The enemy within
The possibility that autism is caused by a maternal immune system gone awry is no longer a fringe idea — but proposals to identify or fix these glitches are still controversial.
Judy Van de Water got into autism research precisely because she wasn’t an expert in autism. She is an immunologist, studying the strategies our bodies employ to defend us against pathogens, and the ways those strategies sometimes misbehave or overreact. But about 15 years ago, the then-new MIND Institute, which sought to bring fresh eyes to understanding disorders of brain development and function, set up shop near her lab at the University of California, Davis. When the institute asked for grant proposals from specialists in fields outside brain development, Van de Water heeded the call.
Her proposal eventually led her to pursue an outsider idea: the possibility that immune responses in an expectant mother’s body, unleashed in the wrong place at the wrong time, can interfere with the development of the growing fetus’ brain. She now holds that this immune activity could be the cause of nearly one in four cases of autism. In particular, Van de Water blames a certain set of antibodies, immune molecules designed to target invading infectious agents and destroy or neutralize them. She’s so sure she’s right that she refers to it confidently as ‘MAR,’ or ‘maternal-antibody-related autism.’
From the start, it was a provocative theory that ran counter to prevailing beliefs about both the immune system and autism, and in the early days Van de Water was one of its few proponents. “We’ve been swimming upstream — still are,” she says. Her peers criticized Van de Water’s work on the grounds that her results didn’t support her claims. And they were deeply upset when, in 2013, Van de Water formed a licensing partnership with a San Diego-based company called Pediatric Bioscience. That deal was aimed at developing a maternal antibody screen that might allow for early diagnosis of autism or, if performed prenatally, indicate the risk of having a child with autism. “This is very, very premature,” Yale University autism researcher George Anderson told Science at the time.
Still, despite the controversy, the basic idea underlying Van de Water’s work — that maternal immune activity can increase risk for some types of autism — is edging into the mainstream. Researchers from other labs are exploring the consequences of maternal immune activity. Some teams are investigating a second immune pathway, involving cytokines, signaling molecules that coordinate the response to infection. Their results, showing that antibodies and cytokines are both capable of producing autism-like symptoms in mice, have been reported in the past year in prestigious journals and at high-profile conferences.
The implications of this idea could be a huge deal for families. It should be possible to offer a test that screens a woman for the antibodies that might trigger autism, just as Van de Water hopes to do. “Testing for the presence of a particular antibody is something that, in principle, we know how to do,” says Betty Diamond, an immunologist at the Feinstein Institute for Medical Research in Manhasset, New York, who is another leader in the new field. What’s still unclear is how accurately such a test in a woman would predict autism risk in her child. Diamond is instead focusing her lab’s efforts on prevention. She envisions treating a woman who carries the harmful antibodies with a relatively benign medicine that would neutralize the antibodies. “We want to develop something that’s safe enough that if we give it to 10 times the number of people we need to in order to protect one fetus, we haven’t done any damage at all,” says Diamond.
”“We’ve been swimming upstream — still are.” Judy Van de Water
Fragile truce:
The suspicion that there might be a connection between the immune system and autism first emerged in the 1980s, based mostly on anecdotal evidence. In a 2006 review of the nascent field, Van de Water’s team called the immune system “a new frontier” for autism research and laid out several relevant themes: Children with autism spectrum disorder often have problems with their immune systems — they are sick more often than typically developing children are — and show evidence of neurological abnormalities, such as aberrant brain structures. What’s more, women with autoimmune diseases, in which the body attacks healthy cells as if they were invaders, are more likely to have children with neurological disorders than are their peers. (A 2015 paper later confirmed this, showing that women with the autoimmune condition lupus double their risk of having a child with autism, and women with rheumatoid arthritis or celiac disease are also at increased risk.) In her review, Van de Water also noted that immune dysfunction and autoimmunity have been associated with other disorders of brain development, such as schizophrenia, Tourette syndrome and Alzheimer’s disease.
Since 2006, researchers pursuing these observations have generally followed one of two tracks: Some have focused on immune issues in children, and others have explored what might happen in utero when a woman’s immune system misfires, overreacts or is ill-timed.
During pregnancy, a woman’s immune system can be said to be conflicted. To defend her against invading pathogens and microbes, the system marshals a veritable army of weapons, ranging from B cells and T cells to antibodies, and deploys them in an impressive variety of ways to get the job done. Yet a growing fetus carries its father’s DNA as well as its mother’s, making it a half-foreign presence in her uterus. In response to this built-in standoff, a pregnant woman’s body compromises. It lets down its defenses a little, suppressing the immune system of the mother in favor of the fetus. So what happens if the woman does get sick while pregnant? Or has an immune system that doesn’t work well to begin with?
From such questions, a theory emerged, first published in 1990, that perhaps the fragile truce between the maternal immune system and a developing fetus doesn’t always hold. When it fails, the hypothesis goes, the mother’s defense mechanisms are activated — or sometimes malfunction — and damage the fetus.
Resistance to investigating immune connections to autism, in either children or their parents, was strong. “People assumed that everything is genetic,” says Andrew Zimmerman, a pediatric neurologist at the University of Massachusetts Medical School and an early researcher of maternal immune antibodies. What’s more, it was long thought that the immune system and the nervous system don’t interact much because most pathogens and immune molecules cannot breach the blood-brain barrier. (That barrier acts as a moat to protect the brain from compounds or pathogens in the blood.) Also, the idea that a woman’s immune system might cause problems in the fetus came to the fore as the autism community was trying to undo the damage from the now-discredited theory that vaccines can cause autism. The experience placed an additional burden on any research implicating the immune system in autism.
Forging ahead:
Undaunted by the headwinds, Van de Water’s lab initially pursued research in both children and mothers, but eventually, her former postdoctoral fellow, Paul Ashwood, took the lead in investigating children’s immune problems at his lab at the University of California, Davis, while Van de Water continued to think about the mothers. She pursued the idea that maternal antibodies attack the growing fetus’ brain, killing healthy cells and setting development off track in a way that might eventually result in autism. “The maternal antibody story made sense on a biological level to me,” says Van de Water. She started by screening blood from women who have children with either autism or specific language impairment, looking for patterns that stood out when compared with the blood of mothers of typically developing children.
Support for the idea came from a 2003 case study of a 38-year-old woman who had one typically developing child, one with autism, and one with specific language impairment. A group of researchers at Oxford University in the U.K. found that her blood carried an antibody that bound to fetal brain tissue from mice, meaning that the antibody was specialized for a target, or antigen, in the mouse brain. The scientists injected serum from that woman into pregnant mice. The pups from these mice were less likely to explore, and a little slower at a standard test of motor coordination, than pups born to mice injected with serum from controls. In 2007, Zimmerman and his collaborators took the work further to show that antibodies in the serum from mothers of children with autism bind to targets in brains from only fetal rats, not adult rats.
Meanwhile, Van de Water’s hunt soon paid off. In 2008, her group reported that in 7 out of 61 mothers of children with autism, or 11.5 percent, they had found a common, characteristic set of antibodies in the women’s blood that bound to tissue from fetal, but not adult, human brains. The researchers could not say why some women produce these antibodies and others don’t or whether these antibodies persist in women for life or are transient — and they still don’t know. It took four tries to get that paper published. Van de Water says one reviewer responded with just one line: “We don’t know that autism has anything to do with the immune system.” Shortly thereafter, her team joined with MIND Institute neuroscientist David Amaral and reported that four rhesus macaque monkeys exposed in utero to the human maternal antibodies showed behavioral abnormalities such as stereotypic pacing and hyperactivity. Watching those young monkeys struggle, says Van de Water, was “the moment I knew the antibodies were doing something.”
In 2013, her group identified seven proteins, all involved in neural development, that apparently are targets of maternal antibodies. Of the 246 mothers of children with autism in this larger study, Van de Water’s team reported that 23 percent carried some combination of antibodies to the specified proteins, compared with only 1 percent of the 149 mothers of typically developing children. (Others who have analyzed the data from that paper say 23 percent is too high because Van de Water’s team included various combinations of antibodies in that figure. Steven Goodman, a biostatistician at Stanford University, noted in Science that no single pattern was found in more than 7 percent of the mothers.)
Diamond, an expert in lupus, wondered whether these same women might have signs of autoimmune disease in their cells even if they showed no symptoms. That’s exactly what her research later found. “They weren’t hurt by it because of an intact blood-brain barrier, but their fetuses might be hurt by it,” she says.
It turns out that a developing brain might be more vulnerable to autoimmune activity because it is not yet fully protected by the blood-brain barrier. In 2014, Diamond and her colleagues found that in mice, the blood-brain barrier of a developing fetus becomes truly impenetrable only in the third trimester. If a similar window of vulnerability exists in people, the implications for brain development are significant. The long-held belief that the brain is ‘immune privileged’ and that antibodies can’t reach it has had to evolve. “We were too limited by that,” says Lior Brimberg, a postdoctoral fellow in Diamond’s lab.
Diamond’s team tested sera from more than 2,400 mothers of children with autism for the antibodies that attack fetal brain tissue. They found that the women who have these antibodies are more likely to have an autoimmune disease than are women who do not have the antibodies. They also found that mothers of children with autism are four times more likely to harbor the antibodies than is a control group of women of childbearing age.
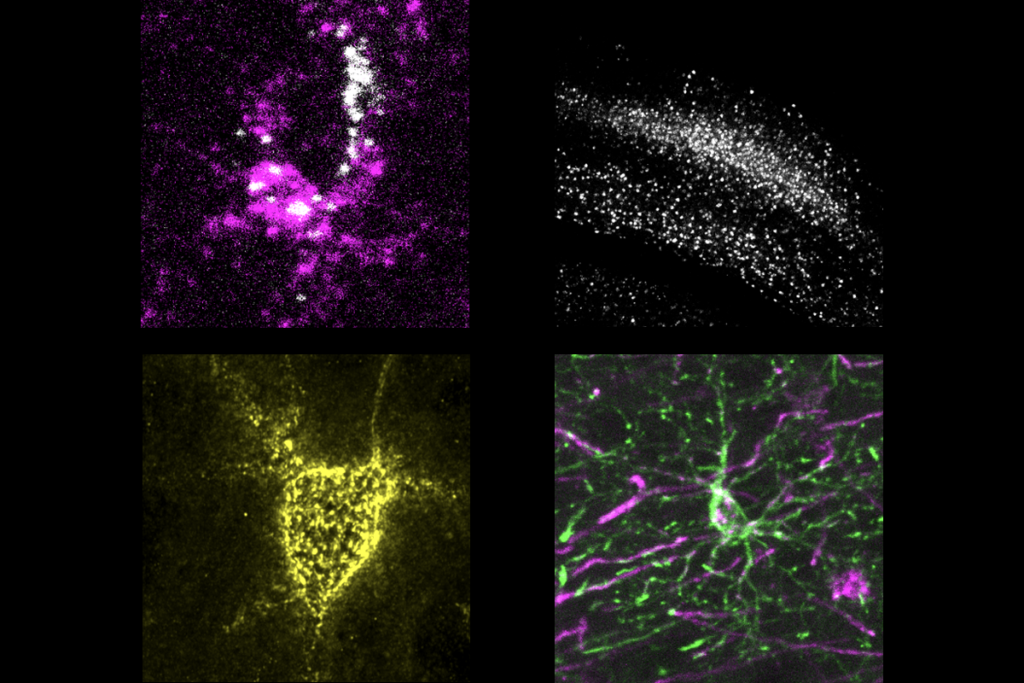
Most recently, Brimberg devised a way to identify at least one of the target neuronal proteins, CASPR2, in fetal brains. When she injected an antibody targeting CASPR2 into pregnant mice, she found that the pups later had structural abnormalities in their brains — their neurons had fewer branches — and behaviors reminiscent of autism, such as impaired sociability. If this protein is involved in autism, Diamond estimates that it could be responsible for up to 4 percent of cases. Notably, CASPR2 is not on Van de Water’s list of seven proteins, which strongly suggests that more possible protein targets for maternal antibodies will be identified in the future.
”"I worry about this … There are real-world consequences.” Emanuel DiCicco-Bloom
Preventing autism?
Another line of research traveling a different path through the immune system has arrived at a similar pattern of results. Some studies showed that a pregnant woman who has a viral infection has an increased risk of having a child with autism. These were retrospective, asking women sometimes years after the fact to report any illness during their pregnancy. A 2014 Swedish study was more persuasive because it followed the outcomes of more than 2 million births, confirming that an infection requiring hospitalization during pregnancy increases the risk of having a child with autism by more than 35 percent — even though the overall risk is still quite small.
Viral infections such as the flu set off a surge of cell-signaling cytokines, and neurobiologist Paul Patterson at the California Institute of Technology in Pasadena, an early pioneer in this research, became curious about the connections between viral infections and brain development. Working in mice, Patterson’s lab mimicked viral infection in pregnant animals, stimulating their immune systems and causing behavioral deficits in the pups. In studying these pups, Patterson zeroed in on a particular cytokine called interleukin-6 (IL-6) that he linked to their abnormal behavior.
Patterson died in 2014, and Dan Littman, a neuroimmunologist at New York University, picked up where Patterson left off. Littman’s team was already studying a type of T cell called T-helper 17 (Th17) that is one of several created in response to the surge in IL-6 during an immune response to infection. Th17 cells help preserve barrier surfaces such as skin and intestinal linings. In January, Littman’s team showed that a cytokine called IL-17A, made by Th17 cells in response to an infection, crosses the developing blood-brain barrier of the fetus, acts on receptors in the fetal brain, and causes a malformation in the one region of the developing brain. The researchers also saw autism-like behaviors in mouse pups exposed in utero to IL-17A. “It’s probably changing the way that the circuitry of the neurons is laid out during development and that leads to the behavioral deficit,” says Littman. When he and his colleagues treated pregnant mice with an antibody that neutralizes IL-17A, their pups did not show any behavioral changes.
There is a major caveat to this work, says Littman: “Whether this occurs in humans, we have no idea.”
Still, there are grounds for optimism. Last year, the U.S. Food and Drug Administration approved an injectable drug that neutralizes a form of IL-17 to treat people with psoriasis; more than 80 percent of the people who received the drug have seen positive results. “It’s revolutionized the treatment of psoriasis,” says Littman. In the past two decades, drug developers have become expert at inventing therapies that target cytokines: Drugs such as Humira, which is used to treat rheumatoid arthritis, Crohn’s disease and other autoimmune diseases, are a major pharmaceutical success story. So it might be possible one day to interfere with cytokines that target the developing brain.
However, cytokine-inhibiting drugs can have serious side effects. It’s also not clear how drug developers would be able to achieve Diamond’s vision of an antibody-blocking drug that can be taken safely by a woman who has these antibodies and is hoping to get pregnant. “That’s the fantasy,” she says. “I’m hoping it’s not that hard. We have our ideas of how to do it.”
The test:
Van de Water can take much of the credit for the growing acceptance of the role of the immune system in autism. “She has made an enormous contribution,” says Zimmerman. But clinicians are still wary of an antibody-screening test. They question what they would tell women based on the results of the potential Pediatric Bioscience test, which is not yet on the market. “Predictability is the key,” says Zimmerman. It’s not enough, in other words, to say that a woman has some of the antibodies in question if you can’t also tell her what that means for her risk of having a child with autism. Those answers will come only with prospective studies, the kind that follow women before, during and after pregnancy and track the health of both mother and child. Several such studies, including two conducted by Van de Water’s lab, are underway.
“A fundamental issue has been the rapidity between raising a possibility and talking as though it’s fact,” says Emanuel DiCicco-Bloom, a pediatric neurologist at Rutgers Robert Wood Johnson Medical School in New Jersey. “I worry about this because parents ask me whether they should be treating their kid with this or that, or shouldn’t get pregnant again. There are real-world consequences.”
Van de Water says many doctors and reporters misinterpreted the news of her relationship with Pediatric Bioscience. “You license early,” she says. “The issue that arose was the misunderstanding between academia and industry about what it takes to go to market with a test; it’s a long, slow process of validation and verification.” She says that the intention is for the test to be used initially as a postnatal screen for antibodies in women as an early warning sign that a child should be monitored closely, perhaps leading to earlier diagnosis and therapy.
Eventually, though, the test would be used to assist with family planning. Van de Water argues that families deserve as much information as scientists can give them. She points out that antibody screening would only suggest whether women are high- or low-risk for having a child with autism: “What it gives families is a tool to make what is quite often a very difficult decision.”
Parents desperate for answers are some of Van de Water’s biggest supporters. Having one child with autism raises the risk of having another by 20 percent, so many families welcome any way to get a clearer sense of the odds.
Steve White, of Hayward, California, decided to participate in Van de Water’s antibody study after his third child, Herbie, was diagnosed with autism, even though he and his wife weren’t planning to have any more children. His wife tested positive for two of Van de Water’s seven antibodies. “I can’t say it solved any problems we had, but we were very glad to have answers,” says White. And a 30-year-old mother, Elise, who did not want to give her full name for privacy reasons, says that with a history of miscarriage and one son with autism, her negative results — she had none of the seven antibodies Van de Water has identified — helped her and her husband decide to try to have a second child. “We know it’s not a guarantee, but it’s nice to have one less thing to worry about,” she says.
Van de Water says she regularly gets emails from women asking when the antibody test will be ready. She knows of families who have one child with autism who have opted to use surrogates, for fear that a second child will also have the condition. Even women long past their childbearing years ask if they can be tested. “They just want to know,” she says.
Van de Water says her dream is that her work, combined with efforts to create drugs that protect against maternal antibodies, will one day make it possible to restore the fragile truce between a woman’s immune system and her growing fetus. “That would be amazing.”
Recommended reading
Explore more from The Transmitter

Neuro’s ark: How goats can model neurodegeneration