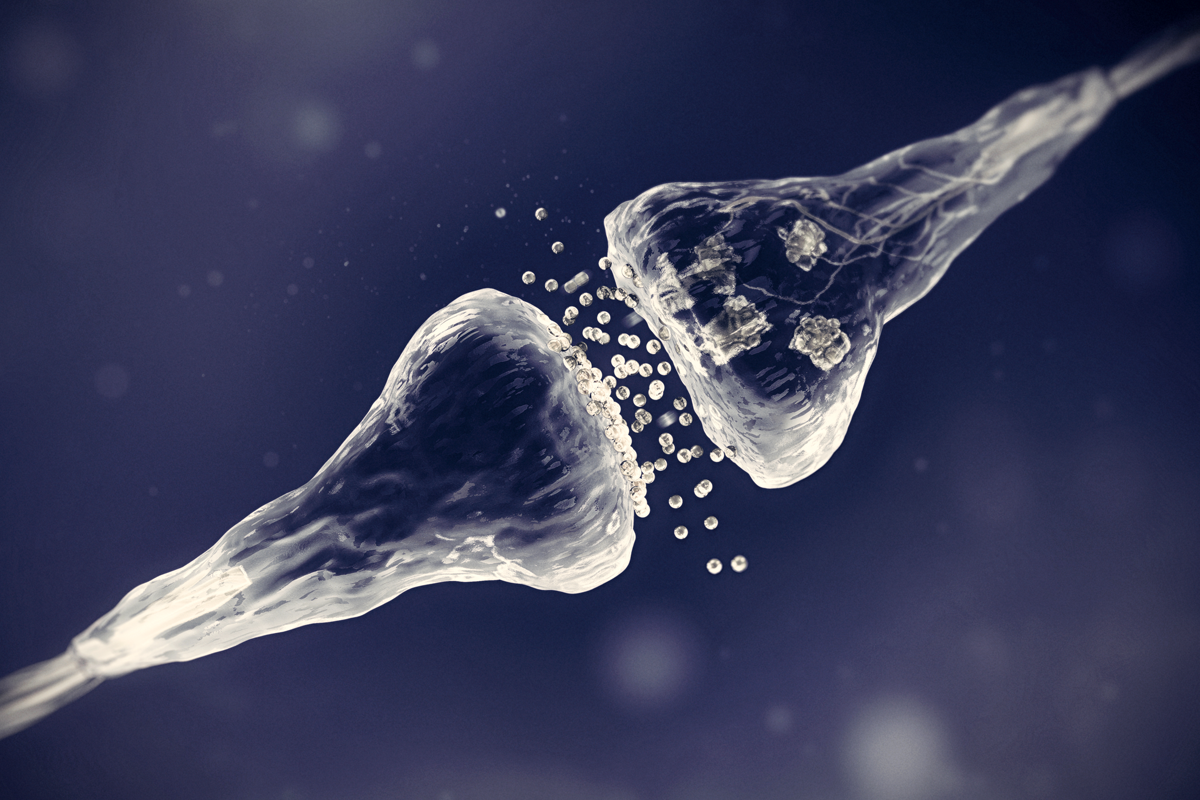
Brain communication relies on a complex set of connections, coordinated by important synaptic proteins. Mutations in one such protein, SYNGAP1, which is critical for brain plasticity, can lead to neurodevelopmental conditions.
SYNGAP1-related intellectual disability (SRID) makes up about 1 percent of intellectual disability cases. It is characterized by seizures, developmental delays and problems with motor coordination. About half of people with SRID have autism.
Recently, a flurry of new SYNGAP1 findings and the development of novel mouse models have expanded scientific understanding of the protein and gene. Together, this work may point to multiple therapeutic possibilities for SRID.
“I think it’s an exciting time,” says Gavin Rumbaugh, professor of neuroscience at UF Scripps Biomedical Research in Jupiter, Florida. “There is a lot of increased interest in SYNGAP.”
For example, past research has indicated that the protein acts as an enzyme to modulate the synaptic connections between neurons. But SYNGAP1 protein may also regulate synaptic plasticity and cognition by physically controlling the number of neurotransmitter receptors at excitatory synapses, according to a preprint posted on bioRxiv in August.
Other work suggests a new role for the gene and protein. In the past, they have primarily been recognized for their effects on synapse functioning. But now SYNGAP1 joins several autism-linked genes that code for synaptic proteins that also shape the developing brain.
A mutation that decreases SYNGAP1 protein levels may exert significant effects on the development of the cortical layers in a human organoid model by disrupting the differentiation of supporting cells that serve as a scaffold for neurons to migrate during development, Rumbaugh and his colleagues have found. Their study was published in Nature Neuroscience in November.
“It’s very important to use model systems to test the function of the proteins associated with disease at different developmental time points and in different cell types,” says lead investigator Giorgia Quadrato, assistant professor of stem cell biology and regenerative medicine at the University of South California in Los Angeles.
A
better understanding of SYNGAP1 may lead to insights into SRID as well. For decades, researchers studied this condition by deleting one copy of the SYNGAP1 gene in mice. These animals have half the usual levels of SYNGAP1 protein and show characteristics of SRID, such as seizures, hyperactivity and faulty learning and memory.In developing human neurons cultured in a dish, a lack of SYNGAP1 leads to increased cell size and dendrite length, and speeds up the onset of synaptic activity.
But it was unclear whether or how small mutations in the gene — the situation typically seen in people with SRID — affect the levels and function of the SYNGAP1 protein, synaptic plasticity and behavior in animals. To address this, lead investigator Richard Huganir and his team at Johns Hopkins University in Baltimore, Maryland, developed two new mouse models.
Each model is based on mutations in the SYNGAP1 gene as they appear in two people — a young boy and girl. “It’s much better to have [models] with patient-based mutations for future therapeutics,” says Huganir, professor of neuroscience.
Using CRISPR, the group introduced the two faulty versions of SYNGAP1 into different sets of healthy mice. Both mutations reduced SYNGAP1 protein levels by about 50 percent compared with those of wildtype mice. And the mice showed changes in the expression of genes involved in synaptic plasticity.
Brain slices revealed that the SYNGAP1 mice also had impaired long-term potentiation, the process by which synapses strengthen to facilitate learning and memory. In line with that finding, these mice less frequently went into the arms of a y-shaped maze they had not recently explored than did wildtype rodents.
That behavior indicates the mice might not recall the arm they were in last, which generally reflects deficits in working memory. The mice also displayed hyperactive and repetitive behaviors, typical characteristics in SRID. The results were published in PNAS in September.
A
he mouse work validates past findings with rodent models — and also offers new insights, says Rumbaugh, who was not involved in this study, though he trained as a postdoctoral researcher with Huganir. For one, it reveals the consequences of single mutations, such as an amino acid change in an area of SYNGAP1, he says.The mice showed altered SYNGAP1 functioning that in turn affected synapse functioning, which, “would suggest it could increase your risk for developing some sort of mental health disorder,” Rumbaugh adds.
This work also reveals that a decrease in SYNGAP1 protein may be a crucial mechanism for the development of SRID. Researchers are already looking for ways to restore the SYNGAP1 protein to treat people with SRID and other neurodevelopmental conditions.
For example, one antisense oligonucleotide — a short molecule of DNA or RNA — increased the levels of SYNGAP1 in mice in a study published in Neuron in March. Yet another approach to intervention could involve new molecular technology that binds to mRNA and regulates gene expression. The resulting tool brings together the protein-producing machinery for a specific gene, according to a study published in Nature Communications in October.
With this technology, it is possible to elevate SYNGAP1 protein levels in neurons derived from induced pluripotent stem cells that lack one copy of the gene. The approach may open a new avenue for treating conditions such as SRID that are caused by the absence of a functional gene.
“[SRID] kids have no direct treatments,” says study investigator Bryan Dickinson, professor of chemistry at the University of Chicago in Illinois. “There is a critical unmet medical need.”
The new mouse strains also offer important therapeutic possibilities. “These are actual patient mutations, and that is really cool,” says Jill Silverman, professor of psychiatry and behavioral sciences at the University of California, Davis MIND Institute, who was not involved in any of the recent studies.
“It’s very innovative and important for precision medicine,” Silverman says. “The sky is the limit.”