What baby siblings can teach us about autism
Studies of infants at risk for autism have not yielded a test to predict who will eventually be diagnosed. But they have transformed our understanding of the condition.
I
n October 2010, Lisa and Eugene Jeffers learned that their daughter Jade, then nearly 2 and a half years old, has autism. The diagnosis felt like a double whammy. The parents were soon engulfed by stress from juggling Jade’s new therapy appointments and wrangling with their health insurance provider, but they now had an infant son to worry about, too. Autism runs in families. Would Bradley follow in his big sister’s footsteps?“We were on high alert,” Lisa Jeffers says. “There were times I would call his name, and he wouldn’t look.” She says she couldn’t help but think: Is it because he’s busy playing or because he has autism?
In search of guidance, the parents signed Bradley up for a three-year study at the University of California, Davis (UC Davis) MIND Institute, a half-hour drive from their home near Sacramento. Researchers there wanted answers to some of the same questions the couple had: What are the odds that infants like Bradley — younger brothers or sisters of a child with autism — will be on the spectrum too? Could experts detect autism in these babies early on, so that they might benefit from early intervention?
The infant-sibling study at UC Davis is one of more than 20 similar long-running investigations across the United States, Canada and United Kingdom, the first of which began around 2000. These ‘baby sib’ studies, which collectively have followed thousands of children, are among the most ambitious and expensive projects in autism research. Many of the scientists who run them anticipated that by tracking this special population, they would be able to spot signs of autism before age 1, and ultimately create an infant screen for the condition.
Obtaining clear answers from baby sibs, however, was far more difficult than expected, with many false starts along the way. Autism revealed itself to be an incredibly complex, heterogeneous spectrum of developmental conditions whose hallmark characteristics emerge over time — unfolding along different trajectories in different babies. All of which made it harder to pinpoint the earliest signs.
Earlier this year, researchers saw new glimmers of hope. Two major findings emerged from investigators in the Infant Brain Imaging Study (IBIS), who took brain scans of more than 300 baby sibs during their first two years of life. In February, one report from the $20 million project described an unusual pattern of brain growth during infancy that forecasts an autism diagnosis. Earlier this month, the IBIS team and their collaborators at UC Davis confirmed a previous observation that a surplus of cerebrospinal fluid at 6 months of age also predicts an autism diagnosis.
These two indicators may be the best leads so far for identifying autism in infancy, but the investigators aren’t declaring victory just yet. “We’re not saying somebody should run out and do this just because we published this paper,” says Joseph Piven, who directs the IBIS project. “This is really just the first step along a long path.”
In other words, after more than 15 years of effort, the ultimate dream of a predictive test that could be used routinely in the clinic is still being worked out.
“The answers are just not going to be that simple for us in autism,” says Helen Tager-Flusberg, director of a baby sib study at Boston University, though she notes that the field is moving rapidly. Given autism’s complexity, it’s unlikely there will ever be any single early predictor for it, she says, although researchers may one day discover a combination of prognostic indicators. She points out that extensive efforts to find predictive tests for adult brain conditions, such as schizophrenia and Alzheimer’s disease, haven’t panned out yet either.
In the meantime, though, the baby sibling research field has produced hundreds of scientific reports and some groundbreaking insights into brain development. And, as often happens in science, a big lesson researchers learned was that some of their assumptions were wrong. “The whole experience has really been quite humbling, and has given us a greater appreciation of both the developmental nature of autism and the heterogeneity in autism,” says Lonnie Zwaigenbaum, an early pioneer in the field.
”“The baby sibling approach currently is the only real way you can get information about autism starting from the early stages of development.” Karen Pierce
Humbling lesson:
T
he rationale for studying infant siblings was compelling from the start. Around two decades ago, analyses of parent interviews suggested that most children who have autism are born with some telltale traits. Many parents said they remembered early signs of autism, sometimes well before their child’s second birthday — and long before a diagnosis, which in the U.S. now is typically not until age 4. Researchers wanted to close that gap.Rather than rely on parents’ memories — which, like all human memory, can be notoriously unreliable — the scientists realized that a more accurate approach would be to track children from birth. But because at that time less than 1 percent of children in the U.S. were estimated to have autism, such an experiment called for monitoring thousands of babies for years, a prohibitively costly and inefficient prospect. So instead, researchers chose to fish in a smaller pond: among the brothers and sisters of diagnosed children, 3 to 10 percent of whom had been estimated to also have the condition. (Baby sib studies from the past several years peg the rate at closer to 20 percent.)
“The baby sibling approach currently is the only real way you can get information about autism starting from the early stages of development,” says Karen Pierce, co-director of the Autism Center of Excellence at the University of California, San Diego, who investigates autism screening but isn’t involved in the baby sib studies. “There’s no other way to really do that.”
In 2003, two research teams in the U.S. and Canada formed the Baby Siblings Research Consortium (BSRC) to share their ideas and unpublished data. Others soon joined. Many investigators hoped the first studies, which focused mostly on social behavior, would nail down signs of autism in the first year of life. They thought they would be able to identify the sibs with autism even as early as 6 months of age, says Sally Ozonoff, who launched the infant sib initiative at UC Davis. There was a “bit of hubris” at the beginning, she recalls with a wry chuckle. “We thought we would just be able to tell.”
Two or three years in, the teams were coming up empty-handed. They saw no hints of autism in the social interactions of children younger than 12 months old. Against expectation, infant sibs who were diagnosed with autism at age 3 looked just like typically developing infants in their first year. Any red flags — from poor eye contact and repetitive behaviors to failing to respond to one’s name — surfaced only in the second year, or sometimes even later. That lag was discouraging from a screening perspective, but it also led to a scientific revelation: Most of the children seemed to lose social skills they had already developed.
The findings drove home that autism is, after all, a developmental condition. “It emerges at different times for different children,” Ozonoff says. “That was really surprising, early on.”
As a case in point, Bradley Jeffers initially seemed to be on track: He was an extremely social baby who flirted with and smiled at grownups. But at around 16 months, he started flapping his hands a little and would say a new word (like ‘moon’) only once and never repeat it, much as his sister had done. Concerned, Lisa Jeffers mentioned it to Ozonoff’s team at his 18-month-old research visit at UC Davis. But that day, he still scored below the threshold for an autism diagnosis.
Three months later, Bradley began fixating on fur and feathers — for example, throwing a dyed feather in the air over and over while jumping up and down. Shortly thereafter, in April 2012, he was officially diagnosed with autism. Within months, he began receiving applied behavioral analysis therapy, and soon his eye contact improved, as did his ability to respond to instructions, his mother says. But now, at 7, he still retains characteristics of autism. He often runs back and forth repetitively, gazing at his fingers, which he holds out in front of his face. He has struggled with schoolwork and acted out in class.
The next hunt:
A
fter the quest to find early behavioral markers had stalled, baby sib investigators shifted gears, expanding their focus on the biology of the developing brain. Around a decade ago, several innovative labs adapted methods such as magnetic resonance imaging (MRI), electroencephalography (EEG) and near-infrared spectroscopy to monitor brain structure and function in baby sibs. Those teams and a few other groups also experimented with eye-tracking technology to look for fine-grained differences in children’s visual reflexes, which reflect brain maturation and functioning.Those efforts began mapping out changes in the brains of babies headed for an autism diagnosis. By 2012, a U.K.-based consortium called the British Autism Study of Infant Siblings (BASIS) had discovered that the brains of baby sibs diagnosed with autism at age 3 show a different pattern of responses to another person’s gaze when the children are between 6 and 10 months old, compared with typically developing babies. The following year, eye-tracking studies uncovered additional impairments before age 1 in attention to stimuli such as faces and eyes.
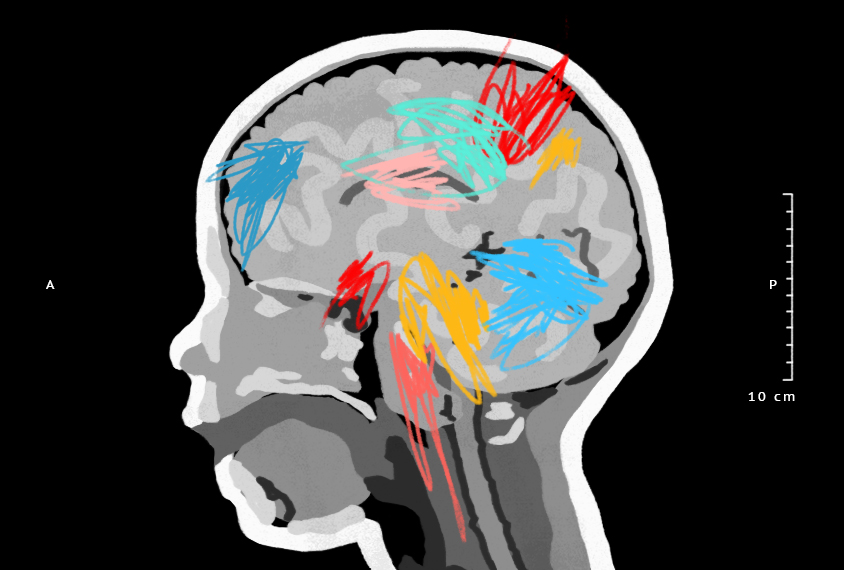
Around the same time, the IBIS investigators observed changes in brain structure that occur in parallel with those functional differences. Researchers at four U.S. sites used identical MRI protocols to scan the brains of 318 infant siblings at 6, 12 and 24 months. A 2012 analysis on a subset of 92 of the siblings revealed that between 6 and 24 months of age, the babies who were later diagnosed with autism show a different growth pattern in the microstructure of nerve fibers that link various brain regions — connections essential for transmitting neural signals across the brain.
These findings introduced a theme that studies from multiple labs have since repeatedly reinforced: Babies who are later diagnosed with autism begin to diverge from typical brain development between 6 and 12 months of age. The signature seems to be a pattern of brain differences that unfolds in unusual ways over time — a concept underscored by the IBIS findings reported last February in Nature. MRI scans from 15 baby sibs diagnosed with autism at 2 showed an abnormally rapid expansion of the brain’s surface area, most noticeably in the visual regions, between 6 and 12 months — followed by an acceleration in overall brain growth between 12 to 24 months, just when social difficulties emerge. By training a computer algorithm to flag the rapid first-year growth pattern, “we got a strong suggestion that before the onset of symptoms, we can actually predict autism,” Piven says.
However tantalizing, these results are preliminary, and weakened by a problem that plagues most baby sib investigations: sample size. Even though this special population is more likely to develop autism than average, the condition is still rare. If you follow 100 baby sibs, fewer than 20 might develop autism. To create a sensitive, accurate test, any promising detection method would need to be assessed in much larger numbers of infants, in different groups of children and by independent teams.
Such replication studies are rare and hard to do, but they are starting to happen. Four years ago, for instance, a small study at UC Davis found that increased levels of cerebrospinal fluid in 6-month-olds track with a later autism diagnosis; the study’s 55 participants included 33 baby sibs, 10 of whom were subsequently diagnosed with autism. In a report this month, the IBIS network arrived at the same result in a separate, larger group of 221 baby sibs, with 47 identified as having autism by age 2. An excess of cerebrospinal fluid is one of the few potential early autism biomarkers to be independently verified so far, but its predictive accuracy still isn’t high enough for it to function as a screen.
Confirming the MRI results of the IBIS study published in Nature, meanwhile, would require either an independent study with hundreds more children or an exact replication of the earlier IBIS protocols — with pre-registered methods for analysis to avoid bias after the fact, says neuroscientist Tal Yarkoni of the University of Texas at Austin. Given the small number of baby sibs with autism in the original IBIS report, the brain’s complexity and the “degrees of freedom” in how scientists analyze MRI data, those findings could be a product of random chance, Yarkoni says. Even if a replication study pans out, he adds, the whole effort would need to be repeated in an even larger population to generalize the results to all baby sibs.
IBIS investigators aim to conduct a follow-up replication study, but Piven says it’s challenging to obtain funding for brain scans in several hundred babies — a problem other imaging studies face, too. Major replication efforts are also already underway in Europe to try to reproduce key findings of small, exploratory MRI and eye-tracking studies from the BASIS project.
Still, there are several reasons MRI studies may not yield a practical test for babies in the general population. First, as the researchers themselves acknowledge, the very idea of using brain scans to screen for autism is a tough sell — they’re expensive, and babies and toddlers must be sedated or trained to fall asleep in the scanner so that they lie still while the images are taken.
In addition, it’s unknown whether some of the unusual brain-development patterns seen in autism may also arise as a result of attention deficit hyperactivity disorder, intellectual delays or other developmental conditions that commonly accompany autism. And even if a method predicts autism in baby sibs, there’s no guarantee that it would work in other infants; there are hints that the siblings differ in fundamental ways from the overall pediatric population.
Doing the legwork to learn whether infant sib findings are generalizable is “an essential priority,” Zwaigenbaum says. “Broader society [should benefit] from this investment, rather than only families where there’s already a child with autism.”
At this stage, routine detection of autism in the first year of life doesn’t seem likely to happen any time soon. Given that reality, some researchers say the field’s emphasis on spotting autism early was misguided.
“The hope or the hype was that we would have these ‘litmus tests’ that would tell us who has autism later and who doesn’t,” says Mayada Elsabbagh, former scientific coordinator for BASIS, who is now at McGill University in Montreal. In her view, that particular promise, amplified in press releases and media coverage, was doomed to disappoint.
”“The whole experience has given us a greater appreciation of both the developmental nature of autism and the heterogeneity in autism.” Lonnie Zwaigenbaum
New basics:
E
ven though the hunt for a litmus test has been frustrating, baby sib research has delivered unexpected payoffs, including a wealth of knowledge about how brain development in autism diverges from typical paths. The investigations have “really opened a new frontier in understanding early brain structure and function in autism and how it might relate to later symptoms,” says Zwaigenbaum, chair of the BSRC.The consortium has also created an unprecedented data resource. Its two dozen principal investigators pool behavioral and cognitive measurements on infant siblings in a centralized database, which now includes records of 3,300 baby sibs and 1,600 infants from families with no history of autism. It is the largest cohort worldwide of children with an elevated risk of autism. (The advocacy group Autism Speaks, which funded the project for many years, declined to renew support in 2017; an emergency grant from the nonprofit Autism Science Foundation keeps the database alive.)
Each baby in the database represents not just hundreds of hours spent by scientists in intensive assessments and data-processing, but the goodwill of a family. Parents bring a child in for as many as seven visits between 6 months and 3 years of age, with each evaluation lasting anywhere from two to five hours. Because every infant sib has an older brother or sister with autism, squeezing these research visits into family schedules takes effort. “It’s a huge burden on the families,” Tager-Flusberg says. “We’re really asking a great deal of them.”
Lisa and Eugene Jeffers can attest to that. They took their son Bradley to UC Davis for detailed assessments every few months — and signed him up in late 2010 for the MRI study that found the cerebrospinal fluid marker. That study involved much more than just showing up for the brain scans. At least two weeks before the first imaging test, the investigators gave the family a recording of the MRI machine’s noises to help condition Bradley to sleep during the scanning process. The week before the appointment, the parents kept their chubby, hyperactive son busy by day — with no naps — and played the recording on full volume at night, praying he would conk out at bedtime. The protocol paid off at his first MRI visit at 6 months old: Bradley slept through more than an hour of scanning.
Baby sib research has also provided valuable answers for the Jeffers family and other families and their clinicians. The studies confirm that younger siblings of children with autism are indeed at an elevated risk: Pooled analyses from the consortium in 2011 and 2015 indicated their odds of having autism is as high as 20 percent. And a large consortium study determined that standard screening tools can reliably pick up autism as early as age 18 or 24 months in siblings who show classic warning signs, such as a lack of gestures or an intense fixation on objects. That’s a significant advance, because most doctors consider an autism diagnosis before age 2 to be unreliable and often won’t start treatment until it’s confirmed, Ozonoff says. “There’s no need to wait,” she says.
More lessons are on the horizon, too. For example, one popular scientific theory held that brain areas for social communication are impaired from day one in children with autism. But it’s now evident that these disruptions don’t emerge until a few months after birth, and that they hit multiple systems, ranging from visual attention to motor coordination, says Mark Johnson, a leader of the BASIS project. Researchers are trying to uncover how these changes consolidate into hallmark social difficulties; perhaps autism traits result from the ways in which the brain compensates for the disruptions, Johnson proposes. Other ideas to explore include Piven’s speculation that an early proliferation of precursor cells leads to rapid expansion in brain surface, and that excessively fast development may be detrimental for maturing neural circuits.
The baby sib findings also suggest that the earliest interventions may prove most successful. Because scientists have no way of knowing in the first year which siblings have autism, they can design early therapies to benefit all of them, Elsabbagh says. Along these lines, the BASIS team has created a home-based program to teach parents to modify their social interactions with their babies. A small randomized controlled trial of the intervention in 2015 showed modest benefits in 7-to-10-month-old infant sibs, indicating “that we are able to shift these risk signs [for autism] very early on in development,” Elsabbagh says.
Another possibility, she notes, is personalized medicine: By combining data on a child’s family background and environment with genetic, behavioral and brain biomarkers, experts might be able to stratify infant sibs into risk categories and tailor therapies.
None of these ideas paid off soon enough to help the Jeffers children. Lisa Jeffers grapples with angst over whether Bradley could have been diagnosed a few months sooner. Yet she still firmly believes in baby sib research. Before their son’s diagnosis — while Lisa Jeffers was pregnant with their third child, Raona — she and her husband enrolled that baby in yet another study. Raona, too, was later diagnosed with autism. With that third diagnosis, Lisa Jeffers says, “it was like someone ripping your heart out and stomping on it.”
The UC Davis team diagnosed Raona at 19 months, before her parents recognized the signs, and she started therapy when she turned 2. She has done so well that now, at age 5, her autism often isn’t obvious to a casual observer.
Having access to experts when she had questions or worries about her children was invaluable, Lisa Jeffers says. And though it may be many more years before baby sib studies yield greater clinical benefits, she would do it again, “if it even just helped one family to get therapy sooner,” she says. “The more people that are involved, the more the researchers are going to be able to understand about autism.” Last March, she browsed the UC Davis website for other studies to which her children, now school-aged, could contribute.
Syndication
This article was republished in Scientific American.
Recommended reading

Among brain changes studied in autism, spotlight shifts to subcortex
Home makeover helps rats better express themselves: Q&A with Raven Hickson and Peter Kind
Explore more from The Transmitter

Frameshift: Shari Wiseman reflects on her pivot from science to publishing

How basic neuroscience has paved the path to new drugs