Supplements, worms and stool: How families are trying to game the gut to treat autism traits
Scientists are playing catch-up as microbiome-based treatments for autism proliferate.
E
very two weeks, Alex Chinitz swallows the strangest of brews: fruit juice with 20 to 30 larvae of Hymenolepis diminuta mixed in. That fancy Latin word is the name of a helminth — a tapeworm, to be precise — that can grow to 30 centimeters.The larvae Alex drinks are not visible, nor can he taste them. They are encased in tiny cysts, and under a microscope, they look like seeds — only with eyespots and tails. By the time they reach Alex’s mouth, they have already passed through several other organisms: The adult parasites lay eggs in rats’ intestines; the rats excrete the eggs; beetles eat the rats’ feces; and inside the beetles, the eggs hatch into larvae. After Alex swallows them, the larvae swim around in the lumen of his gut and die about 10 to 14 days later.
Alex, 25, is autistic and nonverbal, so he cannot tell us what he thinks of this concoction. But his mother, Judy Chinitz, gives it full credit for having eased some of Alex’s autism traits.
In fact, this drink is only the latest in a series of ‘helminth therapies’ she has tried. “It was affordable, and the side-effect profile is minimal to none,” Chinitz says. She helps run a company in the United Kingdom, Biome Restoration, that distributes the larval cysts to thousands of customers worldwide. Regulations in the U.K. prevent company officials from asking their customers how they are using the product. But, as many online forums attest, scores of people are turning to worms such as these to treat autoimmune conditions, severe allergies, digestive complaints, mood disorders — and autism.
Chinitz came to this unusual treatment after years of seeking relief for her son. When Alex was a child, his chronic inflammatory bowel disease (IBD) was so debilitating that he was dependent on steroids to keep it in check; he took six different medications at one point. He often isolated himself, preferring to sit alone in his sensory swing than to spend time with others.
Improvement in his gut health came when Alex was nearly 10, after his mother changed his diet, cutting out grains and processed sugars. But she was intrigued to see whether helminths might have an even greater effect.
She first read about ‘helminth therapy’ in 1999, when Alex was 5, in a news article. “It still hangs in a frame above my desk,” she says. But it took her years to figure out how to procure the worms. Helminths are not exactly stocked in pharmacies, and their manufacture, distribution and importation is illegal in the United States. Eventually, though, when Alex was 13, she found a Thai supplier, now called Tanawisa. She spent $6,000 on a six-month supply of Trichuris suis ova — eggs of whipworms that typically live in pigs — and took a risk having them shipped to her home in New York.
Alex began ingesting about 2,500 invisible eggs in a small drink every two weeks. About 14 weeks later, Chinitz says, she noticed that her son no longer wanted to be by himself. It was like a “happy pill,” she says. “He was responding so beautifully to it, I went into a panic because I couldn’t afford to keep it up.” And so began their journey with helminths.
Despite her conviction, there’s no proof that these treatments work. A colonoscopy has shown that Alex’s IBD is in remission, Chinitz says, but there’s no evidence of any change to his brain; as for his behavior, he may have felt more social after ingesting the whipworm eggs simply because his stomach hurt less. Anecdotally at least, his story resonates with many others who report relief from some autism traits after helminth therapy. In a 2017 survey of physicians monitoring 700 helminth users, more than half of the users have autism and the majority have had a favorable response, says William Parker, a researcher at Duke University in Durham, North Carolina, who led the survey. “The helminths are definitely helping some of the kids.”
Proponents of the approach offer this as a biological rationale: Treatments that shake up the balance of organisms in the gut are known to affect the brain. Almost 20 years ago, for example, researchers noticed that antibiotics could bring about short-lived improvements in autistic children who had lost their language abilities and social skills. I take parasitic worms for my ulcerative colitis, a form of IBD. A regular influx of hookworms seems to keep my disease in remission, but I previously tried Trichuris suis to no effect.
The idea of helminth therapy leans heavily on the ‘old friends’ hypothesis: Through most of our evolutionary history, we humans have shared our bodies with a host of bacteria, viruses and parasites; exposure to these organisms primed our immune system and kept it humming, like a finely tuned instrument. Now, however — thanks to modern hygiene, the widespread use of antibiotics and, to some extent, pollutants — we live without that same microbial mix. And as a result, or so the theory goes, our immune system can go haywire, leading to autoimmune disorders, allergies and some brain conditions. Autism isn’t typically thought of as an immune condition, but there is evidence that immune dysregulation and inflammation play a role in some cases.
Research on the microbiome — the collection of microbes that live in and on the body — is still in its infancy, says Mauro Costa-Mattioli, professor of neuroscience at Baylor College of Medicine in Houston, Texas. Just the idea that microbes could influence the brain was “unthinkable a few years ago,” he says. The pace of research has accelerated over the past few years, but microbe-based medicines are not yet in sight.
Still, many parents and clinicians are not waiting. A growing number are experimenting with specialized diets, probiotics, stool transplants and parasites, trying to game the gut to address core autism traits. About 19 percent of physicians surveyed in 2009 said they recommend probiotics to the autistic people they treat. An unpublished survey of 100 people found 2 adults trying stool transplants at home for autism.
These unregulated therapies can be costly and unpredictable — and they pose significant, even life-threatening, risks. Home-grown stool transplants and parasites, for example, can introduce deadly infections. This month, the U.S. Food and Drug Administration issued a safety alert about fecal transplants after two recipients contracted an antibiotic-resistant infection and one of them died.
Given the public’s interest in these therapies, researchers should “speed up the process, as far as investigating and understanding why,” says Chiazotam Ekekezie, who led the survey of 100 people when she was chief medical resident at Rhode Island Hospital at Brown University. “Rather than [have] people taking it into their own hands, maybe we can standardize it and make access equitable and safe.”
The baseline:
T
he interest in the microbiome’s role in autism is justified: Children on the spectrum are at least twice as likely as their typical peers to have digestive problems; they are also more prone to a range of stomach complaints, including diarrhea and constipation, which may result from eating a restricted diet. Multiple studies show that autistic children have an altered microbiome compared with typical children. However, the studies are mostly small and uncontrolled — and it’s not clear what they mean, given that researchers are still trying to establish the ingredients of a healthy microbiome. The research also doesn’t begin to indicate whether differences in autistic children contribute to their behavior or are instead a consequence of their condition.To get at this chicken-or-egg question, some researchers have turned to animal models. In a series of experiments reported this year, California Institute of Technology microbiologist Sarkis Mazmanian and his colleagues took stool from autistic children and controls and injected the samples into mice that lack a microbiome of their own. Compared with controls, the mice that received an autistic person’s microbes showed what might be construed as autism-like behaviors: They vocalized less than control mice, spent less time interacting with other mice and showed an increase in repetitive behaviors, such as burying marbles.
The result suggests that the microbiome contributes to autism-like behaviors, Mazmanian says. But marble-burying in mice is a far shot from autism traits in people. The team also analyzed the chemicals the microbes produced: These metabolites are one of several lines of communication between the brain and gut. In a 2013 study, they found that one particular chemical, called 4EPS — which is elevated in mice with autism-like traits, according to previous work — induces anxiety but not any other autism-like behaviors. In the more recent study, two other molecules seem to ease repetitive behaviors in the mice and make them more sociable.
The latest work came under heavy criticism from experts who pointed out that the animals’ behavior varied significantly and they did not respond consistently. Some mice that got ‘autistic’ stool, for example, acted no differently than control mice. Others have pointed out possible statistical errors in the analysis.
Still, Mazmanian says the work suggests overall that metabolites produced by bacteria can influence behavior, at least in mice, and that the data so far show the tip of the iceberg. He says he and his colleagues have identified many other metabolites that they have not yet had the time or resources to explore. “Just studying this one metabolite, 4EPS, has taken us seven years,” he says.
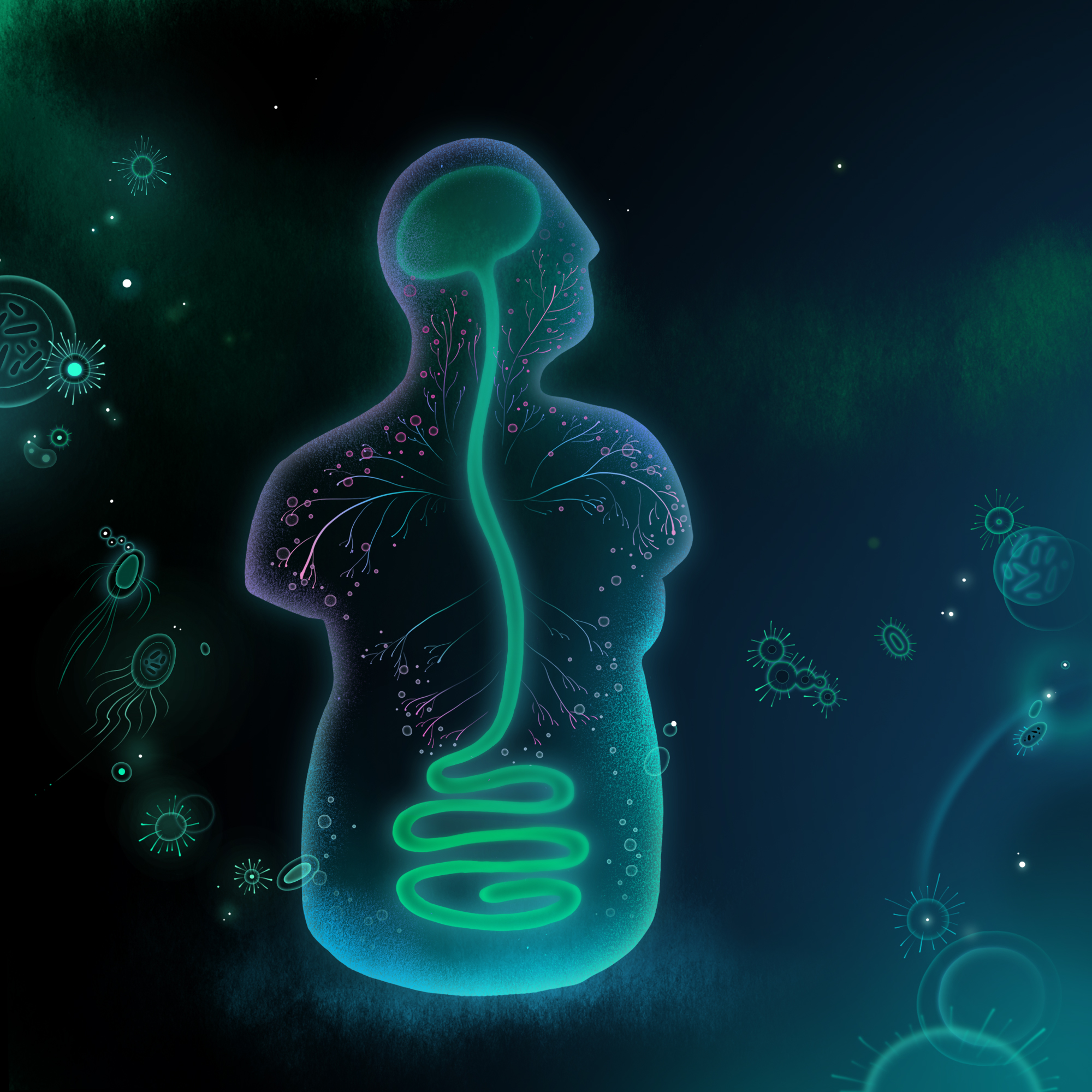
The mechanisms involved in brain-gut communication are many and layered. The vagus nerve, for example, connects the brainstem to the visceral organs; signaling molecules in the immune system, as well as hormones and neurotransmitters, can all modulate messages traveling back and forth. Costa-Mattioli has focused on a single species of gut bacteria, Lactobacillus reuteri, found in yogurt and commercial probiotics. In 2016, his team found that these bacteria seem to restore sociability in pups born to obese mice.
In a follow-up study last year, the team tested L. reuteri in three mouse models raised without a microbiome. Again the bacteria restored the mice’s social behaviors — but only under certain conditions. “We were very surprised to find that when we cut the vagus nerve, the bacteria were no longer able to reverse the social deficits,” Costa-Mattioli says. The mice also did not respond if the researchers knocked out their oxytocin receptors in the brain. Costa-Mattioli speculates that L. reuteri produces a metabolite that activates the vagus nerve to promote oxytocin, the ‘cuddle hormone.’ This hormone then turns on the brain’s reward center for social behavior. Impeding the message at any point along this relay — from bacteria to metabolite to vagus nerve to oxytocin receptors — impairs the animals’ sociability, but Costa-Mattioli points out that other microbes may also produce this same factor or metabolite.
“I don’t want to claim that it is the only one,” he says.
From mouse to person:
E
ven if it were possible to change the social behavior of mice with a single microbe or microbe product — and that’s a big if — people are considerably more complex in terms of brain, behavior and gut bacteria.For these reasons, it has proved challenging to manipulate the human gut effectively. Perhaps the most straightforward approach involves diet, nutritional supplements and prebiotics, the fibrous food that feeds bacteria. One small, randomized trial suggested that a gluten-free, casein-free, soy-free diet, along with certain nutritional supplements such as essential fatty acids, improves autism traits. But there is little evidence from systematic reviews that diet has any real effect on the condition.
Some clinicians aim to curate the microbiome by introducing ‘good’ bacteria in the form of probiotics. Many probiotics are available over the counter, but again the scientific literature on these products is mixed. Some analyses suggest probiotics can improve conditions such as irritable bowel syndrome, but there is little research on how they affect autism traits.
A more direct route is fecal transplants. Think of probiotics as importing single plants into a vast jungle. Diet and supplements only prime the soil; a fecal transplant is like replacing the entire jungle.
A small open-label study from 2017 tested daily fecal transplants from typical children to 18 autistic children. “One of the exciting things we saw was that there were improvements in gastrointestinal symptoms and also on behavior and on the microbiome at 10 weeks, but many of those improvements remained or even got better at 18 [weeks],” says lead researcher Rosa Krajmalnik-Brown, professor of civil and environmental engineering at Arizona State University in Tempe. A follow-up study in April showed many of those same improvements persisted two years later.
Critics point to the study’s small size and lack of controls, but Krajmalnik-Brown says the team is working on a larger blinded trial in which half the participants will receive the treatment and half a placebo. They hope to recruit more than 80 autistic adults.
Helminth therapy is among the most obscure of these approaches targeting the microbiome. The idea to test it for autism started in 2005 with Lawrence Johnson, a now 28-year-old autistic man who was prone to aggressive outbursts and self-harm as a child. Lawrence’s behavior abruptly changed one summer when he was 13 years old and attending a summer camp for special-needs children. The counselors called his father, Stewart Johnson, to report that the boy was suddenly calm and more interactive.
When Johnson went to pick Lawrence up, he noticed his son had bites from chigger mites all over his legs. “It was too coincidental; there had to be some kind of connection,” Johnson recalls thinking. He wondered if that connection might involve the immune system — Lawrence’s behavior also seemed to improve whenever he had a fever and his immune system was fighting an infection. Lending further credence to the idea, Lawrence reverted to his usual behavior when the bites cleared up 10 days later.
Johnson did a little reading and, like Chinitz, came across Trichuris suis therapy. He brought it to his son’s doctor, Eric Hollander, director of the Autism and Obsessive Compulsive Spectrum Program at Albert Einstein College of Medicine in New York City. Hollander started Lawrence with a three-month dose, having the boy swallow the eggs in a drink every two weeks. The effects were rapid and striking, Johnson says: “It was just remarkable; it was back to all the good stuff that we saw.” Hollander, too, recalls a marked improvement in terms of Lawrence’s aggression, self-injury and openness to changes in his routine, adding that “it was easier for the family to travel with him.”
Last year, Hollander and his colleagues published a small trial of helminth therapy in 10 autistic adults. To increase their odds of seeing a response, they selected participants with a personal or family history of autoimmune problems, such as allergies. After 12 weeks of the treatment, they measured the therapy’s effect on certain autism traits. Overall, the participants showed fewer repetitive behaviors and less behavioral rigidity and irritability. The next step, Hollander says, is to identify biomarkers to group the people and traits that are most likely to respond to these therapies.
Inflammatory pathways do not play a role in all autistic people, Hollander says, but it may be that repetitive behaviors and rigidity, for example, are particularly amenable to modifications of the microbiome or the immune system in some people. “It’s possible that there may be different therapeutics for the repetitive behaviors than there might be for social communication,” he says.

The biome business:
I
f these lines of research pan out, doctors may one day be able to treat autism with a combination of drugs, some targeting the microbiome.A plethora of biotech companies are trying to engineer or cultivate the perfect mix of gut microbes or even small molecules that manipulate gut microbes as treatments for autism and other conditions. In February, for example, Boston-based Axial Biotherapeutics Inc., co-founded by Mazmanian, raised $25 million in a second round of funding to develop gut-targeted small molecules to treat Parkinson’s disease and autism.
To date, though, pharmaceutical companies have not shown much interest, perhaps because questions of regulation bedevil such therapies. And although the Food and Drug Administration has approved fecal transplants under close supervision to treat people with deadly Clostridium difficile infections, they have yet to rule on stool for other purposes, such as IBD. Krajmalnik-Brown and her colleagues hope to develop microbial cocktails that can be administered orally, which might make the approach easier to deliver and regulate.
The challenge of standardization also makes helminths harder to bring to market. Companies have shown little interest in parasites since a clinical trial of Trichuris suis ova to treat Crohn’s disease, a type of IBD, fizzled out in 2014. German biotech entrepreneur Detlev Goj, who was involved with those trials and co-founded the Thai helminth distributor Tanawisa, is attempting to get the eggs regulated as a medical food in Europe. If he succeeds, the eggs would be available in supermarkets there, alongside probiotic drinks. Eventually, Goj hopes to have the helminth eggs regulated as a supplement in the U.S.
In the meantime, families continue to fumble with supplements, stool and worms at home, largely by trial and error. According to groups on Facebook and elsewhere, some worms work better for some people, and others have side effects, including rashes, body aches and diarrhea. And then there’s the worms’ cost and lack of easy availability — not to mention the ick factor.
Lawrence Johnson ingested Trichuris suis eggs for seven years, but they were expensive and lost effectiveness over time, his father says. Alex Chinitz also stopped taking the eggs after that initial dose because of the cost. His mother bought a supply for Alex whenever they could afford it. In between, she had him try another worm, Necator americanus. Unlike Trichuris suis or Hymenolepis diminuta larvae, which pass through the gut but typically do not infect people, the larvae of the parasite N. americanus burrow into the skin and colonize the junction between the small and large intestine. To procure these worms, Chinitz, her two children and parents all traveled to Mexico, under supervision from Alex’s doctor. Within months, however, Alex had to abandon the treatment, which had not worked well thus far, because he developed a terrible rash. Eventually, they found the Hymenolepis diminuta he currently takes.
These days, Alex eats a normal diet and his IBD symptoms have been in remission for more than a decade. He enjoys eating out, listening to music and traveling, and he is a “very happy young man,” Chinitz says. And every two weeks, his special larvae-laden drink awaits.
Syndication
This article was republished in The Atlantic.
Recommended reading

New organoid atlas unveils four neurodevelopmental signatures

Glutamate receptors, mRNA transcripts and SYNGAP1; and more

Among brain changes studied in autism, spotlight shifts to subcortex
Explore more from The Transmitter
Can neuroscientists decode memories solely from a map of synaptic connections?

AI-assisted coding: 10 simple rules to maintain scientific rigor
