For more than a decade, Ruth Carper has noticed a troubling pattern in the neuroimaging literature on autism: Every review article seems to say that scientists don’t know much about older autistic adults. Some studies have identified differences between autistic and non-autistic adults, but typically at only a single time point, not over multiple years. Carper, research associate professor of psychology at San Diego State University in California, decided to address this gap.
Since 2015, she and her colleagues have been collecting MRI scans and other data from 40- to 70-year-old autistic and non-autistic adults to see whether the two groups age differently. The team’s first set of results shows various brain structure differences associated with motor skills, anxiety and repetitive behaviors. This year, Carper and her team have begun to collect a second set of data from the same participants, as well as a new cohort, which may begin to illuminate how these associations change over time.
Spectrum spoke with Carper about what she and her colleagues have found so far, the challenges of studying this population and what she hopes others will take away from her team’s efforts.
This interview has been edited for length and clarity.
Spectrum: Why did you embark on this longitudinal study?
Ruth Carper: I had been studying autism in children and adolescents, and I realized that nobody was looking at what happens in aging. So we wanted to know more. After all, everybody who has autism is getting older.
S: Your team has published several papers on the study’s first time point. What have you found?
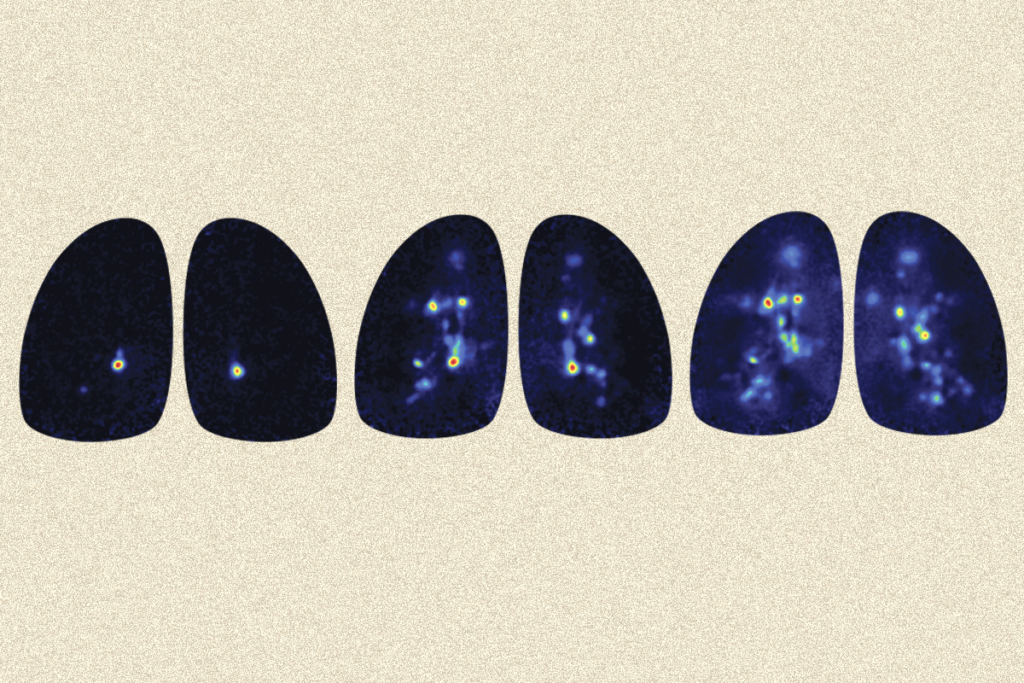
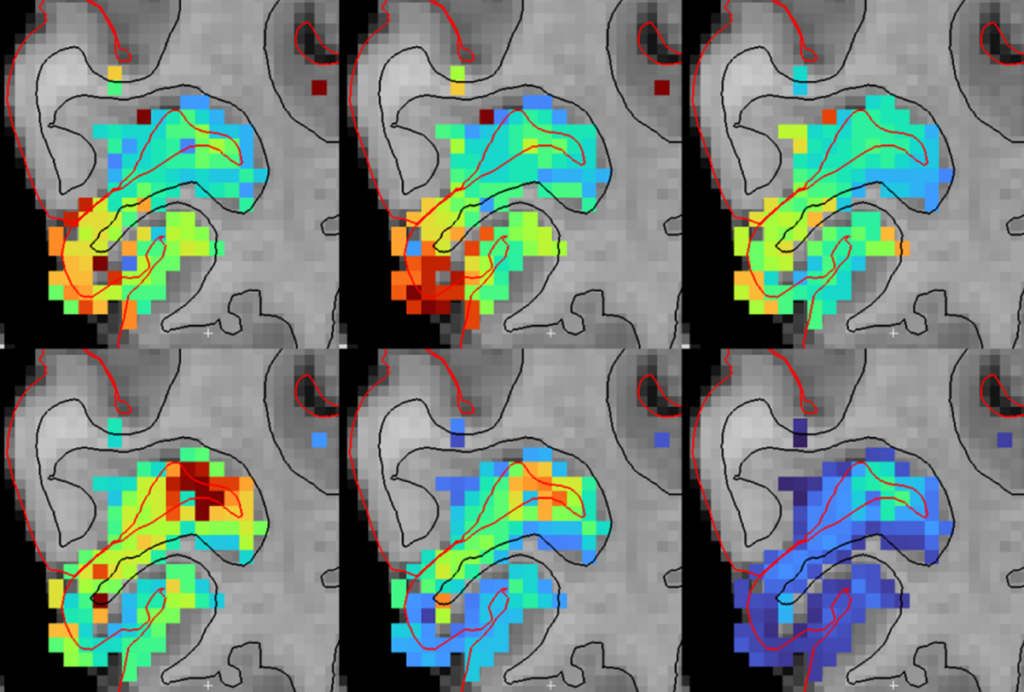
RC: One thing we found was that aging autistic adults score lower on assessments of motor function than non-autistic adults do, and this is associated with reduced functional connectivity and atypical network organization in the sensorimotor network. Executive function, to the degree that we’re able to measure it, also seemed important: Non-autistic adults show a clear relationship between their inhibition skills and the surface area of their anterior cingulate cortex, but autistic adults have no such relationship.
We’ve deliberately targeted those functions that are not only affected by aging in the general population, but that are also different in autism. With just one time point, we don’t yet know how much of that is just because this is an older population. It could be that these folks have always had these differences. It’s really the longitudinal data that’s going to show us.
We’ve seen reduced connectivity in autistic adults compared with non-autistic adults, but I don’t know that we have enough data to draw any conclusions about which networks are most affected. We also don’t know whether the rate of change in connectivity patterns differs between autistic and non-autistic adults as they age — because that reduced connectivity is also seen in younger people with autism — and that’s the biggest question.
S: What are some of the biggest challenges in studying this age group?
RC: The heterogeneity in autism — at any age, the traits we see and the affected brain areas and networks are heterogeneous. Then the older you get, more heterogeneity of experience accumulates: the interventions that people have gone through, the educational opportunities or lack of opportunities that they’ve had.
And then you’ve got cohort effects, which are going to be the most striking thing: We’ve got people who received a diagnosis under every version of the Diagnostic and Statistical Manual of Mental Disorders (DSM) that has ever existed. Someone with autism who is now about 50 might have been diagnosed under the DSM-III, the first edition to include “autistic disorder” as a diagnosis, or might have received another diagnosis under the DSM-II, such as “mental retardation” or “schizophrenia, childhood type.” Or they might not have been diagnosed with anything at all.
S: How do you recruit participants?
RC: We work with agencies that provide supportive living or supportive employment. We go to any event that’s vaguely related to autism, just to advertise our study as broadly as we can. Because we are a large group that studies kids with autism as well, we reach out to their families. It is not at all uncommon for a parent who has a child on the spectrum to say, “You know what, now that I’ve seen what my child is like, I’m realizing maybe I fit on that spectrum, or maybe my brother fits on that spectrum.” So we get referrals that way. The toughest group to find is those who never had a diagnosis in the first place.
Adults who need a diagnosis and struggle to find one, they wind up coming to us, to our research study, because that’s about the only way they can get an adult diagnosis. So, in our 40- to 70-year-old study, we don’t require an existing diagnosis.
If someone thinks they might have autism, they are welcome to volunteer for the study. We then have a multistage enrollment process that includes phone screenings and an in-person assessment. Sometimes people kind of meet the criteria, or they could probably use some support, but they don’t quite meet the criteria for our research study. In that case we usually write up a report that they can use for services.
To enroll 41 participants for our first time point, we had to screen 197 individuals. We’ve enrolled more since then, but it is a huge undertaking.
S: Now you’re collecting data for the second time point of the longitudinal study. What does that look like?
RC: We have this large cohort that we started with in 2015, for whom we have diagnostic information, neuropsychological cognitive information, IQ measures, and executive function and motor measures. We’ve got extensive MRI data on functional conductivity, neuroanatomical information and diffusion data. We’re collecting all these measures all over again, as well as doing a medical screening and collecting information on challenges related to the pandemic.
We originally planned to have about three years in between the two time points, but due in part to the pandemic, it’s going to be more like five to seven years. When you’re looking at aging, more time is beneficial from a research standpoint, though. If there are differences, they’re now going to be larger.
S: What do you hope that researchers who want to study autism in older adults might take away from your work?
RC: Regarding studying the population, it is not easy. There are big challenges. There are statistical challenges, cohort effects, many, many things you need to adjust for: differences in medical status, age at first diagnosis, socioeconomic status and cognitive impairment level, if any. Getting a broad representation of gender and ethnicity is a big one, too. But it’s something that really needs to be done, because it is a population where there just isn’t enough information. And autistic adults make up a population that is completely underserved.
It’s rewarding, because any time that I talk to adults with autism in this age range, they’re excited to know that anyone is looking, that this group has not been entirely forgotten. It’s not that the population itself is any more challenging than any other population. It’s just that finding the people in it is hard.