
Studies spotlight role of medicines, hospitals in autism
People with autism who have a mood disorder or sleep problems are more likely to be admitted to inpatient psychiatric units than those who do not have one of these other conditions.
People with autism who have a mood disorder or sleep problems are more likely to be admitted to inpatient psychiatric units than those who do not have one of these other conditions1. Nearly all individuals with autism who are hospitalized take prescription drugs, but one in three of them stops taking the drugs soon after discharge2.
The findings stem from two studies using data from the Autism Inpatient Collection, a repository of medical information and biological samples from individuals aged 4 to 20 who had been in psychiatric units. Many of these individuals have intellectual disability and problem behaviors, such as self-injury, that can lead to hospitalization.
In one study, the researchers compared records from 218 young people in the collection to those from 255 individuals of similar age in the Rhode Island Consortium for Autism Research and Treatment who were never hospitalized.
The analysis indicated that having a mood disorder such as depression or bipolar disorder increases the odds of being admitted to a hospital sevenfold. Sleep problems, such as insomnia, double the odds of hospitalization. Every increase of a single point on a scale of social communication difficulties raises a person’s odds of hospitalization by 13 percent.
Being aware of these risk factors may help clinicians “decrease the likelihood of a crisis or postpone it by a period of time,” says Giulia Righi, assistant professor of psychiatry and human behavior at Brown University in Providence, Rhode Island, who co-led the study.
Having parents who are married or in a domestic partnership, and having good ‘adaptive’ skills such as getting dressed or bathing, lowers the odds of hospitalization, the researchers found. They speculate that a two-parent household may be less cash-strapped or less stressed by caregiving, which could help a family avert crises that require a hospital stay.
Medication mystery:
Both new studies focus on the severe end of the spectrum, which has historically been underrepresented in autism research, says James McPartland, director of the Yale Developmental Disabilities Clinic, who was not involved in the research. “These are some of the people who are in the most dire need of help.”
The second study examined medication use among 350 people from the collection before, during and after hospitalization.
The researchers analyzed participants’ medical records for six classes of psychotropic drugs, a diabetes drug and medications for gastrointestinal problems. They then followed up with participants in person or over the phone to find out which drugs they continued to take two months after discharge.
More than 91 percent of the participants were taking at least one drug when they were admitted to the hospital. This proportion rose to 97 percent at the time of discharge.
Surprisingly, only 64 percent of the study participants reported taking a drug two months after they left the hospital. That’s a “steep drop,” says study investigator Craig Erickson, associate professor of psychiatry at Cincinnati Children’s Hospital Medical Center.
“We really need to figure out why that’s happening,” Erickson says. It’s possible that some participants improved and no longer needed the medications. But Erickson says other factors, such as insurance barriers and side effects, may be at play.
References:
Recommended reading
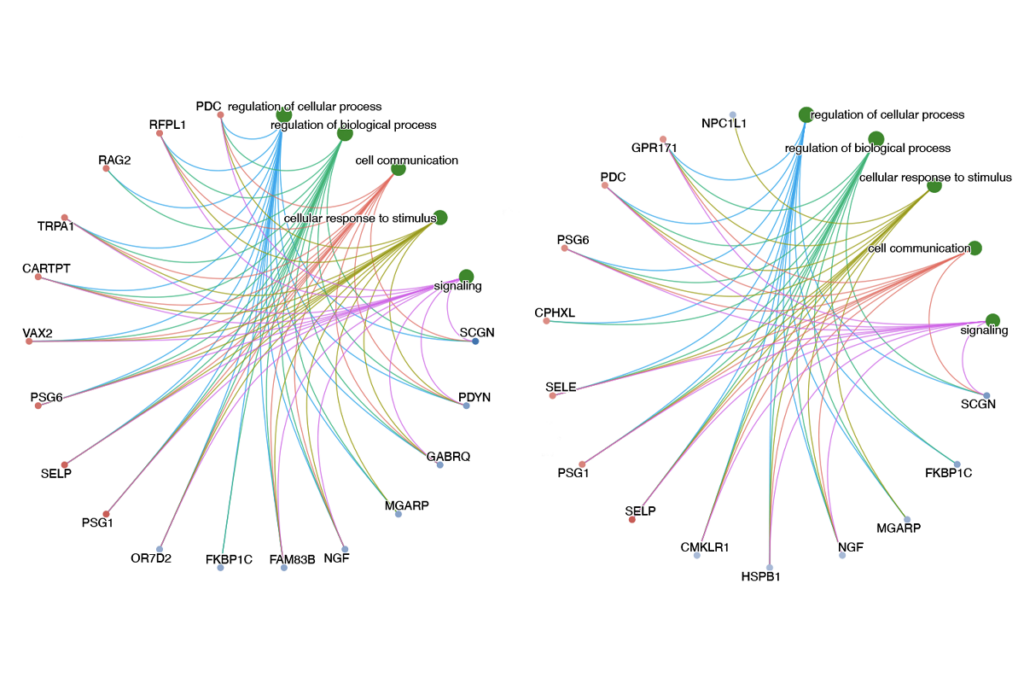
New tool may help untangle downstream effects of autism-linked genes
NIH neurodevelopmental assessment system now available as iPad app
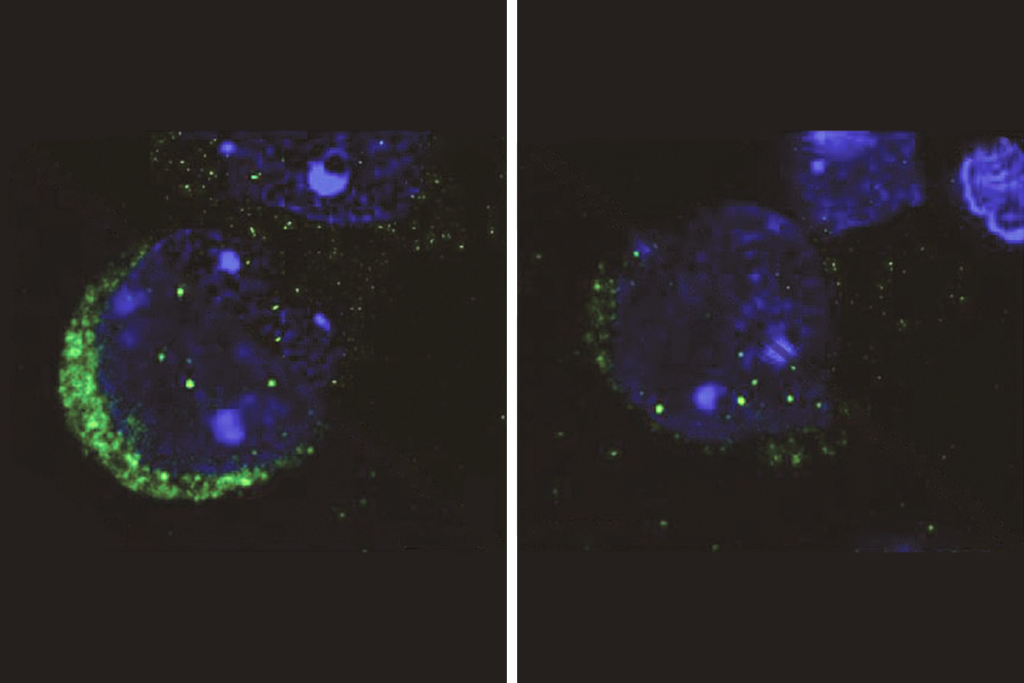
Molecular changes after MECP2 loss may drive Rett syndrome traits
Explore more from The Transmitter
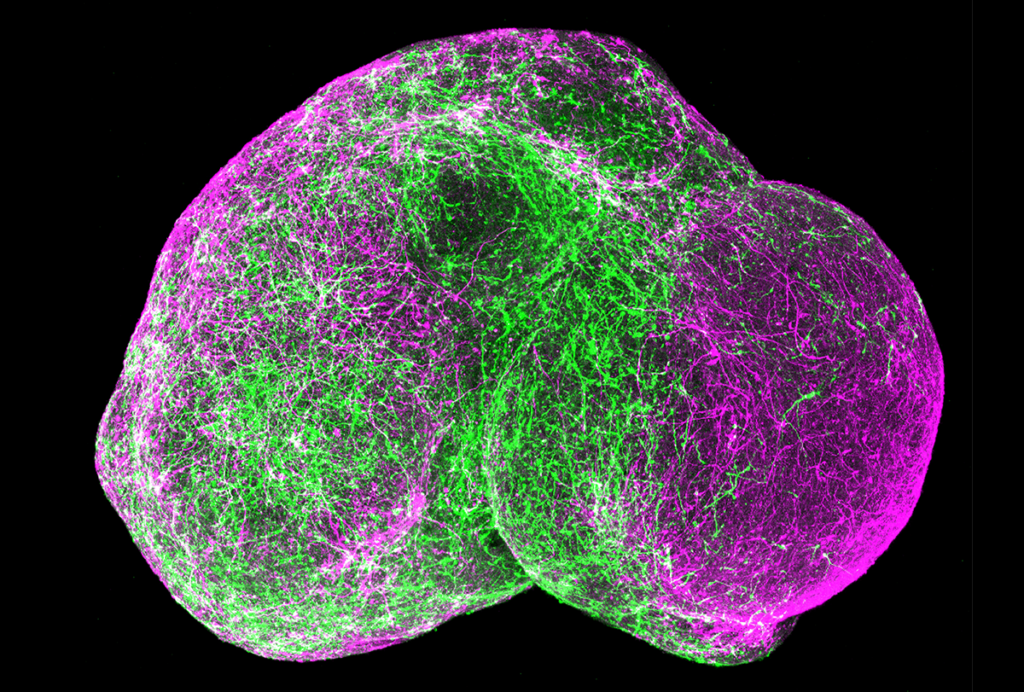
Organoids and assembloids offer a new window into human brain
Who funds your basic neuroscience research? Help The Transmitter compile a list of funding sources
