Rare form of autism linked to lack of key nutrient
A mutation that prevents some amino acids, the building blocks of proteins, from entering the brain may lead to autism.
A mutation that prevents some amino acids, the building blocks of proteins, from entering the brain may lead to autism1.
The number of people with the mutation is likely to be small. But for those individuals, injecting the amino acids into the brain might treat their autism. The results were published 1 December in Cell.
The findings add to a body of evidence suggesting that conditions that arise from the lack of a key nutrient can raise the risk of autism.
“The metabolic disorders are among the more treatable of human genetic conditions,” says Arthur Beaudet, professor of medical and human genetics at Baylor College of Medicine in Houston, Texas, who was not involved in the study. “If we have metabolic findings, it generally means that there is some potential for dietary manipulation or other intervention.”
The researchers first reported the link between a metabolic problem and autism in a 2012 study. They identified a mutation that inactivates both copies of a gene called BCKDK in individuals with autism in three families. Lack of BCKDK leads to rapid disassembly of three amino acids that the body cannot make and must get from food.
The team hypothesized that the mutation leads to a deficiency of these essential amino acids in the brain — which in turn leads to neurological problems. In support of this theory, they found that mice lacking BCKDK have a dearth of these amino acids in their brain.
“It is very fascinating to think that simple amino acids that we get through our diet continuously can regulate brain activity,” says lead researcher Gaia Novarino, assistant professor at the Institute of Science and Technology in Klosterneuburg, Austria.
Brain access:
If the amino acids’ presence in the brain is key, the researchers mused, similar problems should arise from mutations that prevent the amino acids from entering the brain.
Typically, the blood-brain barrier — a set of specialized cells on certain blood vessels — blocks toxins from seeping into the brain. Dedicated channels recognize permissible molecules and usher only those molecules into the brain.
Novarino and her team looked for mutations in these channels in more than 2,000 families in which intermarriage among related individuals is common. (Intermarriage increases the chances of inheriting double doses of harmful mutations.) In two of the families, the researchers found multiple children with autism who have mutations in a gene for a channel component.
Five children with double hits to this gene, called SLC7A5, have autism, motor problems, unusually small heads and are either nonverbal or have delayed language. (One other child with the mutation shares many of these features but was not tested for autism. Another died of unrelated causes prior to publication.)
“This study exemplifies how new hypotheses about autism etiology can be obtained from genetic data by clever detectives,” says Aravinda Chakravarti, professor of medicine at Johns Hopkins University in Baltimore, who was not involved in the study.
Better balance:
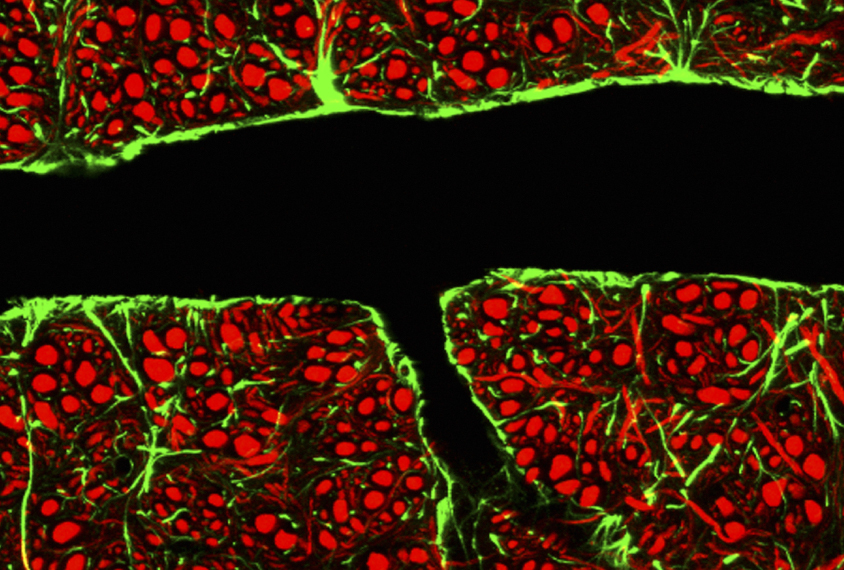
The researchers made mice that lack SLC7A5 in cells of the blood-brain barrier. They found that fetal mice show typical brain levels of dietary amino acids, suggesting the amino acids either leak into the brain or are brought in by another transporter.
After birth, however, brain levels of the essential amino acids plummet. As adults, these mice have motor tics, repeatedly clasping their hind paws together, and struggle to balance while walking on a beam. They also show social deficits.
The motor skills of the mice improved significantly after the researchers injected two of the missing amino acids into their brains using a pump. The treated mice also stopped clasping their paws. (The treatment involved cumbersome headgear, so the researchers could not test the mice’s social skills.)
Amino acid injections might also help people with autism who have SLC7A5 mutations, Novarino says, but the procedure carries risks, so it would require rigorous testing first.
Why low levels of amino acids in the brain might lead to autism specifically is an open question. As a step toward an answer, the researchers found that mice with SLC7A5 mutations have defects in neurons called interneurons, which dampen brain activity. Studies have tied problems with signaling among interneurons to autism. The next step is to understand why this family of neurons is especially sensitive to a lack of these amino acids, Novarino says.
Meanwhile, the findings hint that mutations in other genes that regulate amino acid levels in the brain might contribute to autism, Chakravarti says. It is also possible that mutations with mild effects on amino acid levels could be a factor in a larger group of people with autism.
References:
- Tarlungeanu D.C. et al. Cell 167, 1481-1494 (2016) PubMed
Recommended reading

Among brain changes studied in autism, spotlight shifts to subcortex
Home makeover helps rats better express themselves: Q&A with Raven Hickson and Peter Kind
Explore more from The Transmitter

Frameshift: Shari Wiseman reflects on her pivot from science to publishing

How basic neuroscience has paved the path to new drugs