Some researchers suspect that clues to autism’s origins lurk in the mitochondrial genome, a ring of 37 genes that control our cells’ ability to create energy. However tantalizing that idea may be, though, it’s difficult to prove, in part because many strategies for sequencing and editing the nuclear genome don’t work on mitochondrial DNA (mtDNA).
A suite of new tools that can find and edit disruptive mtDNA mutations may fill that gap, however, making the mitochondrial genome more accessible for autism researchers.
One such tool, called STAMP (Sequencing by Targeted Amplification of Multiplex Probes), debuted in 2020 and can identify mutations that arise in only some copies of a cell’s mtDNA, a situation known as heteroplasmy. At least one heteroplasmic mutation has been identified in people with autism, and the mutations contribute to the condition in about 3 percent of autistic people, according to a forthcoming analysis that uses STAMP.
“It’s really exciting to see the recent expansion of the mtDNA toolbox,” says Nicole Lake, a postdoctoral researcher in Monkol Lek’s lab at Yale University who is developing a method to identify mtDNA mutations in whole-genome sequences.
O
ver the past decade, the Genome Aggregation Database (gnomAD) has amassed whole-genome sequences from tens of thousands of people. Because it excludes children with autism or other pediatric neurological conditions, it can serve as a reference to help researchers identify variants linked with such conditions.Until 2020, gnomAD didn’t include data on mtDNA variants. But once it did, Lake and her team developed a method to use existing, smaller mtDNA databases in combination with gnomAD to locate mitochondrial mutations that might be linked to disease.
In an analysis of 56,434 whole genomes from gnomAD, 231 carried an mtDNA variant known to be pathogenic — roughly 1 in every 250 people, or about half a percent. The team also identified 997 variants not previously identified in existing mitochondrial databases. The findings were published in Genome Research in January.
Lake and her colleagues are developing a model to home in on areas of the mitochondrial genome that are most likely to harbor disruptive variants. Scientists use similar models to find autism-linked genes in the nuclear genome, Lake says. “We hope this will also be a useful tool for autism research, to help elucidate the contribution of mtDNA.”
I
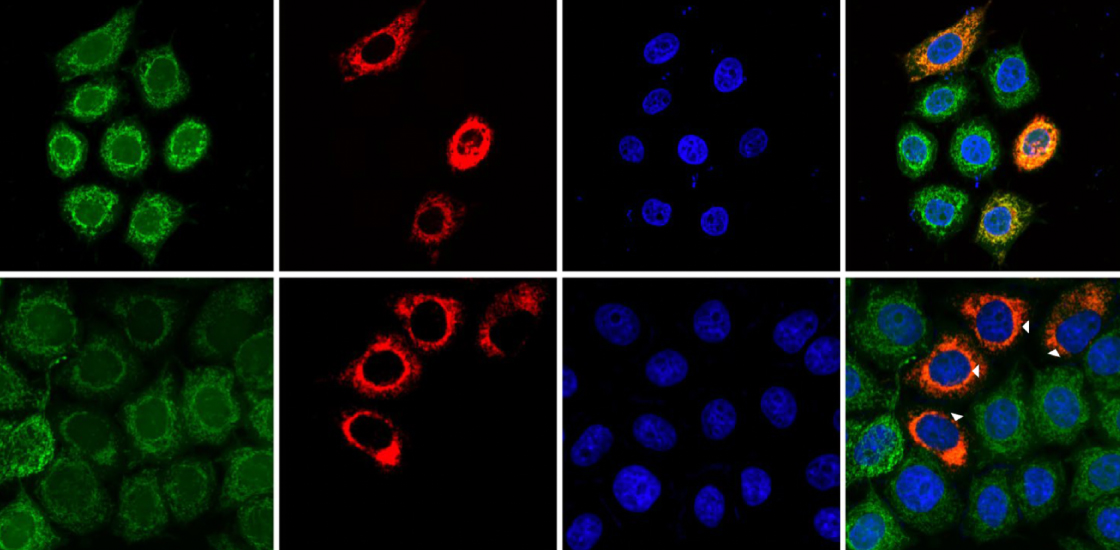
dentifying mtDNA variants potentially linked to autism is just the first step. To test the effects of mutations in nuclear DNA in cells or animals, researchers often turn to the gene-editing tool CRISPR. But CRISPR relies on stretches of single-stranded genetic material to deliver the tool to a precise spot in the genome — a method that currently doesn’t work in mitochondria.In 2020, researchers identified an enzyme that can act as a DNA base editor without CRISPR, but only on sequences with certain base pairs. Newer versions of the enzyme can act on a greater variety of sequences and have improved editing efficiency in both mitochondrial and nuclear DNA, according to a paper published in Nature Biotechnology in April.
The updated editors enabled the researchers to introduce two mtDNA mutations previously linked to different conditions — benign kidney tumors and a degenerative eye disease — into human cells in a dish. Cells with either mutation showed reduced mitochondrial activity; introducing the mutations using the earlier version of the tool had no such effect, suggesting that those edits were unsuccessful.
The tool “will enable researchers to study the cellular effects of specific mtDNA variants, including those identified in individuals with autism,” Lake says.
Y
et another new technique could power experiments involving mitochondrial replacement. Developed to prevent the transmission of potentially lethal mtDNA mutations from mother to child, the approach could have broad research implications, says Elizabeth Ann Jonas, professor of internal medicine and neuroscience at Yale University, who was not involved in the work but studies mitochondria in mouse models of fragile X syndrome.Mitochondrial replacement makes it possible to swap an embryo’s mtDNA — inherited entirely from the mother — with that of a donor. But if even a few copies of the embryo’s mutated mtDNA evade replacement, they can replicate, reducing the technique’s overall effectiveness.
To address such ‘genetic drift,’ researchers took advantage of a cellular process called mitophagy, which recognizes and clears mutated mtDNA from cells while leaving healthy copies alone. They harness “forced mitophagy,” as they call it, to identify mtDNA carrying unwanted mutations and degrade those copies.
In human embryos treated with forced mitophagy, less than 1 percent of mtDNA copies retained mutations, compared with about 4 percent of those in controls, according to findings published in Nature Biomedical Engineering in April.
Mitochondrial replacement is not yet approved for use in people in the United States, but forced mitophagy could provide another strategy to edit mitochondria in cells or animals and study variants’ effects, Jonas says. It’s “very interesting” for autism researchers, she says. “It basically means that you can remove the mitochondria of choice from your cell and insert other mitochondria.”