In race to crack autism’s code, two contenders shoot ahead
Two candidate genes have risen to the top, and may help scientists understand what autism really is.
Readers, meet CHD8: In the lineup of genes for autism risk, it has emerged as a leader. CHD8 controls thousands of other genes via chromatin — a complex of DNA and protein. And nearly everyone with a faulty copy of CHD8 seems to have autism.
Now meet SCN2A: This is the other leading candidate, and it couldn’t be more different. SCN2A codes for a sodium channel. Some mutations in this gene are known to cause severe seizures early in life. Others, apparently, cause autism.
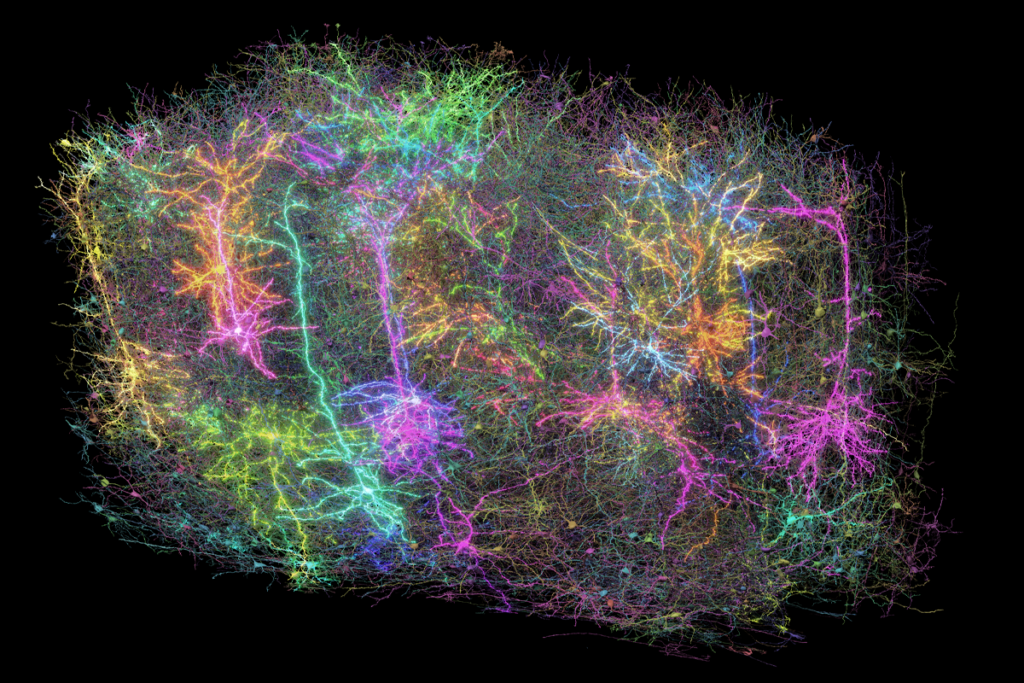
Neither gene is one anyone would have predicted as being important in autism a decade ago. Scientists then had their sights mostly set on genes at neuronal connections.
“If someone came to me back in 2010 and said, ‘The answer is going to be a sodium channel and a chromatin gene,’ I would have thought that’s insane, that’s madness,” says Stephan Sanders, assistant professor of psychiatry at the University of California, San Francisco.
Both emerged as autism candidates in separate 2012 studies that sequenced the genes of hundreds of children with autism and their unaffected parents and siblings. And they quickly found their champions.
CHD8’s advocates say it tops their list because its mutations seem to be highly ‘penetrant’ — meaning they nearly always cause autism, sometimes without other conditions such as intellectual disability. SCN2A’s supporters, including Sanders, call it the ‘Rosetta Stone’ for autism because it has a well-understood function that is relatively easy to study. Most candidates for autism risk are more likely to be similar to SCN2A than to CHD8, in that they may have links to multiple conditions.
Mutations in either gene are rare, accounting for less than 0.5 percent of people with autism. But their strong ties to autism — and their differences — may reveal the various paths that lead to autism.
“The fact that you have these two genes that at face value have nothing in common — there’s no obvious reason why these should lead to the same common phenotype — that is at once very puzzling, but also the greatest strength here,” says Sanders. “I have a sneaking suspicion if we could understand why SCN2A and CHD8 are in this special top-tier category, we probably would understand sort of the core of what autism is.”
Leader of the pack:
CHD8 had made its way to the front of the pack by 2014, when researchers published a high-profile study characterizing the features of children with mutations in the gene. It continued to top the list in several studies that followed. In a study published earlier this year, for example, CHD8 emerged as one of eight genes that crop up more often in people diagnosed with autism than in those with intellectual disability.
People with a mutation in CHD8 have distinct features, such as gut problems and large heads. They also have “waiting-room autism,” meaning their condition is instantly recognizable, says Raphael Bernier, who has described many of these individuals. So far, Bernier and his colleagues have characterized 26 such people; 24 of them have autism.
Their condition resembles “core autism” more than the effects of the other top candidates, says Bernier, associate professor of psychiatry and behavioral sciences at the University of Washington in Seattle.
Among the many genes CHD8 controls are many other autism candidates — including SCN2A. That suggests that the two genes converge on a similar process in the brain. “There has got to be some cross talk between them,” says James Noonan, associate professor of genetics at Yale University.
Catching up:
When it comes to understanding mechanism, SCN2A may cross the finish line first. Whereas CHD8 alters hundreds of pathways, SCN2A has a single, well-understood function: It propagates the electrical signals neurons use to communicate. Unlike CHD8, it is expressed only in the brain.
Still, SCN2A’s contribution to autism is not straightforward. Mutations in the gene could have widespread effects on brain circuits, says Kevin Bender, assistant professor of neurology at the University of California, San Francisco, who collaborates with Sanders. “We have a handle on very fundamental neuronal activity changes,” he says. “But that might just be the tip of the iceberg.”
Not all mutations in SCN2A cause autism. So far, scientists have found mutations in SCN2A in 55 people with autism and another 13 with developmental disability. Mutations that enhance the sodium channel’s activity appear to lead to infantile seizures, whereas those that disrupt the channel’s activity reliably lead to autism.
Even in cases where the mutation leads to autism, the picture is murkier than with CHD8. Bernier and his team have assessed 10 children who have mutations in SCN2A.
“When we’ve been seeing our SCN2A kids, it didn’t strike me in the same way [as with CHD8] because these kids have other profound challenges,” says Bernier. Most of the children also have severe intellectual disability or seizures.
Holding hands:
These observations suggest that CHD8 may hold an edge over SCN2A in terms of autism candidacy.
Still, studies cataloging the effects of mutations in SCN2A may shore up its association with autism, says Holly Stessman, assistant professor of pharmacology at Creighton University in Omaha, Nebraska. “I think the current work in SCN2A really highlights a need to understand the function of a mutation,” she says.
Sanders and Bender are characterizing how SCN2A mutations change electrical currents in cell culture and in mice. Meanwhile, Noonan and his colleagues are mapping the effects of CHD8 mutations on gene expression in the brain.
“A detailed analysis of all the mutations and their functions and how they affect development is going to be critical before we can really make a comparison or conclusion,” on the relative importance of the two genes in autism, says Guoping Feng, professor of brain and cognitive sciences at the Massachusetts Institute of Technology. Feng’s team is introducing CHD8 mutations into mice.
Ultimately, the answers to autism may lie in how these two genes chart two different paths to the same result, says Sanders. “In a race, there is a winner and a loser, and this is actually a situation where the real winning is when both those genes cross the line and shake hands.”
Corrections
A previous version of this story stated that CHD8 is not usually associated with intellectual disability. In fact, it is associated with intellectual disability slightly more than half the time.
Recommended reading

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys

PTEN problems underscore autism connection to excess brain fluid
Explore more from The Transmitter
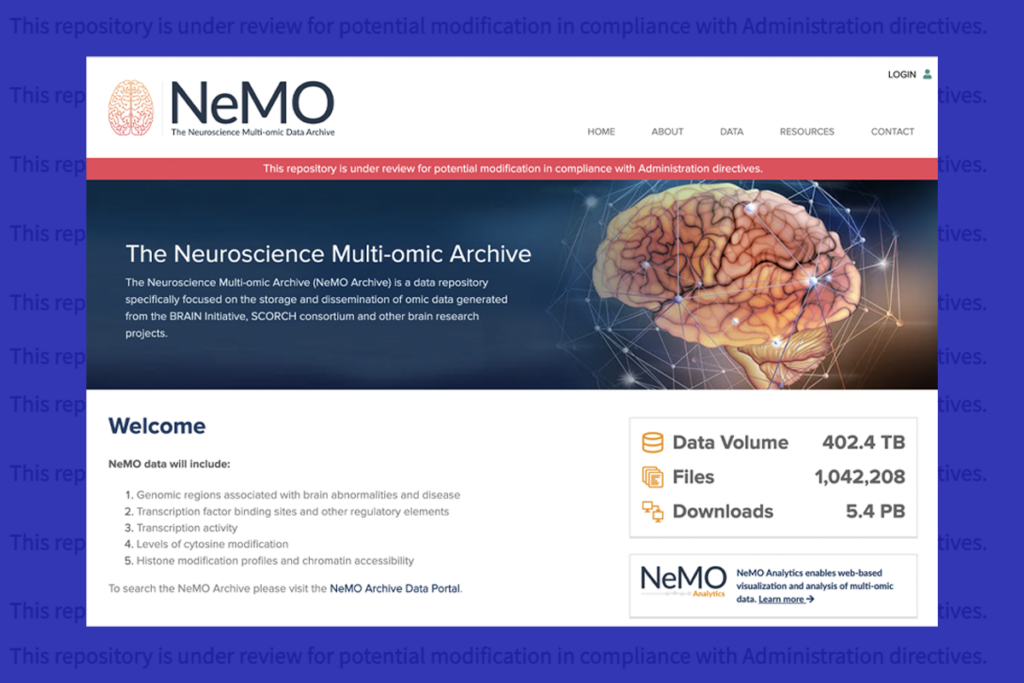
U.S. human data repositories ‘under review’ for gender identity descriptors