‘Science junkie’ bets big on autism’s environmental origins
Jill Escher is on a mission to spur research into how chemicals in the environment may influence risk for autism.
Jill Escher can talk knowledgeably for hours, and hours, about autism — about its prevalence, which genes and environmental factors may be involved and how brain development may go awry in the brains of children with the condition. Escher, 50, has no formal training in science, but she reads scientific papers, gives lectures at universities and speaks at conferences.
This self-described “autism science junkie” taught herself the intricacies of research as she struggled to understand how her two children came to have autism. Along the way, she came up with a provocative idea to explain how chemical exposures might have led to their autism diagnoses.
Her theory goes something like this: In 1965, when she was in her mother’s womb, hormones her mother took during pregnancy damaged the DNA in Escher’s eggs. (Girls are born with all the eggs they will ever have.) The hormones left her seemingly unscathed but, decades later, caused her two children to have autism. In other cases, tobacco smoke or chemicals such as hormones or anesthesia drugs may alter eggs or sperm precursors.
Convinced of this hypothesis, in 2011 she established the Escher Fund for Autism Research, financed primarily by a stock portfolio her husband acquired while working at a Silicon Valley giant. Each year, the fund awards one team of scientists a grant of up to $100,000. The goal of each project is to determine whether and how exposures in the womb track with autism symptoms in grandchildren or in mouse pups.
“I feel like this is just the very beginning of what’s going to be a long scientific journey,” says Escher. “I’m just trying to accelerate the pace of research into these ideas.”
Few autism researchers dispute Escher’s idea, but most say they think it is unlikely to account for many cases of autism. “It’s not impossible that environmental variation is important,” says Bernie Devlin, professor of psychiatry at the University of Pittsburgh. “But the question I have is how important is [her hypothesis] to explaining risk for autism.”
Others are more sanguine, saying just because Escher’s hypothesis is esoteric doesn’t mean researchers should push it aside. “Her ideas should not be ignored,” says Peter Bearman, professor of social sciences at Columbia University. “People ought to have a chance to design studies to test what she thinks.”
Germ of an idea:
Escher didn’t give autism much thought until 2001 when her son Jonny, then 2, was diagnosed with the condition. She stopped working as a lawyer to care for him, and began to study autism’s causes. Her interest intensified when her daughter Sophie received the same diagnosis seven years later. Both children, now 17 and 10, speak no words and seem to have the intellectual abilities of toddlers.
For years, Escher wondered how she could possibly have had two children with autism. Both pregnancies were uneventful, with no sign of any complications, such as infections, that are linked to autism. Neither she nor her husband has a family history of autism or psychiatric conditions. And genetic tests revealed no glitches linked to autism in her children’s genomes.
“To have two kids whose neurodevelopment went so badly awry out of absolutely nowhere was, and continues to be, a deep mystery,” Escher says. “Why would this happen?”
In 2010, she stumbled across research that suggested a link between in vitro fertilization and autism risk in the resulting children1. Escher had never used fertility treatments, but the study prompted her to ask her mother if she had used any. To her surprise, her mother said she had taken synthetic hormones when pregnant.
Escher eventually managed to get a copy of her mother’s medical records and learned that her mother had taken six hormones — including synthetic estrogens, progestins and corticosteroids — to prevent miscarriage while pregnant with Escher.
Escher still could not explain how the drugs related to the children’s diagnoses. A year later, she heard a “nutrition guru” on a podcast claim that what a pregnant woman eats can affect her future grandchildren by altering her fetus’ ‘germ’ cells — cells that become eggs or sperm, and later may become part of a fetus. Escher recalled that her mother had taken hormones throughout the first seven months of her pregnancy, including the period during which eggs in a female fetus develop.
“It occurred to me that maybe those drugs had some impact on my eggs,” Escher says.
Hormone hypothesis:
Escher contacted reproductive and developmental biologists for their take on her idea. She says they told her they did not know of any studies investigating the effects of those hormones on developing eggs or sperm. But they pointed her to research in rodents hinting that other hormone-like chemicals, such as pesticides and plasticizers, affect germ cells.
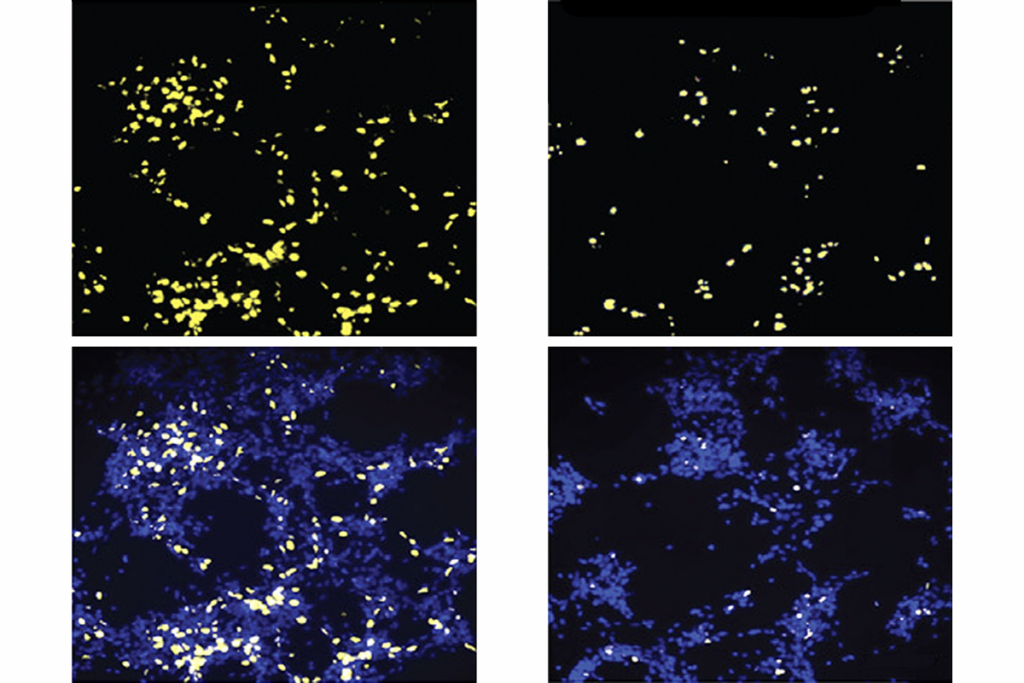
Emerging evidence hints that some synthetic chemicals may damage not just DNA, but also the ‘epigenome’ — the pattern of chemical tags that control how genes are turned on and off. Animal studies suggest that epigenetic patterns can be passed down through generations.
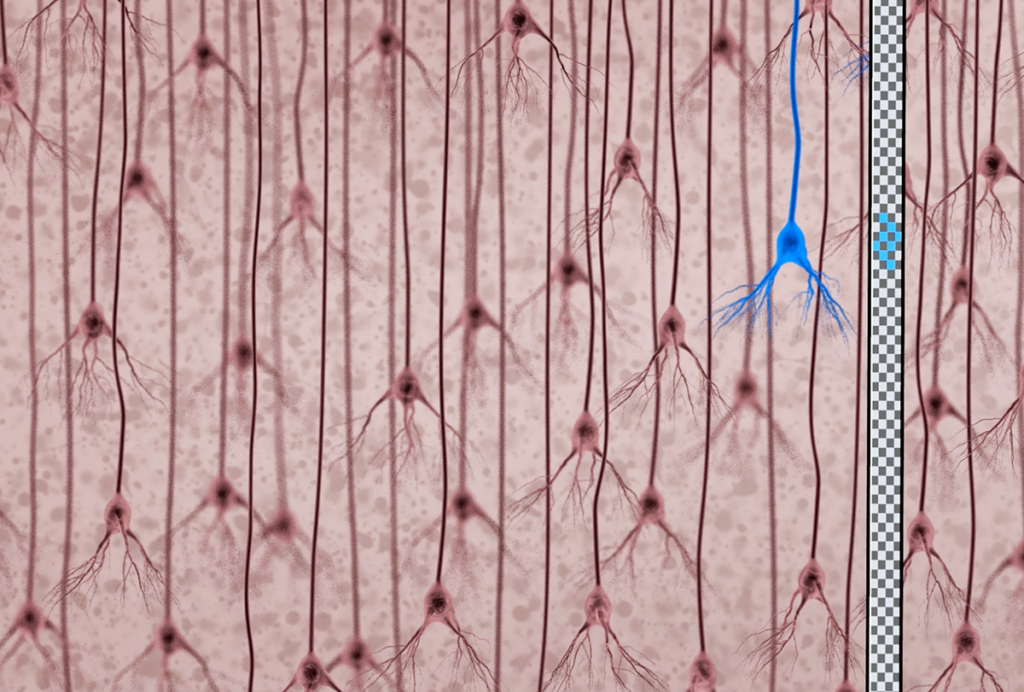
Aberrant epigenetic patterns in the brain could contribute to autism, but no one knows for sure whether an altered epigenome affects brain development in children or grandchildren.
Few studies have looked at how chemicals affect human germ cells. “We don’t traditionally think too much about how germ cells are affected by those exposures,” says Lisa Chadwick, health scientist administrator at the National Institute of Environmental Health Sciences in Research Triangle Park, North Carolina.
Even if chemicals affect the epigenome of germ cells in ways that are passed down, it’s unclear how this would lead to autism. “Just because there’s a change in the epigenome doesn’t necessarily mean that it’s going to cause a negative health effect,” says Dana Dolinoy, associate professor of environmental health sciences at the University of Michigan in Ann Arbor. “That is one of the critical barriers in this field.”
DNA damage:
Researchers now know that some people with autism carry rare mutations that are not inherited from their parents. “A big question in the field is, ‘Where are these mutations coming from?’” says Mark Zylka, associate professor of cell biology and physiology at the University of North Carolina at Chapel Hill. Geneticists typically assume these mistakes arise by chance as germ cells divide, but chemicals — such as those Escher wants to investigate — may cause the same sort of damage, he says.
Proving that the chemicals contribute to autism will be tricky, however, he says. “If you have some chemical that causes random mutations in the germ cells, the odds of it hitting an autism gene are low.”
Instead of trying to link a pregnant woman’s chemical exposure to autism in her grandchildren, it might be more fruitful to determine whether the exposure triggers spontaneous mutations in her child, Zylka says. “That’s an easier question to address,” he says.
Even if the answer to this question is yes, chemical exposures might account for only a small proportion of autism cases. Genetic factors confer a substantial portion of the risk for autism — at least 50 percent, according to the latest estimate. Rare, spontaneous mutations account for more than 3 percent of autism risk, and no one knows how much epigenome alterations might contribute.
Escher says her hypothesis evolves as she learns and communicates with scientists. “I welcome people asking uncomfortable questions and poking me; it only makes [the hypothesis] stronger,” she says. “If the day comes to pass that none of this proves to have any validity, then okay, another hypothesis bites the dust. But I have some ideas I think are important.”
References:
- Zachor D.A. and E. Ben Itzchak Res. Dev. Disabil. 32, 2950-2960 (2011) PubMed
Recommended reading
Documenting decades of autism prevalence; and more

Expediting clinical trials for profound autism: Q&A with Matthew State
Explore more from The Transmitter
‘Perturb and record’ optogenetics probe aims precision spotlight at brain structures