Questions for Joshua Gordon: Circuit solutions for autism
The new director of the National Institute of Mental Health says work on brain circuits may yield treatments for autism.

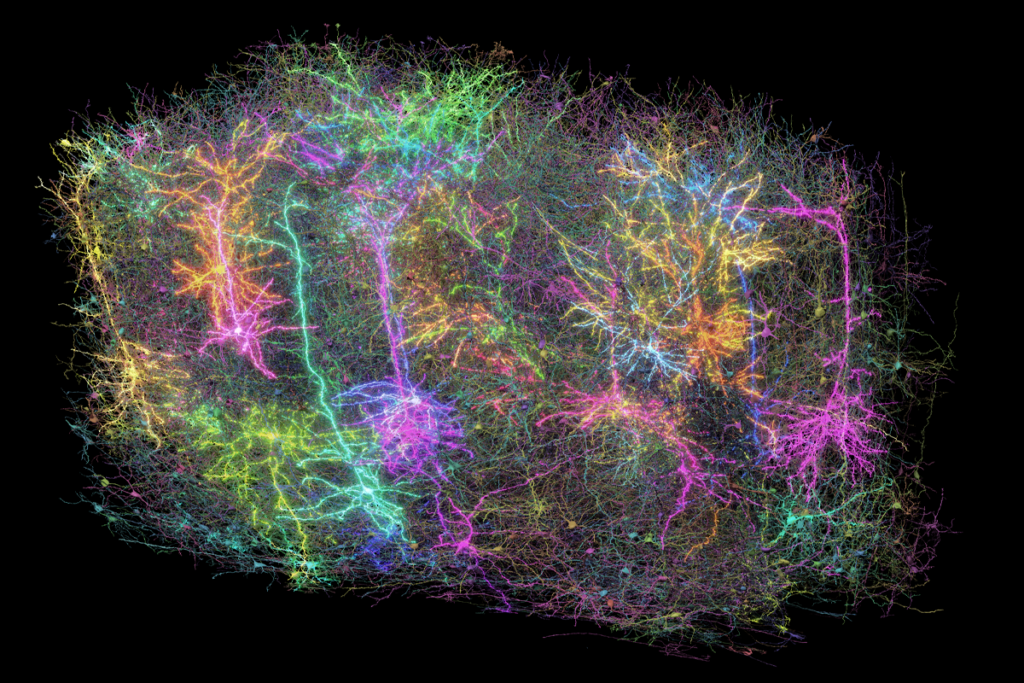
It’s been nearly three months since Joshua Gordon took the reins as director of the U.S. National Institute of Mental Health (NIMH). In that time, Gordon has made it clear that one of his top priorities will be ‘circuit science’ — investigations into the clusters of neurons that underlie certain behaviors.
Gordon studied neural circuits implicated in schizophrenia, anxiety and depression for more than a decade as a research psychiatrist at the New York State Psychiatric Institute in New York City. These conditions share features and risk factors with autism, suggesting the same brain circuits are involved.
Identifying which neural circuits are altered in the brains of people with autism may help scientists develop treatments that can fine-tune the wiring, Gordon says. But this approach could take decades, so Gordon also plans to invest in research on adults with autism. We asked him to elaborate on his plans to back science that is likely to have a direct impact on the lives of people with autism.
Spectrum: How can ‘circuit science’ help people with autism?
Joshua Gordon: Right now, our understanding of which circuits underlie certain features of autism is rudimentary at best. Our goal is to identify behaviors that are disruptive for people with autism, and then manipulate the underlying circuits to reduce a person’s disability without altering his or her abilities.
For instance, we need to know more about the circuits that underlie sensory hypersensitivity — the sensitivity to sight and sound experienced by some individuals with autism. Are they the same or different than those involved in sensation? For auditory hypersensitivity, for example, wouldn’t it be great to tune down the system so that it is not quite as sensitive to loud music, but still sensitive enough to hear the music?
We can tune circuits with exquisite precision in mice. We can boost the activity; we can turn down the activity. More and more, we’re learning how to do that in specific circuits related to things such as fear and anxiety, which plague many people with autism. The more we learn about a given circuit, the more we can control activity within that circuit. And that’s very exciting.
S: What’s the ultimate aim of this work?
JG: It’s important to use the knowledge we learn from neural circuits to design therapies that modify those circuits. Those may be medications, psychotherapy or even behavioral therapy. Theoretically, one could use techniques such as transcranial magnetic stimulation to directly alter a circuit’s activity. But we’re not there yet.
S: How has your previous work influenced your goals for autism research?
JG: From a genetics standpoint, schizophrenia, autism and bipolar disorder have a lot of overlapping genes. Imaging data also reveals similarities between these conditions. An imbalance between excitatory and inhibitory brain signals seems to be present in both autism and schizophrenia.
It could be that these separate conditions are tightly related generally, or perhaps we see these commonalities because certain people labeled as having ‘schizophrenia’ are neurobiologically akin to some people labeled as having ‘autism.’
In a cross-diagnostic approach, the idea is to study specific features — such as behaviors, genes, brain activity — that are commonly disrupted across different conditions, and ask whether these features are seen in certain subgroups of people regardless of which condition they have.
The hope is that we’ll be able to identify an individual’s particular genetic risk, their particular behavioral disturbances and their particular brain signatures. Altogether, these might indicate a diagnosis that is more reliable than ‘schizophrenia’ or ‘autism,’ and more predictive in terms of what treatments would help that individual. That’s really what precision medicine is all about.
S: What are your plans for helping people with autism in the short term?
JG: I chair the Interagency Autism Coordinating Committee, which manages autism initiatives across funding agencies. The committee’s priority is to make sure the federal effort on autism accounts for the needs of individuals with autism and their families.
One focal point is research into treatment for adults with autism. This is an unmet need in the community. So we’ve started giving out grants for studies into what interventions are efficacious for these adults.
We also need to pay attention to the issue of premature death in adults with autism. Individuals with autism have a lower life expectancy than their typical peers. That’s pretty tragic. We need to find out what’s causing this phenomenon.
For instance, do individuals with autism have the same access to medical care as people without autism? Are they given the same priority by their primary care doctor? Can they recognize that something feels wrong and communicate that concern to a physician? Is there a biological factor in individuals with autism that not only affects their brain but also, say, their heart or other organs?
We’d love to know the answers to these questions, but getting them requires research.
S: What’s the most important insight you’ve gleaned over your career?
JG: The most profound thing I’ve learned is that a person’s identity can be wrapped up in their psychiatric diagnosis. As researchers and physicians, we must remember that this can work both ways.
For instance, a person’s identity might be so wrapped up in their experience of a psychiatric condition that it might be very difficult for them to muster the hope to continue living. But another person might see the condition as something that makes them special. Even though it causes disability, it also creates uniqueness.
Many of the people with autism with whom I’ve worked side-by-side in a professional capacity say that autism is disabling in many ways, but it also gives them a powerful perspective on life.
Recommended reading

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys

PTEN problems underscore autism connection to excess brain fluid
Explore more from The Transmitter
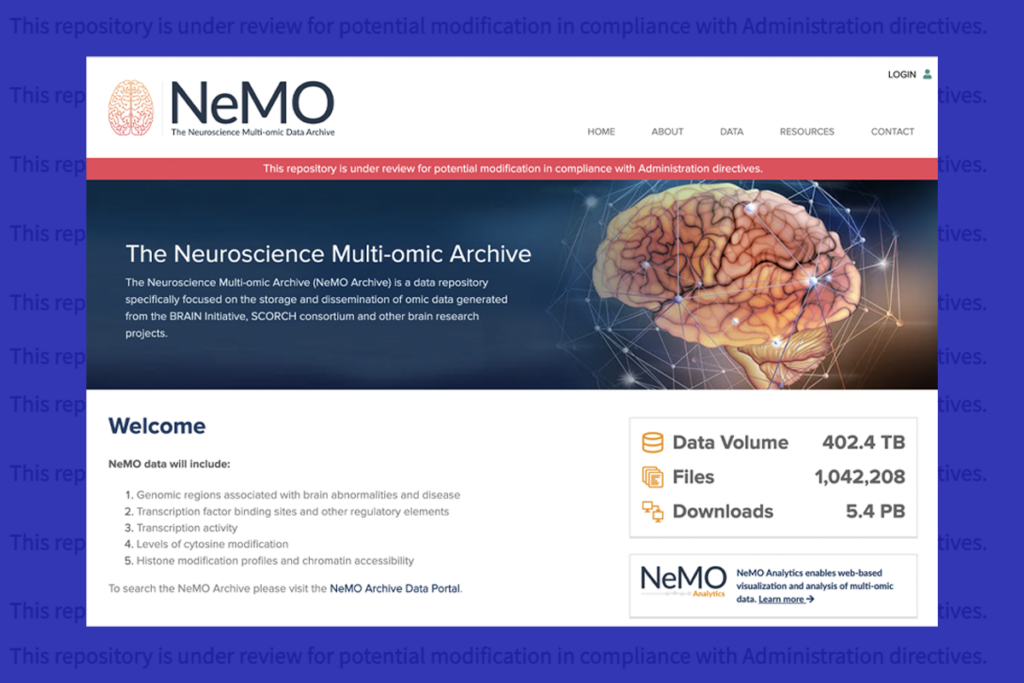
U.S. human data repositories ‘under review’ for gender identity descriptors