What Ehlers-Danlos syndrome can teach us about autism
Not much is known about the connection between autism and Ehlers-Danlos syndrome, a condition that affects collagen. But preliminary work provides tantalizing clues.

As an autism researcher interested in rare genetic syndromes, I have always found my grandmother fascinating. She had subtle but distinctive facial features, as well as epilepsy and learning difficulties. But I have never been able to work out what syndrome, if any, she might have had.
I wrote about her unusual traits on my blog in 2014 — and a reader responded, suggesting that my grandmother might have had Ehlers-Danlos syndrome. I didn’t think much of the suggestion at the time because I had done a lot of digging and this condition had never come up.
But as I continued to communicate with the reader, I realized that many of the features she mentioned in fact described me: I have chronic pain and am double-jointed in most of the major joints of my body, for example.
The conversation spurred me to see my doctor, who referred me for an assessment at Greenwood Genetic Center in Greenville, South Carolina, where I live.
Ehlers-Danlos syndrome and related conditions are thought to stem from problems with the formation and repair of collagen, the glue that holds the body together.
Because of this, people with these conditions are often hypermobile (double-jointed), have stretchy, delicate skin, immune disorders and sometimes heart problems. They often experience severe chronic pain related to joint dislocations, partial dislocations and excessive inflammation. Some require numerous surgeries and may have to use mobility devices by their teenage years.
Official estimates suggest that 1 in 2,500 to 5,000 people have the condition, but most clinicians agree these estimates are outdated. And the symptoms are nebulous enough that the frequency may be significantly higher.
Although I’m still awaiting genetic testing to rule out other hereditary connective-tissue disorders, my physical exam suggests I have a condition closely related to Ehlers-Danlos called generalized hypermobility spectrum disorder. After my diagnosis, I joined online communities for people with these conditions and began to learn more.
I noticed numerous posts asking about Ehlers-Danlos’ overlap with autism. It was as if the scientific stars had aligned and gifted me an important new question: Are Ehlers-Danlos syndrome and autism related? And, if so, could the biology of Ehlers-Danlos teach us something about the biology of autism?
Connected conditions:
The literal and figurative connection between the two conditions may lie in collagen.
Collagen has an important role in the developing brain. It is abundant in the membrane enveloping the brain and spinal cord1. In a typical embryo, radial glia cells — a form of neural progenitor cell — attach to the membrane like a scaffold. If the cells cannot attach properly because of problems with collagen, that could disrupt brain development2. This is just a hypothesis, however.
Another possibility lies in the immune conditions that frequently affect those with Ehlers-Danlos. Autism is also linked to problems with the immune system: Maternal immune disorders or infection during pregnancy are linked to autism risk in the child, for example. I think a similar relationship may exist in Ehlers-Danlos syndrome.
In 2016, I started to look for data to address these ideas — but I found few studies linking autism and Ehlers-Danlos. Aside from a few case reports, only a single Swedish study had investigated their co-occurrence: It estimated that 3 percent of people with Ehlers Danlos also have an autism diagnosis3. But because most people with Ehlers-Danlos are women, and women are notoriously underdiagnosed with autism, I suspect the overlap is much greater. The same trend may be true of generalized hypermobility spectrum disorder.
My colleagues and I started our scientific journey by conducting a small online survey of autistic women, 85 with and 20 without generalized joint hypermobility (defined as hypermobility in five or more joints)4. We asked them questions about their immune and hormone function. We found that autistic women with generalized joint hypermobility are more likely than those without it to have co-occurring immune and hormonal conditions such as asthma, allergies, diabetes and polycystic ovary syndrome.
In a second survey of more than 700 people, we compared adults with Ehlers-Danlos syndrome and generalized hypermobility spectrum disorder (with or without autism) with those who have autism (without hypermobility) and those with neither condition5. We surveyed a wide variety of issues, including joint dislocations, tendency to bruise, chronic pain and cardiovascular problems.
Perhaps unsurprisingly, the Ehlers-Danlos group had the most health problems, followed by the people with autism. But to our surprise, the autism group also reported high rates of problems related to connective tissue (easily bruised skin, for example) as well as chronic pain.
We also found that approximately 20 percent of mothers in the Ehlers-Danlos group have autistic children, and that these women have more immune-related problems than Ehlers-Danlos mothers without autistic children. We strongly suspect the mothers’ immune disorders play a role in the children’s autism.
Top priority:
We are in the midst of our first clinical study, and we hope to recruit at least 150 people. We are comparing features of Ehlers-Danlos syndrome in two sets of women: those who have autistic children and those who have children with attention deficit hyperactivity disorder (ADHD). We test the mothers’ joint mobility and orthostatic tolerance (the cardiovascular system’s ability to adjust to changes in body posture). We also ask them about their immune, hormonal and other health issues, and assess their autism traits.
Our preliminary results are tantalizing: They suggest that rates of generalized joint hypermobility do not differ between the two groups, but the mothers of autistic children have more hypermobility overall and experience far more pain and musculoskeletal impairment. We plan to add a control group later this year to see whether these problems are more common in families with autism or ADHD than in controls.
We need to probe the underlying biology of these conditions to tease out whether Ehlers-Danlos in the mother contributes to autism in her child. We also need accurate prevalence estimates for Ehlers-Danlos syndrome and generalized hypermobility spectrum disorder before we can pin down their prevalence among autistic people.
There is growing interest in hereditary connective-tissue disorders within the autism community because they can so debilitating. In fact, the link between hypermobility-related disorders and autism was one of the major research priorities proposed by the adult autistic community attending the 2019 annual meeting for the International Society for Autism Research. (You can read more about this via the Twitter hashtag #AutINSAR.)
Thankfully, my condition does not leave me so disabled that I cannot work — although I do require some minor accommodations. But many people with these conditions are not so lucky. So I feel it rests partly on my shoulders to advocate for this population. After all, who else would fight as hard as a scientist who has the same condition?
Emily Casanova is research assistant professor of biomedical sciences at the University of South Carolina School of Medicine in Greenville.
References:
Recommended reading

Common and rare variants shape distinct genetic architecture of autism in African Americans
Explore more from The Transmitter
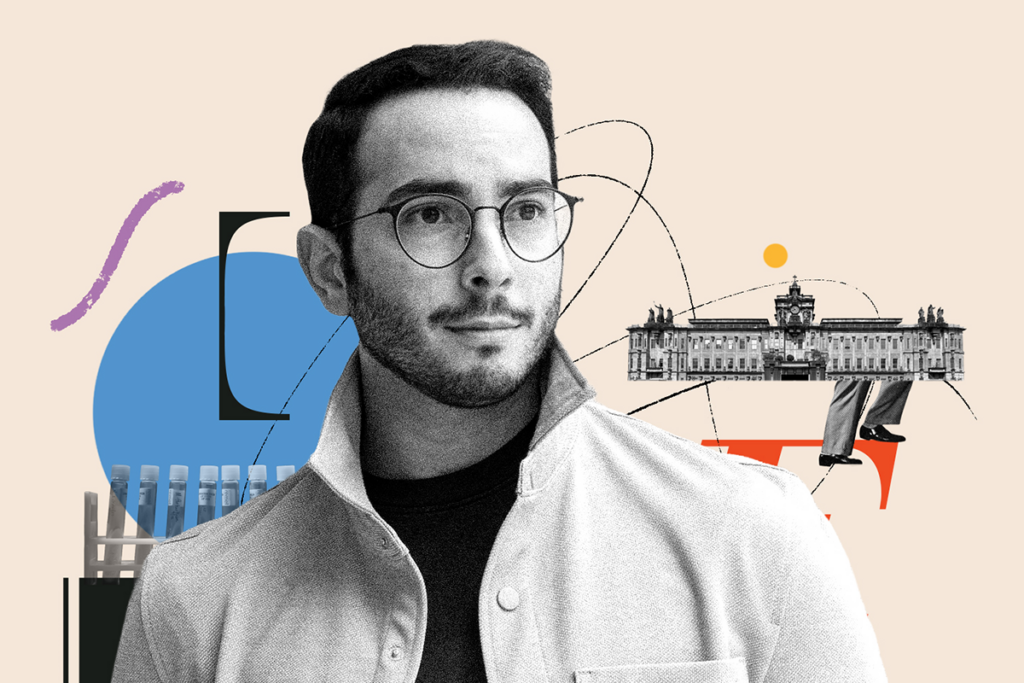
Frameshift: At a biotech firm, Ubadah Sabbagh embraces the expansive world outside academia