The innovators: How families launch their own autism studies
Some parents are starting ‘N-of-1’ studies for autism, but their efforts don’t always get taken seriously.
Editor’s Note
This article is the third in a four-part series on the unique relationship between researchers and families in the autism community. Be sure to read the first two articles in the series: The pioneers and The seekers. The fourth and final article goes live 5 October.
Listen to the Spectrum podcast to hear more from the parents and scientists featured in the Family Ties series, as well as the reporters’ experiences behind the scenes:
J
ohn Rodakis expected Thanksgiving of 2012 to feature turkey and football, just like it had in past years. Instead, it brought his two children a strep infection and a prescription for the antibiotic amoxicillin. He and his wife dutifully dosed the children with the cotton-candy-pink liquid twice each day. By the end of the holiday weekend, the children’s fevers and all other signs of the infection had disappeared. As Rodakis continued giving them the 10-day course of antibiotics, he found that it had an unexpected effect on his 4-year-old son, who had been diagnosed with autism earlier that year.His son had shown some speech delay, but had otherwise been a happy, healthy baby until about 30 months, when his development abruptly stopped. Rodakis immediately knew something was wrong. Like many children with autism, the boy suddenly had difficulty making eye contact, rarely spoke and wouldn’t socialize with other children. Nothing seemed to help his behaviors — until he started the antibiotics. By the Monday after Thanksgiving, he was speaking in short sentences rather than single words, and he had started to make eye contact.
“Each day, he seemed to get better; I had no idea what was going on,” Rodakis recalls.
Rodakis isn’t a scientist but a venture capitalist, investing in biotechnology startups. He started to search through the medical literature to see if he could learn more about why antibiotics might be helping his son. He found few scientific reports of children with autism improving while on antibiotics or ill with fevers. But when he spoke with parents in internet groups, he heard many such stories.
“So many parents had seen a similar pattern, but there wasn’t much in the media or scientific literature,” Rodakis says. “It was very frustrating. I had no idea why there wasn’t any follow-up.”
A self-described tech geek, Rodakis had been logging many of his son’s behaviors and their severity daily using the iPhone app Autism Tracker, so he knew he hadn’t imagined the improvements. The logs also documented the return of many of the child’s autism-related behaviors after he finished the antibiotic course. He retained his improved ability to make eye contact, although it still was not the same as that of a neurotypical child. Doctors prescribed Rodakis’ son several other courses of antibiotics for infections over the next few years. His signs of autism improved every time he took amoxicillin, but not while taking co-trimoxazole, a combination of two other antibiotics (amoxicillin and co-trimoxazole differ somewhat in the types of bacteria they target).
When Rodakis took his data to autism researchers, they urged him to publish the details as an ‘N-of-1’ case study (‘N’ refers to the number of participants). Many of medicine’s most successful treatments started off when one parent, physician or person with a condition noticed something unusual. But these types of trials, also known as ‘single-subject design,’ have also historically been scorned by clinical researchers. After all, the logic of a clinical trial is to apply the same therapy systematically to a large number of diverse people with a condition, in order to draw conclusions about the therapy’s effectiveness.
The growing interest in personalized medicine and the quantified self, in which people use technology to track their own physiological data or symptoms, is beginning to shift researchers’ views toward N-of-1 trials. The search for effective treatments for a variety of chronic conditions has led to a boomlet of N-of-1. The conditions run the gamut, ranging from speech disorders to stroke, bipolar disorder, cancer and fibromyalgia.
Although N-of-1 trials are on the rise in every area of medicine, they have had a particularly large impact on autism research. Based on work by Rodakis and other parents, some autism researchers are beginning to explore potential causes and novel treatments they might otherwise have missed.
“Parents want to find answers, and we have to listen to them and be skeptical at the same time. N-of-1 trials can be a messy way of looking at things, but they provide important clues about what’s going on,” says Richard Frye, a pediatric neurologist at the University of Arkansas in Little Rock. “I think they are really under-utilized in medicine.”
These trials provide a two-way street: People with a condition can try different regimens and find options that work best for them, and scientists are exposed to new ideas that could drive research forward.
Unique trials:
F
or decades, randomized controlled trials have been medicine’s gold standard. Although these trials can vary in their design, the general premise is the same: randomly divide a group of people with a particular condition into two groups, giving one group a drug or treatment and the other a placebo. This approach has led to many of medicine’s biggest breakthroughs because it lets scientists account for the placebo effect, as well as the typical waxing and waning of chronic conditions. Sophisticated statistical analyses can adjust the data for variables such as age, race, ethnicity, sex and socioeconomic status, says Richard Kravitz, professor of medicine at the University of California, Davis.But the trials also have serious limitations. Inclusion criteria — rules that determine who is and isn’t eligible to be included — are often restrictive, which can bias the research in one direction or another and lead to conclusions that apply to a small portion of the population. For diverse conditions such as autism, treatments that work for one set of individuals may have no effect on another group and may even harm some individuals.
“Randomized controlled trials are designed for the average patient, but most patients aren’t average,” Kravitz says.
An N-of-1 trial can be used to assess a single treatment or compare the effects of several treatments in one person. The person serves as his own control. An ideal N-of-1 trial typically intersperses intervals of treatment with ‘washout’ periods, during which the person receives no treatment at all. The treatment is then reinstated to see if the same changes recur. Kravitz outlines this approach in a document commissioned by the Agency for Healthcare Research and Quality, the government agency tasked with improving the healthcare system. However, interpreting data from these trials is challenging even for highly trained individuals, says Mark Drangsholt, a trial design expert at the University of Washington in Seattle. In some cases, devices such as fitness trackers can provide, for example, unbiased recordings of sleep duration. But having a parent tell you which treatment improved their child’s social skills is much murkier. It’s a double-edged sword: Participant buy-in means they’re more likely to stick with the treatment, but it might also inflate their belief in its efficacy.
In some ways, a basic N-of-1 trial is not all that different from a standard visit to the doctor, who might try out a series of treatments before finding one that works. But it is different in that it rigorously documents baseline symptoms as well as the effects of a treatment. Most people begin tracking their symptoms only after they start a treatment, which can give them a biased view of how much it actually helps.

Not every condition can be studied using an N-of-1 design. Short-lived, acute conditions such as strep throat don’t linger long enough to adequately test multiple treatments. Conditions in which symptoms can shift in intensity, such as autism, are also harder to test, because participants and physicians need to observe the effects over long periods. They must also have easily measurable benchmarks, such as symptoms that can be tracked with a smartphone app, or blood and urine tests.
Drangsholt says the popularity of N-of-1 trials is bound to rise, due both to the ready availability of self-tracking devices such as smartphones and Fitbits and to people taking an increasingly active role in their own care.
It was this enterprising attitude that led Rodakis to investigate his son’s response to amoxicillin. As it turned out, his project would follow in the footsteps of a parent who had discovered something strikingly similar two decades earlier.
Familial territory:
A
ndy was the youngest of Ellen Bolte’s four children. Up until 18 months of age, he followed the same developmental path as his three older siblings. A series of suspected ear infections led to several courses of antibiotics, during which Andy’s behavior began to change. He stopped making eye contact and starting screaming at the slightest provocation. His diapers filled with a foul-smelling goo that looked nothing like what Bolte had seen in the thousands of other diapers she had changed. Andy vomited fist-sized balls of mucus. Every day brought with it a new symptom.“As my husband and I would put him to bed, we would ask ourselves, ‘What did he do today that he won’t be able to do tomorrow?’” Bolte says.
The changes were so extreme that Andy was diagnosed with regressive autism just after his second birthday, a remarkably early diagnosis for the mid-1990s. Bolte, a Chicago-area computer programmer, knew nothing about medicine, but she didn’t believe the experts who told her she must have missed early signs of his autism. They told her autism was a genetic condition, meaning that Andy was born with it and there wasn’t much she could do.
Bolte rejected that advice. Instead, she visited Chicago’s many medical libraries to log onto the fledgling internet and study autism. Delving through the densely written scientific literature, Bolte began to see a connection between her son’s antibiotic use, gastrointestinal symptoms and autism. Over the course of a year, Bolte formulated her hypothesis: Andy’s prolonged course of antibiotics had killed his healthy gut bacteria, allowing harmful bacteria to take over. These microbes secreted toxins that harmed his neurons and ultimately triggered his autism. If this were true, then eliminating the damaging bacteria and perhaps allowing his brain to recover might help his symptoms.
Bolte went to specialist after specialist, armed with her hypothesis and the research to back up her point. “I was not warmly received,” she says. Most doctors had no idea what to do with her theory. Many dismissed her outright; others simply referred her on to another specialist.
After visiting nearly 40 experts, one doctor — pediatric gastroenterologist Richard Sandler — agreed to hear her out and help however he could. Her first visit lasted several hours, and Andy screamed the entire time. After a month of deliberation over Andy’s obvious misery, Bolte’s desperation and the strength of her hypothesis, Sandler agreed to her proposal: eight weeks of vancomycin to kill the harmful bacteria in his gut and hopefully allow the healthy flora to take over and alleviate his symptoms. Key to their agreement was Bolte’s insistence that she keep everything else in Andy’s life the same, from the brands of foods he ate to his sleep schedule. This consistency was what made Andy’s vancomycin treatment an N-of-1 trial as opposed to simply following a hunch, or randomly trying out possible therapies.
“Most people want to throw as many treatments as possible at the problem, and who can blame them? But testing the effects of a specific treatment means making sure that is the only thing you’re doing differently,” says Duke University neurologist Richard Bedlack, who investigates alternative treatments for amyotrophic lateral sclerosis (ALS).
After a month of taking the vancomycin, the changes were “nothing short of remarkable,” Bolte says. Andy began making eye contact. He started babbling and using the toilet. And he stopped screaming. At his eight-week follow-up appointment, Sandler realized right away that Bolte had probably been right. He prescribed another month of antibiotics to see if Andy’s improvement could be extended. The improvements persisted, but Bolte and Sandler agreed they had to stop the antibiotics: Andy wasn’t a guinea pig.
Still, Andy’s response to the treatment encouraged Sandler and Bolte to set up a larger trial in other children with regressive autism whose symptoms began after antibiotic treatment. Bolte and Sandler approached Sydney Finegold, an infectious disease expert at the University of California, Los Angeles. Finegold found Bolte’s hypothesis and results so intriguing that he immediately agreed to help with the trial.
“I had trouble convincing journals that this was a legitimate study, but there was no other easy explanation for what was going on,” Finegold says.
With Finegold’s help, Sandler and a group of American researchers were able to repeat the vancomycin treatment with similar results. They included several children being treated at university clinics for regressive autism who also had a history of antibiotic use around the time their symptoms appeared. The study, published in 2000 in the Journal of Child Neurology, was one of the first to establish a potential link between gut flora and autism. Although the microbiome is now one of medicine’s hottest areas of research, at that time it was brand-new.
“There was this subset of kids with autism that had gut problems, and no one was focusing on that. They were just looking at the brain, and Ellen helped us realize that maybe we’ve been looking at the wrong end,” says Emma Allen-Vercoe, a microbiologist at the University of Guelph in Canada.
”“Randomized controlled trials are designed for the average patient, but most of our patients aren’t average.” Richard Kravitz
Parallel stories:
O
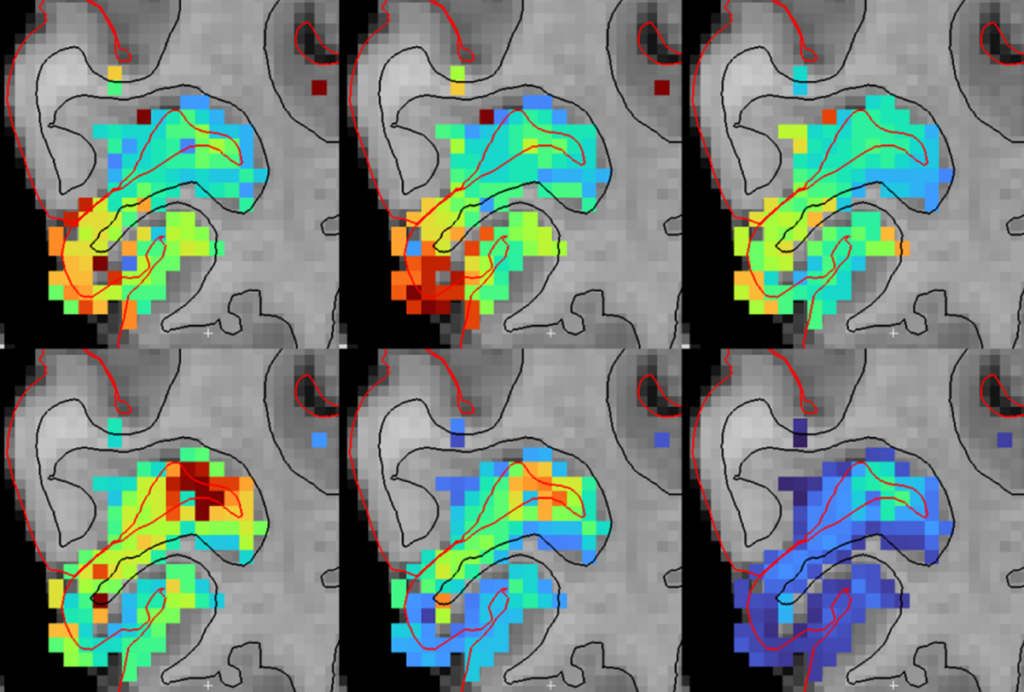
ther potential autism treatments have also originated from N-of-1 trials that were subsequently expanded. In the early 2000s, researchers reported a condition called cerebral folate deficiency (CFD), which results from folate not getting into the brain and is characterized by seizures, learning difficulties and irritability. Early case reports mentioned that many children with CFD also have symptoms of autism. When a boy with possible CFD and autism showed up at Richard Frye’s clinic five years ago, Frye tested the boy for antibodies to the folate receptor protein — a test that is diagnostic for the disease. With the diagnosis confirmed, Frye prescribed leucovorin calcium, which helps transport folate into the nervous system and alleviates symptoms of CFD. To his surprise, Frye found that it also improved the boy’s autism symptoms. Based on this observation, Frye began to collaborate with other researchers to test children with autism for signs of CFD, thinking they might benefit from the treatment.Frye asked 44 families to document their children’s symptoms before and after treatment, and used the families still waiting for CFD test results as controls. “Parents are often partners in these trials, since they typically know their children best, and are often the first to pick up on subtle changes in behavior,” says Frye. The results were published in a 2012 study showing that this treatment can also improve symptoms in children who have only autism.
“You can’t do double-blind clinical trials on everything,” says Frye. “N-of-1 trials provide an important jumping-off point. They can generate better data about what might be causing a disease and what might work to treat it.”
Researchers in other specialties have taken this approach even further. Bedlack treats people with ALS, a condition with few treatments. He sees parallels between ALS and autism that encourage experimentation. That isn’t necessarily a problem, Bedlack says, as long as there’s an open, non-judgmental conversation about the options.
“People want to believe there’s something better out there to treat their illness, but they’re hesitant to share their efforts with their doctors because there’s often a dismissive or paternalistic response,” Bedlack says.
Bedlack’s willingness to look beyond the standard randomized controlled trial and prowl the back alleys of the internet for new ideas has given him the nickname ‘the Fox Mulder of ALS.’ People often come to him with ideas they read about online, such as coconut oil or protein supplements. Researching each option could take hours, and the process would have to be repeated for each. So Bedlack created ALS Untangled, an online forum where anyone can submit ideas for ALS therapies. Bedlack and an international team of ALS specialists then search through both medical literature and unconventional reports in what Bedlack refers to as the “dark corners of the internet.” They review the information from all their sources, and ultimately publish their conclusions in a research article that anyone can read for free.
Because symptoms of both ALS and autism change over time, it can be difficult to interpret the results of N-of-1 trials; a treatment might seem to be working, but the effect could just be a consequence of the condition’s inherent changeability. So doctors need to know the history of the condition in that particular individual in order to identify “what is a big enough signal that we can be confident is not noise,” Bedlack says.
Although he and his team haven’t yet found any unexpected therapies for ALS, they have found that cooking with coconut oil might help with the weight loss, dry skin and constipation that many people with ALS report. Bedlack also investigated what seemed to be a partial reversal of ALS symptoms in an individual who took lunasin, a peptide supplement derived from soy. The results were promising enough to warrant Bedlack to launch a small open-label pilot study of the supplement, which is underway.
“Until you actually look at something, you can’t say whether or not it works,” Bedlack says. “It would be doubly tragic to have an effective treatment out there that no one could be bothered to test.”
Back to the future:
T
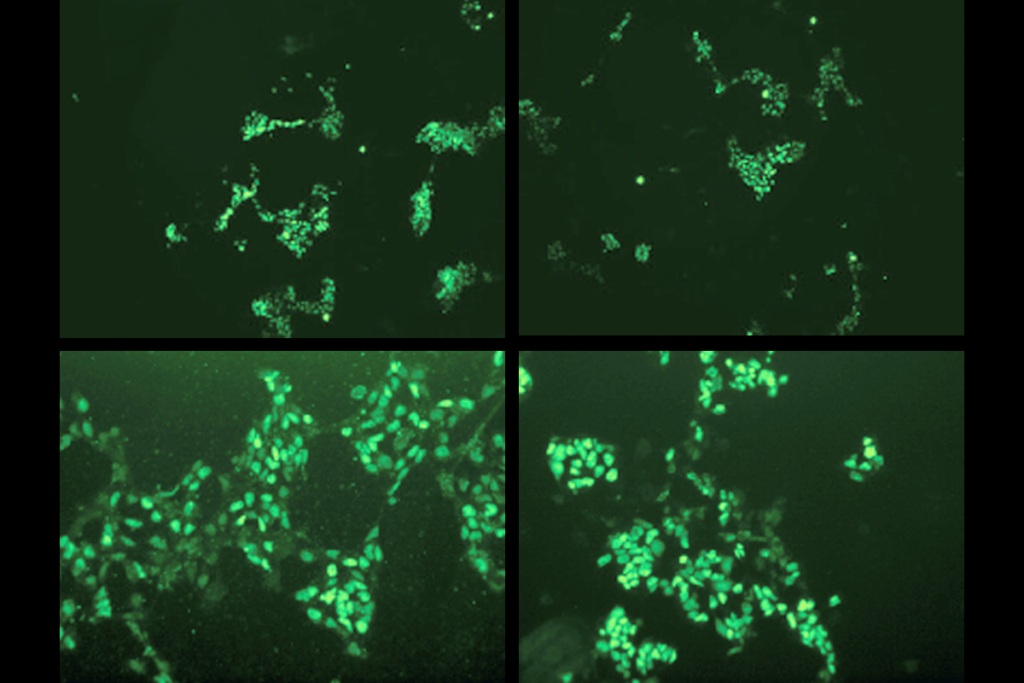
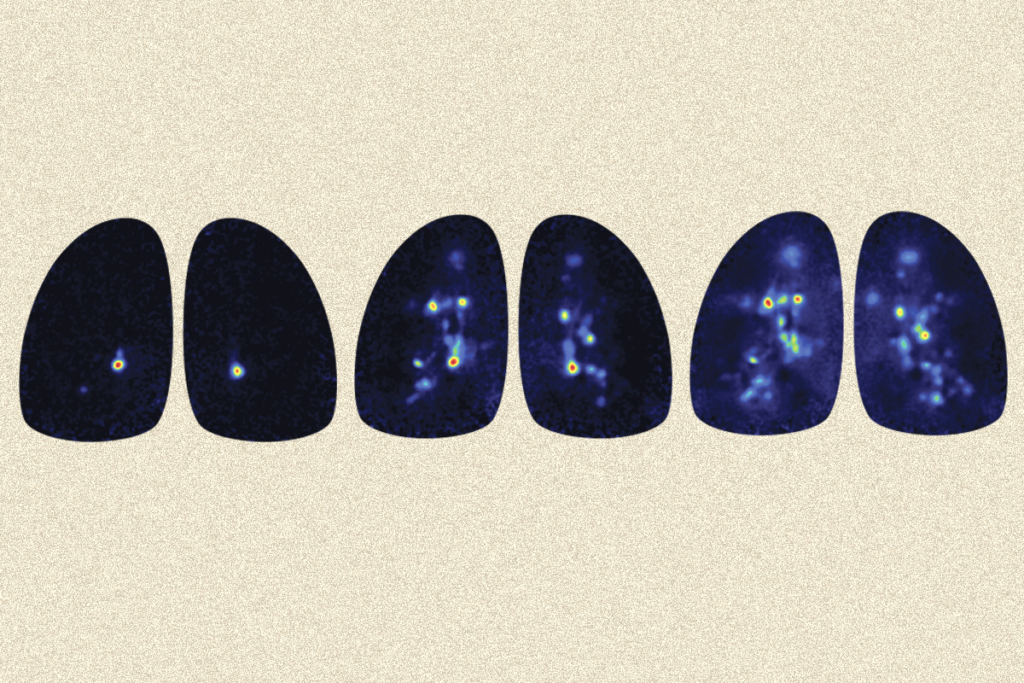
he challenge for both Rodakis and Bolte has been opening doctors’ minds to new ideas from families. Frustrated at having doctors brush off his ideas and observations about his son, Rodakis used his venture capital background to launch a nonprofit called the N of One: Autism Research Foundation. His goal was not to fund N-of-1 trials for autism per se, but rather to help fund pilot studies that combine data from a small number of people, especially in the area of autism and the microbiome.In late 2014, the first study he funded reported the effects of a chemical called sulforaphane on autism symptoms. Sulforaphane, found in broccoli and Brussels sprouts, stimulates heat-shock proteins, which are also activated when people have fevers. Lead researcher Andrew Zimmerman, a pediatric neurologist at the University of Massachusetts in Worcester, was one of the first to document what parents had long observed: that the behaviors of many children with autism improve while they have a fever. He suspected that sulforaphane stimulates some of those same beneficial effects.
When he tested the compound in 29 young men with autism, he found a significant improvement in their behaviors. The study was met with no small amount of pushback. Critics argued that the broccoli sprout extract was only successful given the unusually small placebo effect in the trial. What’s more, only about 30 percent of people with autism experience the ‘fever effect,’ which means the participants were not necessarily representative of everyone with autism. Zimmerman and others are continuing to study the compound.
N-of-1 trials have met with more systemic criticisms. At the research blog Science-Based Medicine, physician David Gorski notes that N-of-1 trials don’t tell scientists whether someone improved specifically due to the treatment or whether it was a placebo effect — the act of being treated — that helped. It’s why one person may find something such as acupuncture beneficial even when rigorous trials show the procedure to be no better than a sham treatment. Although a well-designed N-of-1 trial with multiple different treatments and washout periods might help rule this out, its reliance on one person’s data means that any bias can have a big impact.
Take Rodakis’ observation of his son’s improvement on antibiotics. He did his best to record his son’s symptoms accurately, but he also knew that his son was taking this medication. His normal, parental desire to see an improvement may have caused him to see improvements that were more significant than they really were. A larger trial in which participants didn’t know if their children were receiving antibiotics, and in which neutral observers rated the participants’ behavior, would potentially have eliminated that bias.
“It’s a very human tendency – we all do it – to remember the things that meet with our expectations or beliefs and forget the ones that don’t,” Gorski says. “That’s part of the reason you need science.”
As Gorski points out, failing to challenge a person’s beliefs with skepticism and rigorous research often creates a slippery slope toward out-and-out pseudoscience. Just because something works in an N-of-1 trial doesn’t make it a valid therapy, he says. That is, N-of-1 trials showing benefits of the fever effect, antibiotics on autism symptoms, or special diets for autism don’t mean they’re generally effective or that they should be adopted by other families or prescribed by doctors.
Then there’s the issue of applying the results of one N-of-1 trial to many people. Writing in the Postgraduate Medical Journal, biostatistician Robert Gordon Newcombe at Cardiff University in Wales notes that in large clinical trials, doctors can be reasonably confident that the treatment will work in a person similar to those included in the study. The idiosyncratic nature of individual people means that the results of an N-of-1 trial might actually be relevant to only that person. In other words, the personalization of these trials is both a strength and a weakness.
On their own, N-of-1 studies aren’t enough to spur broad changes in how everyone is treated, but they might help people decide which potential treatment works best for them. Integrating observations of parents is key to this process. When Rodakis asked his son’s pediatrician about trying a dairy-free and gluten-free diet, the doctor told him it wouldn’t improve the boy’s autism features. Rodakis knew that clinical trials had not found a benefit of the diet in large groups of children with autism, but he also knew that didn’t mean they were never effective. Despite what the research literature said, he started his son on a dairy-free diet. Rodakis believes it worked — he says his son began speaking more, using more words together and relying less on pointing.
“It would be great if someone comes up with a universal treatment for autism,” he says. “However, in the meantime, I’d like to see less emphasis on group results and more emphasis on understanding why some people respond to certain treatments and using this to identify subtypes of autism.”
Until that day arrives, Rodakis says, there’s always the N-of-1 trial.
Return to “Family ties” series
Syndication
This article was republished in The Atlantic.
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome
Changes in autism scores across childhood differ between girls and boys
Explore more from The Transmitter
Smell studies often use unnaturally high odor concentrations, analysis reveals
‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt