The deep emotional ties between depression and autism
Autistic people are four times as likely to experience depression over the course of their lives as their neurotypical peers. Yet researchers know little about why, or how best to help.
I
n June, Nicholas Lyons graduated from a private special-education high school in Maryland. Like many of his classmates, he is unsure what he is going to do next. His mother, Kelly Lyons, is worried, too — but more about his health than his plans: At 18, Nicholas has already endured several bouts of depression, one of which drove him to contemplate suicide.Nicholas was diagnosed with autism at age 9. By 12, the socially awkward, bright boy was in therapy for depression, too. “He was made fun of because he was different. He was smart enough to know that,” his mother says. “It posed a real problem.”
At 13, Nicholas’ mood plummeted further. He disengaged from everyday activities, such as talking with his family at dinner and playing video games, and he began sleeping a lot — common signs of depression. His mother increased his therapy sessions from once to twice a week. Meanwhile, his social problems only grew worse. “The autism caused me to take insults a lot. The insults were harsh,” Nicholas says. “Sometimes the kids made me angry. Sometimes it really annoyed me. The insults made me sad sometimes.”
The bullying got so bad that his mother pulled him out of the public school he was attending. He switched to a private special-education school, where he thrived until about age 17. Then he started worrying about what he would do after graduation. Again, he spiraled into depression, and his psychiatrist prescribed an antidepressant. The drug has helped Nicholas feel “even-keeled,” he says, but he is still anxious that his life is changing.
Nicholas’ ongoing battle with major depression is not unusual for people on the spectrum, according to a meta-analysis of 66 studies published in January: They are four times more likely than neurotypicals to experience depression over the course of their lives, although scientists are unsure why. Their rates of depression rise with intelligence and with age. In fact, says Carla A. Mazefsky, associate professor of psychiatry and psychology at the University of Pittsburgh in Pennsylvania, more than 70 percent of autistic youth have mental health conditions, including depression and anxiety, and these are thought to often persist or worsen into adulthood.
The consequences for many autistic people are dire. Major depression can severely impair their independence; their coping, daily living and social skills; and their communication — all things they may already find challenging. Depression can also trigger suicidal thoughts: Before Nicholas’ mother pulled him out of his public school, he had intended to end his life, she says.
Despite this grave set of circumstances, there is little hope available. There are no studies on which screening measures are most useful or which treatments work best to ease depression among autistic people. It is not known, for example, whether depressed autistic people respond differently to psychotherapy than others do, or how best to adapt treatments such as cognitive behavioral therapy for them. Talk therapy, in particular, may not work well for autistic people, because they can struggle with social communication and with identifying their feelings, a trait known as alexithymia.
It is also unclear what effect medications for depression have on people on the spectrum. “They may have more side effects and more difficulty,” says Jeremy Veenstra-VanderWeele, a child and adolescent psychiatrist at Columbia University in New York. Antidepressants can even disrupt autistic children’s sleep and make them more impulsive, potentially outweighing any benefits, he points out.
In addition to developing better screening tools and treatments for depression in autistic people, researchers are trying to get at the root causes involved. The origins of the overlap have not been easy to trace. “Despite us knowing that depression among people on the spectrum is a common problem, in truth we know alarmingly little about depression and autism,” Veenstra-VanderWeele says. “The whole field is moving very slowly.”
Underpinnings of depression:
P
sychiatric disorders such as depression usually arise from some mix of genetic and environmental factors. At this point, researchers don’t know how autism figures in that mix, says Lisa Gilotty, an autism expert at the National Institute of Mental Health. According to one study last year, unaffected siblings of autistic people are at a roughly 40 percent increased risk of depression relative to the general population, suggesting a role for genetic factors.For others — especially autistic youth such as Nicholas who have few support needs — depression can result from bullying, isolation or other social problems. One study found that loneliness is the strongest statistical predictor of depression. “Getting your social needs met is important — autism can get in the way of that,” says clinical psychologist Katherine Gotham, who led the study.
Rumination — repetitive thinking about negative events and emotions — can also set some autistic people up for a depressive episode, according to research presented in May at the International Society for Autism Research conference. Many autistic people have repetitive behaviors and intensely focused interests, and it can be detrimental to their mental health if that focus turns to sad or undesirable experiences. “It is not rare to experience trauma and adverse events if you’re on the spectrum; this contributes to depression among individuals with autism, too,” Gotham says.
People with autism may be especially prone to dwell on negative emotions, she says. Autistic adults react faster to photos of sad faces than to photos of neutral ones, as measured by their pupil response, for example. And depressed autistic adults fixate on angry and sad faces, and spend more time overall looking at sad faces, compared with either neurotypical depressed people or non-depressed people. “What this says is that if we can find strategies that could effectively redirect people with autism from dwelling on negative information, it can help them develop a more adaptive pattern of thinking,” she says.

Some of those strategies may be no different from what works for typical people: Social support and supported employment programs guard against depression and suicidal ideation in neurotypical people, and studies show that they do so in autistic individuals too.
The right kind of job support helped Sean Boogaard, 47, of Jacksonville, Alabama, pull out of his recurring episodes of depression. Boogaard was diagnosed with autism almost five years ago but says he always had trouble communicating, which he says probably cost him several jobs. “I had trouble reading body language like if someone was mad,” he says. “I was doing everything right, yet still getting negative reactions that I never understood. I didn’t get second chances like many people do.”
Boogaard was married for five years in his 30s and says he was “grossly underemployed” during that time. He struggled with depression then, and when his marriage ended, it became worse. “It was all situational,” he says. After his autism diagnosis in 2014, he found a job with his local county, maintaining the road networks and zones that emergency responders traverse. His new supervisors know he has autism, so they are more direct with him when they relay information.
“Things are far better on the job since they know I’m on the spectrum,” Boogaard says. If he does something wrong, his bosses explain what happened and how to fix the situation. “In many places, a corporation will create a list of the wrongs you do until they have enough to fire you rather than giving a chance to make amends,” he says.
Complex clinical picture:
L
ike Boogaard, Becca Lory Hector of Bailey, Colorado, cycled through many jobs as a young adult and didn’t know why. Several therapists had misdiagnosed Hector with schizophrenia and bipolar disorder, and had given her medications that made her feel worse.One day in 2009, when she was 33, Hector decided to quit her job as a bartender and move back in with her mother in Queens, New York. “I climbed into the bed I grew up in and said I give up,” she says. She spent the better part of the next three years hiding under the covers. “The only reason I didn’t take my life is because I was afraid of what it would do to my mom,” she says. At 36, Hector was finally diagnosed with autism, along with anxiety and major depressive disorder: “I felt relieved, validated, and for the first time in over a decade, I felt there was possibly hope for me.”
Many people with autism never get a depression diagnosis, though, or the help they need.
“It’s really hard to assess depression in individuals with autism,” Gotham says. Health professionals may not notice it because depression is an ‘internalizing’ disorder, meaning it is characterized by feelings — such as hopelessness, self-criticism or sadness — that happen internally. And spotting an internalizing disorder is particularly challenging in an autistic person who is not adept at expressing her emotions or nonverbal.
Also, depression is an episodic illness. To spot it over time, clinicians need to stay attuned to their autistic patients, and ask about and look for subtle changes in their functioning, including shifts in their sleep patterns, social activities and appetite.
Compounding those challenges, some signs of depression, such as being socially withdrawn, can be incorrectly interpreted as part of autism. Depression can also manifest as physical complaints that often accompany autism, including fatigue, restlessness and stomachaches. And depression can sometimes exacerbate autism traits, including aggression, self-injury and irritability. The hidden nature of depression and its overlap with autism traits make for a complex clinical picture. Tools to identify depression in autism are still being validated.
In the meantime, mental health professionals and psychiatrists would benefit from training about how to help autistic people. In an unpublished study presented at the International Society for Autism Research conference in May, Brenna Maddox, a postdoctoral fellow at the University of Pennsylvania, and her colleagues found that community mental health clinicians are not always confident in their ability to treat autistic adults. Among the 100 clinicians the team surveyed, 70 had no autistic adults in their caseload, 76 had no formal training in working with autistic adults, and most reported greater confidence in treating adults without autism. These clinicians are “selling themselves short,” Maddox says.
Parents and pediatricians can also be coached to look out for signs of depression in their autistic children, says Sarah Cassidy, assistant professor of psychology at the University of Nottingham in the United Kingdom. In 2018, it became standard for pediatric primary care providers in the United States to screen for depression in all children. Pediatricians should be able to tease out subtle signs of depression because they are accustomed to treating children, many of whom cannot express themselves well or at all, says Edward Lewis, who has practiced as a pediatrician in Rochester, New York, for 38 years. When he needs additional advice, Lewis says, he relies on Project TEACH. Through the program, he is able to schedule a phone consultation with a child psychiatrist from the New York State Office of Mental Health.
Lewis says he has learned that children with autism and depression show a range of warning signs. “Some children with depression can be somewhat irritable and edgy, others can become more agitated and inattentive or anxious,” he says. “There’s no one size fits all; a patient may present with lethargy and no oomph, and sadness. When you look in their face, you can tell they’re depressed.”

Tailoring treatment:
S
potting depression in autistic people is only half the battle. Treating the condition is also less than straightforward, and can present clinicians with difficult decisions.For example, some autistic people, especially children, appear to be at a greater risk of experiencing side effects — including agitation, hyperactivity and aggression — when they take antidepressants. And there have been only limited clinical trials of the efficacy of these drugs to treat depression in autistic people to begin with, says Roma Vasa, director of psychiatric services at the Center for Autism and Related Disorders at Kennedy Krieger Institute in Baltimore, Maryland.
Most clinicians treating autistic people with depression turn instead to adapted psychotherapies, such as cognitive behavioral therapy (CBT), in which therapists help clients to reframe harmful thought patterns. Researchers don’t yet have data on the efficacy of CBT for depression in autism, but the method has been studied to treat anxiety in autistic people and can be adapted, Gotham says. “Unfortunately, we don’t have a gold standard to care for these [autistic] patients yet,” she adds, but she sees no reason to wait: “I think that CBT is unlikely to do actual harm to treat depression in this population.”
Some researchers are exploring ways to modify CBT to treat depression in autistic people. Mazefsky says clinicians could follow a predictable session routine and structure, incorporate a client’s strengths and talents, repeat concepts often and make abstract concepts more concrete via visual aids and worksheets. They could also put greater focus on emotion recognition. Mazefsky has also found that incorporating mindfulness training can help autistic clients improve their emotional awareness.
In December 2017, one small trial found that an adapted, guided self-help form of CBT, called ADEPT, is well received by therapists and by autistic participants with depression. The 70 participants attended nine sessions with a therapist. Instead of leading the sessions, the therapists simply encouraged the participants to investigate any links between the self-help exercises they had completed and how they felt, so that they could make constructive changes in their daily lives. Although the researchers were not assessing the approach’s effectiveness, the trial showed some evidence that the intervention helped improve participants’ mood.
“It is important that people with autism are able to access a range of effective treatment options and make individual choices about the treatment that will be best suited to them,” says Ailsa Russell, a clinical psychologist at the Centre for Applied Autism Research at the University of Bath, in the United Kingdom, who led the ADEPT trial. Guided self-help interventions might help autistic people with depression overcome simple barriers to accessing care, including things such as scheduling appointments and getting out of the house.
Once a person with autism does make an appointment, it is important to individualize the treatment plan to that specific person and the idiosyncrasies of her particular version of the condition. Hector’s therapist helped her understand what an autism diagnosis meant to her and how the condition shaped her life. The therapist then addressed Hector’s depression.
With ongoing therapy, Hector was well enough to become a neurodiversity and inclusion consultant. She bought a house and, in August 2018, got married. “I never thought I would qualify for a mortgage or get out of New York City. It was a dream of mine since I was 16,” Hector says.
Nicholas is working on some of his own dreams. He is looking for a job and thinking about going to college. His mother says he doesn’t need as much help as he once did. She is trying to take a step back — but says she finds it difficult while he is not taking all the steps he might to move forward.
Still, he is making progress. This summer, Nicholas is doing CBT with his therapist, and he continues to take antidepressant medication. For him, it has not caused any serious side effects. “At the moment, I’m trying to keep myself active so I don’t end up in a slump,” he says. “I like to keep doing things so I don’t feel like I’m not doing anything with my life. I’m planning out a strategy.”
Recommended reading
Explore more from The Transmitter
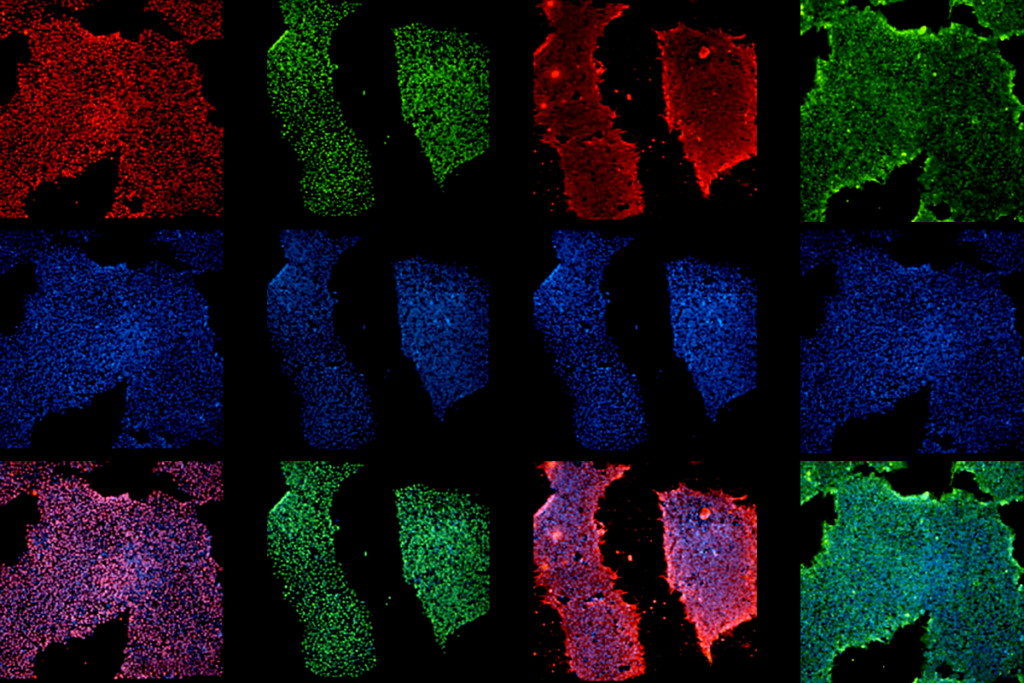
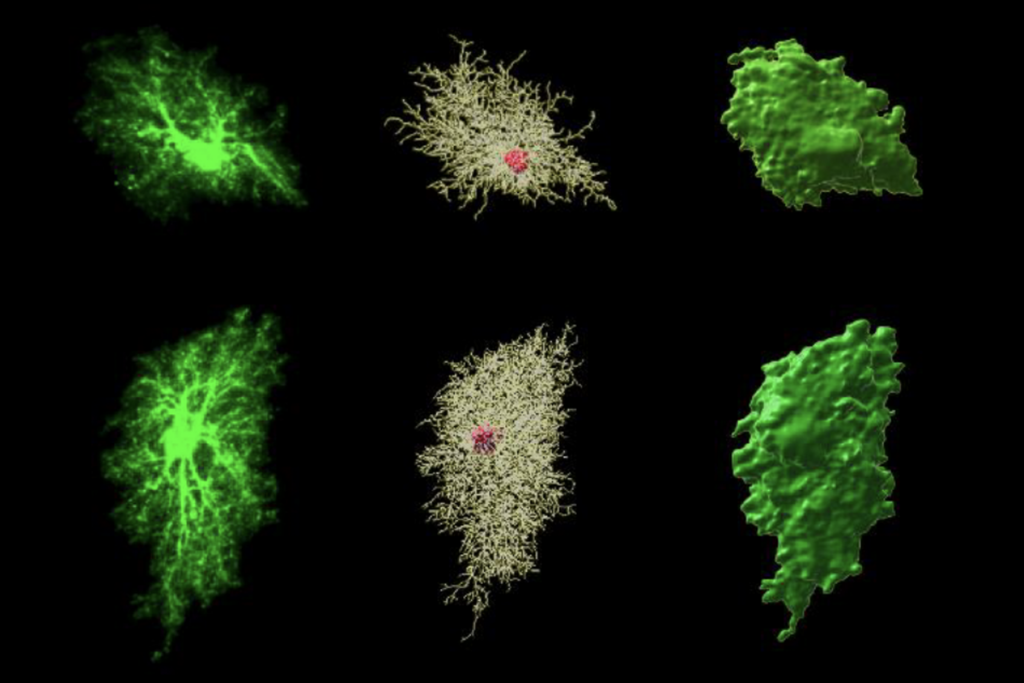
Bringing African ancestry into cellular neuroscience