Sleep, mood woes weigh on obese children with autism
Adding to the complications of autism, overweight and obese children with the disorder are prone to a host of other troubles, including depression, anxiety and sleep problems, reports a study published 2 February in the Journal of Autism and Developmental Disorders.
Adding to the complications of autism, overweight and obese children with the disorder are prone to a host of other troubles, including depression, anxiety and sleep problems, reports a study published 2 February in the Journal of Autism and Developmental Disorders.
The findings suggest that excess weight can signal, or even trigger, less obvious conditions in autism, and that variations in weight may affect results about the prevalence of sleep, mood and anxiety problems in behavioral research studies.
In the new study, researchers calculated the body mass index (BMI), a measure of body fat based on weight and height, of 376 children with autism living in Oregon. (The healthy range for a BMI is between 18 and 25.) The participants, ranging in age from 2 to 18 years, are part of the Autism Treatment Network, a group of collaborating hospitals organized by the research and advocacy group Autism Speaks.
The researchers then analyzed the relationship between parent and clinician reports and the children’s BMI. The reports documented the children’s behavior and other conditions.
Roughly 18 percent of the children in the study were overweight — with a BMI between 25 and 30 — and 17 percent were obese, with a BMI above 30. For comparison, about 32 percent of typically developing children are overweight or obese.
Among teenagers with developmental disabilities, those with autism are the most likely to be obese, according to a study published 20 February in Maternal and Child Health Journal. The study found that 32 percent of adolescents with autism are obese, compared with 20 percent of those with developmental disabilities such as intellectual disability and attention deficit hyperactivity disorder. In contrast, 13 percent of typical teenagers are obese.
Studies have suggested that depressive symptoms may be both a cause and a consequence of childhood obesity. The Oregonstudy found that obese children younger than 6 years are more likely to suffer from anxiety and mood problems, such as depression, than are children who weigh less.
Obese children older than 6 years do not show this trend, but that may be because their version of the test poses different questions.
Roughly 85 percent of overweight and obese children with autism under 11 years also struggle with sleep. Children with the disorder tend not to sleep well in general.
The new study found that roughly 75 percent of the children with autism under 11 years of age with a healthy weight don’t sleep well.
Possibly as a consequence, one in three obese children with autism take the sleep-promoting hormone melatonin, compared with one in five children with autism who have a healthy BMI.
Interestingly, however, some symptoms of autism are less severe among children carrying extra weight. The study found that children with the disorder who are overweight, but not those who are obese, have lower levels of repetitive behaviors than their slender peers do.
This relationship is difficult to interpret, the researchers note. It’s possible that repetitive behaviors burn many calories, contributing a healthy BMI, but that does not explain the severity of the behavior among obese children with autism. The researchers also suggest that children with severe repetitive behaviors may take medications, such as risperidone, that cause them to gain weight.
Recommended reading

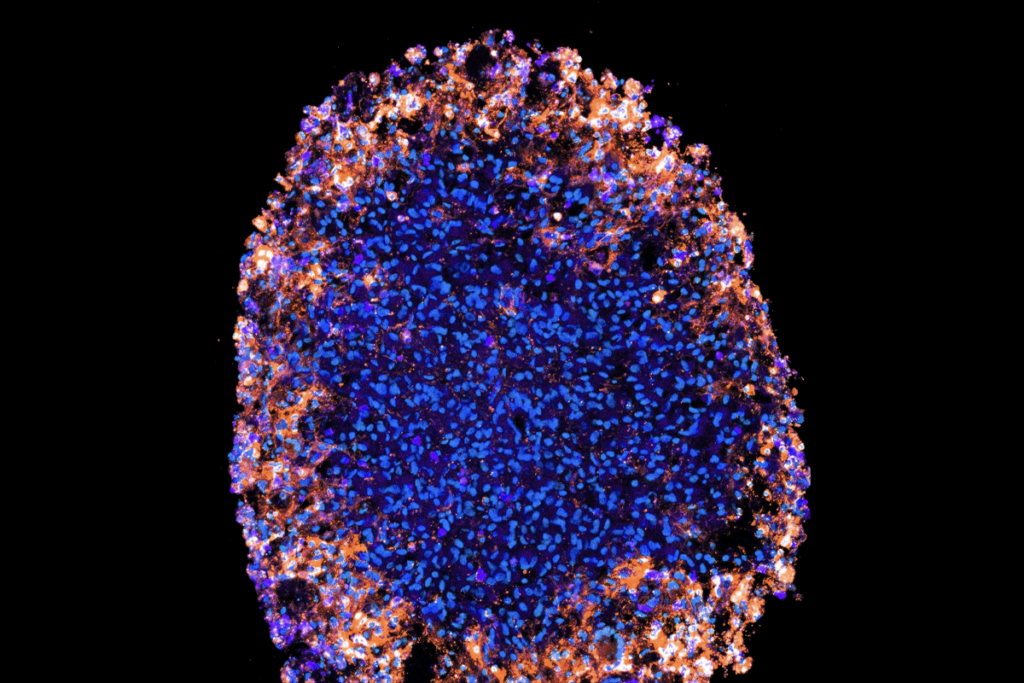
Among brain changes studied in autism, spotlight shifts to subcortex
Home makeover helps rats better express themselves: Q&A with Raven Hickson and Peter Kind
Explore more from The Transmitter
Dispute erupts over universal cortical brain-wave claim
Waves of calcium activity dictate eye structure in flies