There are no therapies approved for the core traits of autism, nor for most genetic syndromes linked to the condition. But there are many under investigation, and those that do come to fruition will likely target one of three levels of human biology, according to an expert review published in February in Translational Psychiatry: DNA, mRNA or proteins.
Such treatments could take the form of gene therapies, antisense oligonucleotides (ASOs) or small-molecule drugs, respectively, according to lead investigator Lilia Iakoucheva, professor of psychiatry at the University of California, San Diego, and Derek Hong, who worked on the paper as a graduate student in Iakoucheva’s lab. Spectrum caught up with Iakoucheva and Hong to discuss their ideas.
This interview has been edited for length and clarity.
Spectrum: In the paper, you say it’s time to shift away from identifying more autism-linked mutations to doing something about treating them. Could you talk a little bit about that?
Lilia Iakoucheva: What I mean is that we should probably advance both fronts. Autism has many rare genetic variants associated with it, which means we have lots of low-hanging fruit, right? I did not mean to say we have to stop gene identification, but I think we have to also advance therapies. Whole-genome sequencing will help to identify the interplay between rare de novo and common inherited alleles. There is more and more evidence now that common inherited variants play a very important role in the genetics of autism, especially for the syndromes in which we cannot find a high-confidence rare de novo variant.
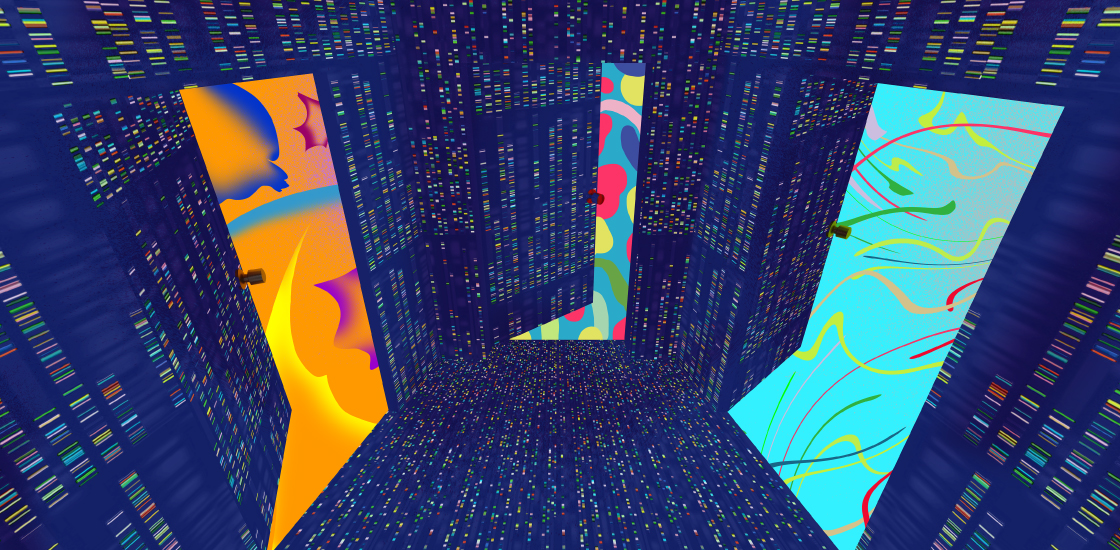
Derek Hong: To add on to that, I feel like recent whole-exome sequencing results drove a wedge into a door where we can begin to investigate therapeutics for those specific genes. But I think given more whole-exome sequencing investigation, we could potentially drive wedges through some more doors for targeting.
S: In this paper, you discuss three targets for intervention: DNA, mRNA and proteins. Which seems the most promising or furthest along?
DH: The biggest things that come to my mind are the natural antisense transcripts that are expressed alongside certain autism susceptibility genes. Some natural antisense transcripts inhibit the translation of an autism-linked gene that’s implicated or that has a loss of function. I think it could be very promising to target these because ASOs themselves are relatively transient, meaning in a clinical setting we could potentially work with a dose that we know is tolerable and isn’t dangerous. And if necessary, after four months, when the drug is no longer in someone’s system, we can adjust that dosing without significant harm.
LI: Sometimes you can come up with treatment without even knowing the neurobiology. For example, in the ASO for spinal muscular atrophy (SMA), we still don’t know why those motor neurons are dying, but we have a treatment anyway.
But I think all three levels of intervention are valid, and they are all promising. CRISPR approaches should be approached with a high degree of caution because they’re harder to reverse, whereas small molecules are probably less dangerous because they will degrade. So in terms of development or safety, I think the small molecules will be the least dangerous, ASOs will be the second most and CRISPR-based approaches will be the most risky, in my opinion.
S: In terms of biological pathways, how do you decide which approach is most applicable?
LI: It depends on what is being corrected, right? We know synapses and circuits are implicated in autism. But depending on the gene, there can also be translational pathways or ubiquitination pathways. You’re not going to correct everything with just one drug because autism is so multigenic. Even if a single gene is mutated, it still can influence a variety of different pathways. There is a lot of work that would need to be done to deconvolute all the pathways involved in autism.
S: In your paper, you talk about some of the obstacles yet to be overcome, including the blood-brain barrier and delivery challenges. What are the most significant obstacles, and what do you think it’s going to take to get past them?
LI: The most challenging thing is to determine when to treat, what cell types to treat and how we judge whether the treatment actually helped. This may mean we need to select specific cohorts for clinical trials because maybe one treatment is not going to help everybody. There are lots of challenges to address before we can start treating, beyond things like the blood-brain barrier. Given so many different labs and companies working on delivery, I think that could be solved more easily than factors like at what time point and what population to treat, and how we judge improvement.
S: Are there models of success from the field?
LI: Well, we have a very short list of Food and Drug Administration-approved therapeutics for genetic conditions so far. We have SMA, where the drug is delivered through a spinal tap. We have trofinetide, which was just approved for Rett syndrome.
DH: There are some phase 1 and 2 clinical trials for Angelman syndrome, specifically using ASOs to target the natural antisense transcripts for UBE3A. I’m watching that with some promise because there are three different groups working on that. That’s what I’m currently looking at. Especially given the ASOs used in the past for SMA.
LI: Maybe the next one will be Angelman. Actually, it looks like that.