
Why are there so few autism specialists?
A lack of interest, training and pay may limit the supply of specialists best equipped to diagnose and treat children with autism.
W
hen Natasha Marrus started her residency in general psychiatry in 2007, none of her 11 classmates ever mentioned autism. They eagerly discussed schizophrenia and bipolar disorder, and occasionally a “really tough” resident would talk up personality disorders, recalls Marrus, now a child psychiatrist at the Autism Clinical Center at Washington University in St. Louis, Missouri. But even those who were considering working with children did not share her interest in autism.Sarah Spence had a similar experience while training to become a neurologist in the 1990s. “My boss was thrilled I wanted to do autism, because nobody in neurology did this,” says Spence, co-director of the Autism Spectrum Center at Boston Children’s Hospital.
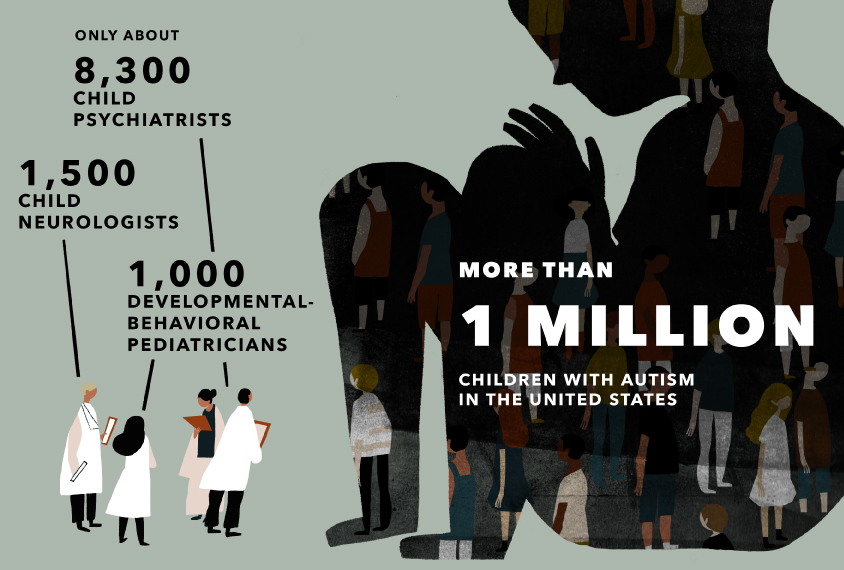
Decades later, both scientists are still in the minority: According to the latest estimates, there are more than 1 million autistic children in the United States but only about 8,300 child psychiatrists, 1,500 child neurologists and 1,000 developmental-behavioral pediatricians. And within those small numbers, autism remains an unpopular choice: “It’s not a perfect analogy, but I feel like autism within psychiatry is like psychiatry within medicine,” Marrus says.
These doctors are not alone on the frontlines of autism. Psychologists play a crucial role in screening for and diagnosing the condition, and some also provide behavioral therapy. But because autistic children frequently have additional psychiatric conditions, as well as physical ones such as epilepsy, frequent infections, sleep disorders and gastrointestinal problems, they benefit greatly from the medical expertise specialized pediatricians can offer.
Hard hit by the shortage are rural communities in the U.S., where many people with autism receive specialist medical attention only in an emergency, when a behavioral crisis has become too much for their families to handle. In South Dakota, for example, there is approximately one child psychiatrist for every 100,000 children under age 18.
The situation is no better elsewhere in the world. Regions such as North Africa, the Middle East and South Asia are home to the majority of children living with autism and intellectual disability, according to a report in The Lancet in August, but have few medical personnel qualified to care for these children. “This is a global problem, and the problem is much more pronounced in low- and middle-income countries,” says Rosa Hoekstra, senior lecturer in psychology at King’s College London.
Given the shortfall, many families join waitlists or travel long distances to see experts who have experience with autism. “The severe shortage is in treating the emotional and behavioral problems that come in the school-age population, 5 to 20 years old,” says Matthew Siegel, director of the Developmental Disorders Inpatient Research Collaborative at Spring Harbor Hospital in Westbrook, Maine. The average trainee in a child psychiatry fellowship program in the U.S. sees fewer than five people with autism or intellectual disability each year, according to a 2014 survey conducted by the American Academy of Child and Adolescent Psychiatry. Few get additional training, Siegel notes, in part because the American Board of Psychiatry and Neurology does not recognize specialties related to autism.
Siegel and his colleagues offer training and experience working with autistic children to more than 20 child psychiatrists each year, but they find it difficult to recruit enough fellows. And it is no easier to recruit staff to train them. Some 10 to 15 autism centers across the country are all seeking psychiatrists to work for them, he says. “There is no one to recruit; it took me a year and a half to find someone to join up here.”
”“The reality is we're not going to have specialists to see every child with autism.” Shafali Jeste
Show me the money:
P
art of what makes autism a daunting specialty is that working with autistic children demands a high level of skill and dedication. These children often have complex behavioral problems, plus a constellation of accompanying complications that are rarely solved with a quick prescription. A pediatrician could treat a typical child with an ear infection in 10 minutes but a developmental-behavioral pediatrician would need 40 minutes or more to follow up with an autistic child. Clinicians working with autistic children also often spend long hours helping families connect with community resources, such as school services, behavioral therapists and speech therapists — and they often must provide lifelong support rather than short-term solutions. “I think there are people who find that less fulfilling because you are not fixing [the condition],” Spence says.Working with autistic children is also often less lucrative than many other specialties. Most insurance companies readily reimburse doctors for procedures such as brain scans or surgery, but they are less likely to do so for time spent outside an office visit trying to connect an autistic child to the right speech therapist. “People who do behavioral work tend to have longer visits, and you don’t get reimbursed more for a longer visit per patient,” Spence says.
Autism clinics sometimes try to avoid wrestling with health insurers over reimbursements by only accepting cash payments. But many families cannot afford that option, and so it narrows even further the pool of experts available to them, says Shafali Jeste, director of the Care and Research in Neurogenetics Clinic at the University of California, Los Angeles. Jeste’s center does accept health insurance, but it is also partly supported by funding for autism research. “It’s very difficult to build a model of billing that doesn’t lose money,” she says. “Our reimbursement rate is abominable; we’re basically doing services for free.”
Because autism specialists typically don’t bring in as much money as other specialists do, they also tend to command lower salaries. Developmental-behavioral pediatricians complete three years of extra training after their pediatrics residency, yet they typically earn the same as or less than primary care physicians, says Leonard Rappaport, chief emeritus of the developmental medicine division at Boston Children’s Hospital.
Foregoing a higher salary is not an easy choice when the average 2016 medical school graduate left with $190,000 in debt. “We would see people in the general-psychiatry residency who were interested in working with [autistic] kids,” Marrus says. “But they decided, ‘You know what, I have a life to lead … I want to pay my debts now because I’m having kids and expenses are getting high.'”
The U.S. government offers loan repayments to medical students who agree to spend several years working in regions of the country that have too few physicians. Some experts have suggested expanding those programs to include doctors who pursue autism and other developmental conditions. “By doing loan repayment, you stand a chance that you can then draw in a whole other group of people who would like to do it but can’t face the debt issue,” Rappaport says.
Swelling the ranks:
A
utism specialists are trying to swell their ranks by giving child psychiatrists, child neurologists and developmental-behavioral pediatricians access to training.Siegel, Marrus and others are developing a series of nine video lectures as part of their efforts on the American Academy of Child and Adolescent Psychiatry’s Autism and Intellectual Disability Committee, which oversees training for these conditions. Once the series is ready to distribute, which may be sometime next year, the committee plans to redo the 2014 survey of psychiatry programs. They then aim to track any improvements the videos bring about, including the number of related training hours in residency programs. “Our thought was if you at least increase training, you’d have the newer generation of psychiatrists who don’t have that inertia [toward autism] as likely because they would be more comfortable,” Marrus explains. “You’d increase your supply of doctors.”
To extend autism training to child neurologists, some residency programs have started to offer a specialization in neurodevelopmental conditions. Without that sort of training, child neurologists may not be prepared to handle behavioral problems, Jeste says. Instead, they focus only on conditions that often accompany autism, such as epilepsy. “We need [autism] specialists; we need to train the next generation,” she says.
Among developmental-behavioral pediatricians, the problem is less about training and more about numbers. A survey in March found that the current number of trainees will not replace the number of physicians with this specialization who plan to retire in the next three to five years. “Most people in [this] workforce have the appropriate expertise to diagnose and offer treatments [for autism], whether it’s the mental aspects or medication,” says Carolyn Bridgemohan, a developmental-behavioral pediatrician who co-directs the Boston Children’s Hospital Autism Spectrum Center with Spence. “The problem is not enough people in the workforce.”
Since 2000, the nonprofit that sets medical-education standards has made developmental-behavioral pediatrics a required rotation in pediatric residencies in an effort to attract more people to the field. The staff at Boston Children’s Hospital plan to offer residents in this rotation a series of autism-related behavioral simulations. The staff and hired actors mimic common hospital procedures that can be stressful for an autistic child, from routine blood-pressure checks to placing electrodes for an electrocardiogram. “You put the hospital staff through the simulation of behavioral escalation, and they practice de-escalation techniques so that they can figure out a way to get a medical procedure done in an easier way for the patients,” Spence says. “There is a major focus on experiential learning.”
The hospital’s developmental-behavioral pediatrics program fills every year, and the program officers are fortunate to be able to recruit the top residents in the incoming group. “We had [eight] good applicants this year, but every program in the country is trying to get those eight applicants,” Rappaport says. Before he stepped down as chief, Rappaport says he fielded weekly requests for developmental-behavioral pediatricians from other medical centers around the country — another measure of how supply falls far short of demand.
”“The severe shortage is in treating the emotional and behavioral problems that come in the school-age population.” Matthew Siegel
Widening the circle:
F
or some children on the spectrum, it takes more than one autism specialist to help them out of a behavioral crisis. Estimates suggest that 11 percent of autistic children are admitted to a psychiatric hospital at least once before adulthood — often after months or years of not getting the right kind of care.For instance, when 7-year-old Alana arrived at Maine’s special hospital unit for children with autism in 2012, she was either biting her hands or smacking her head more than 100 times a day. (Spectrum is withholding Alana’s last name to protect her privacy.) Her self-harm, along with tantrums and aggressive behavior, had increased sharply over the preceding two months — and she was exhausted; she had been staying awake for several hours every night.
A slew of medications, including antipsychotics, antidepressants and sedatives, and frequent home visits from various therapists had all failed to help. Nor had she improved after a brief stay in the children’s unit of a general psychiatric hospital. Out of options, her in-home services supervisor referred her to the Spring Harbor Hospital Developmental Disorders Unit. The unit is home to a team of veritable medical superheroes: child psychiatrists, pediatricians, behavioral psychologists, physician assistants, occupational and speech therapists, social workers, nurses and special-education experts.
Over the course of about a month, the team brought Alana’s harmful behaviors back under control. They weaned her off of sedatives, easing her irritability and boosting her alertness, and devised a regular sleep routine for her. They also diagnosed her with generalized anxiety disorder and constipation, both of which had gone unnoticed and contributed to her distress. And they crafted a positive behavioral support plan, involving visual cue cards and her favorite toys, to help her when she went home. Alana lives too far from the hospital to use their outpatient services, but she has never been readmitted.
Many centers are testing ‘telehealth’ technologies as a means to assemble wide-ranging teams of experts like the one at Spring Harbor. As part of that drive, Autism Speaks, a New York-based advocacy organization, has established Extension for Community Healthcare Outcomes Autism, or ECHO Autism, a network of hospitals and clinics. Primary care clinics consult by video conferencing with panels of autism experts at academic medical centers. Each panel includes a pediatrician, psychologist, psychiatrist, dietician, social worker and a parent of a child with autism.

In September 2018, Project ECHO Autism announced an expansion of its network of academic medical centers from 14 to 24 sites across the U.S. and Canada. One of the centers, Cincinnati Children’s Hospital Medical Center in Ohio, works with Adams County Regional Medical Center, a smaller facility in southern Ohio with no autism specialists on staff. “We’re using telemedicine connections into rural Ohio as a first step to improving access,” says Craig Erickson, director of research at the Kelly O’Leary Center for Autism Spectrum Disorders at the Cincinnati center. “We would rather treat you with telemedicine chronically than have you arrive in crisis.”
Experts could also tap telemedicine to make better use of their time and resources. They could train local physicians to conduct basic exams and screening, and to diagnose comorbid conditions such as gastrointestinal problems and insomnia. They could also offer consults on complex issues via video conferencing. “My goal is that we might have these clinics everywhere, partly run through telehealth,” Jeste says. “The reality is we’re not going to have specialists to see every child with autism.”
Compared with when she was a resident nearly a decade ago, Marrus says more medical students are pursuing child psychiatry and autism. Some of that increase may reflect autism’s rising prevalence and the growing numbers of autistic children in clinics and hospitals. More trainees also now say they are interested because they have family or friends with the condition. It’s still not nearly enough but, Marrus says, “it’s a long game.”
Corrections
This article has been modified from the original. A previous version incorrectly implied that psychologists cannot diagnose autism.
Recommended reading

Too much or too little brain synchrony may underlie autism subtypes

Developmental delay patterns differ with diagnosis; and more
Explore more from The Transmitter

This paper changed my life: Shane Liddelow on two papers that upended astrocyte research
Dean Buonomano explores the concept of time in neuroscience and physics

