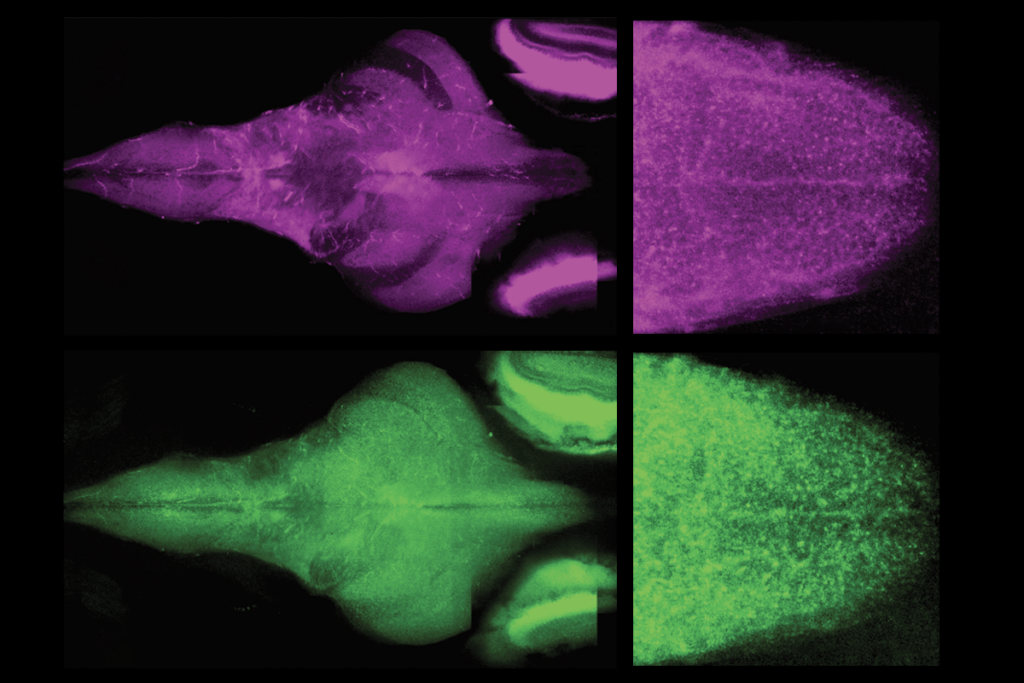
Most tau isoforms range from 352 to 441 amino acids in size, but big tau comprises 758 amino acids. This supersized version is significantly more abundant in the cerebellum and brainstem than in the cortex and hippocampus of mice—and it is much less likely to form abnormal clumps than its smaller counterparts, the preprint shows.
“Big tau can resist several key pathological changes related to [Alzheimer’s disease],” wrote study investigator Dah-eun Chloe Chung, a postdoctoral researcher in Huda Zoghbi’s lab at Baylor College of Medicine, in a post on X about the work. (Zoghbi declined to comment for this article because she says the study is currently under review for potential publication, and Chung did not respond to email requests for comment.)
Scientists identified big tau in the peripheral nervous system in the 1990s, and it is the predominant tau isoform there. But most research on tau since then “ignores the existence of big tau,” according to a 2020 review.
“No one has bothered to study this protein in the context of neurodegeneration,” says Veera Rajagopal, a research scientist at Regeneron, who did not take part in the new work. “All tau-related research has been focused on the shorter isoforms that play a key role in the tauopathies like Alzheimer’s disease, frontotemporal dementia and so on. Now many will go after this big guy.”
T
au normally helps stabilize the framework of microtubules within neurons. In Alzheimer’s disease, tau undergoes several chemical modifications, including the addition of phosphate groups, which cause it to detach from microtubules and form clumps.Big tau, by contrast, is less prone to gaining phosphate groups and binds more strongly to microtubules, Zoghbi and her colleagues found in experiments using mouse brain extracts and human cells grown in culture. It is more susceptible to the addition of ubiquitin tags, which target proteins for cellular destruction, and it breaks down far more rapidly than other tau variants, the study shows.
In addition, big tau is significantly less prone to clumping in live mice, further experiments suggested, even when the team engineered the mice to carry a mutation known to promote aggregation in regular tau.
When the scientists analyzed data from 124 people with Alzheimer’s disease collected in the Mayo RNAseq study, they confirmed that big tau levels were significantly higher in the cerebellum than in the cortex. This “may provide insight into why the cerebellum tends to be less affected by Alzheimer’s pathology than other brain regions,” says Andy Tsai, a postdoctoral scholar in Tony Wyss-Coray’s lab at Stanford University who did not participate in this study.
These new findings support earlier predictions suggesting that certain features of big tau could protect it from the kind of problems seen in Alzheimer’s, says Itzhak Fischer, professor of neurobiology and anatomy at Drexel University, who co-wrote the 2020 review paper on big tau but did not take part in the new study. “What was missing was an in-vivo confirmation and data from experimental models of degeneration, as well as supportive data from human tissue,” Fischer says. “These new findings provide that important new information.”
A
ll in all, the research highlights the importance of studying genetic diversity between brain regions and cell types in the context of disease, Rajagopal says. “The conventional approach is to compare the brains of diseased and normal individuals to understand disease-related biology. The study reminds us that we could also learn from comparing between brain regions and cells within a single brain.”These findings also showcase the starkly variable consequences that different isoforms can have in disease. “Ongoing efforts [from many groups] are expected to soon elucidate in detail how tau splicing regulation changes in the aging brain,” says Juyoun Yoo, a postdoctoral research scientist in Franck Polleux’s lab at Columbia University’s Zuckerman Institute who was not a part of the new study. “Studies on how these splicing events are regulated will be a very promising direction for not only understanding the etiology of the Alzheimer’s disease, but also developing therapeutic strategies.”
Future research can investigate a variety of open questions about big tau’s role in the brain and how it differs from smaller tau proteins, says Peter Baas, professor of neurobiology and anatomy at Drexel, who co-wrote the 2020 review with Fischer but did not work on the new study. For instance, “If big tau is protective against degeneration and accumulates in regions of the brain not afflicted by Alzheimer’s disease, why is it more readily degraded?” he asks. “How exactly is big tau prevented from aggregation and propagation? If the big-tau-specific sequence varies so much in different species, does the big tau in other species also have enhanced microtubule binding capacity? How did these properties of big tau evolve?”
Another key question these new findings raise is why the cognitive centers of the brain only express lower-molecular-weight tau if big tau could protect them against neurodegeneration, Baas says. “There must be certain advantages to lower molecular weight with regard to plasticity and cognition that other populations of neurons can sacrifice in favor of better protection against degeneration,” he suggests. “We need to understand this basic science question before we can risk applying lessons from big tau as therapy for degenerative diseases of the brain.”