Questions for Nordahl, Mello: Scans for children with autism
Techniques used in behavioral interventions could help scientists scan the brains of children who have both autism and intellectual disability.

The cacophonous, confined space of a magnetic resonance imaging (MRI) scanner can provoke panic in anyone. But for some children with autism who are extremely sensitive to noise, lying in a scanner can be terrifying.
Some scientists try to ease the children’s anxiety by drawing storyboards that explain exactly what will happen the day of the scan. To make the process fun, they decorate the scanners to look like a train or spaceship. And they introduce the children to these spaceships with a ‘mock’ scan before attempting the actual test.
But these tactics don’t work for roughly one-third of children with autism who have intellectual disability. These children may not be able to follow the storyboards, says neurobiologist Christine Wu Nordahl, and so studies often rely on scans from children with at least average intelligence quotients (IQs).
To help coax children with IQs below average into a scanner, Nordahl recruited a behavioral analyst, Melissa Mello. Using a variation of applied behavioral analysis (ABA), a widely used autism therapy, the team succeeded in scanning the brains of 13 children, ages 9 to 13, who have both autism and intellectual disability1.
Other teams may be able to use the same approach and include children with intellectual disability in their studies, the researchers say. We spoke with Nordahl and Mello about what they hope to learn from the scans.
Spectrum: Why do imaging studies exclude children with low IQs?
Christine Nordahl: There really is the impression in the field that children with low IQs are unable to submit to any sort of scanning without general anesthesia or sedation. Anesthesia is often not an option. In the case of functional imaging, a person has to actively respond to certain stimuli, so they need to be alert. Also, anesthesia carries some risk, and I think some parents are reluctant to sign up for imaging studies when anesthesia is involved.
In our case, we want to scan these children multiple times as they grow up, and the risk of general anesthesia magnifies each time.
S: What was your strategy for scanning these children?
CN: Early on, we recognized that mock MRI scans alone would not work. With a mock scan, you can train children to lie down and remain still. But children with intellectual disability, who are sometimes minimally verbal, don’t respond as well to the typical mock scan procedures. This is probably because MRI researchers aren’t clinically trained to work with more severely affected children.
Building off the idea that clinicians have used ABA strategies to help these children sit in a dental chair or prepare for a flu shot, we enlisted the help of colleagues with expertise in behavioral analysis. Behavioral analysts Melissa Mello and Audrey Shen gradually familiarized children with the scanning environment by breaking down the typical mock scanning process into incremental steps.
S: How does the method work?
Melissa Mello: Our approach involved learning each child’s needs and taking each step at his or her pace. We also asked about each child’s favorite foods or toys, and we made those items — goldfish crackers, cookies, fruit snacks, toy helicopters or plastic alligators — available as rewards.
We took each child on as many visits to a scanner as needed. Some children were able to enter the scanner on the first day, whereas others initially just sat near it and received their reward. For all of the children, we used a process called ‘shaping,’ which involves slowly increasing the expectations for them.
One of the most successful approaches was to play a child’s favorite video in the scanner. Once a child realized that he or she could just hang out and watch a video, the child usually decided that being in the scanner wasn’t so bad.
We also used both visual and verbal countdown timers to let the children know how long we wanted them to remain still for each scan. And for some children, we stopped the video if they moved, reinforcing the need to stay still.
S: Were there any children who found this challenging?
MM: One girl wouldn’t even go near the scanner on the first day. All she was willing to do was enter the room and sit down in a chair. We gave her a favorite treat, fruit snacks, just for doing that, because it was so stressful to her.
During the next visit, we escalated her challenge: She had to come into the room, sit in the same chair and get a little bit closer to the scanner. Then we asked her to sit on the table. We turned each step into a positive experience that yielded a treat.
For another child in the study, we learned during a scanner visit that videos were distracting, but that she was soothed by a certain musical artist. So we played music for her rather than a video. It’s about individualizing the process.
S: Did these methods come up short for any of the children?
CN: Not yet. Although some children needed up to three visits to the mock scanner, once these children were prepared, the actual imaging session was successful on the first try.
The psychologists who work with these children were surprised we were able to obtain these scans. Many of the parents were also skeptical when we first approached them about having their child do the MRI scan while awake. We’ve all learned that these kids can do a lot more than anyone thought they could. This outcome is validating for the child and for the parent. That was an emotional part of the study we didn’t anticipate.
S: What do you hope to learn from scans of this group of children?
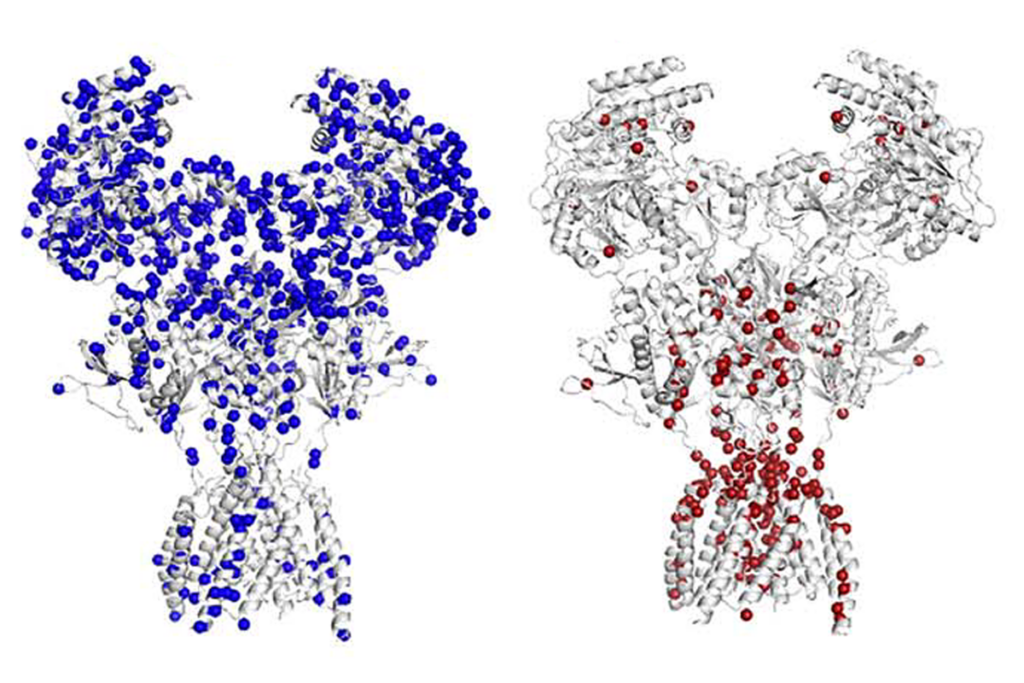
CN: Some children with autism have abnormally enlarged brains around age 3. And current theory states that the enlargement goes away between adolescence and adulthood. Brain imaging in 3-year-olds is typically carried out during natural sleep or using sedation, so data at that age includes children with low IQs. But studies of older individuals only include children who have relatively typical IQs.
We really need longitudinal studies that extend from early childhood through adolescence to determine whether this altered trajectory of brain growth happens in everyone.
We’re now looking at kids who had large brains relative to their bodies at age 3 and who have intellectual disability. So far, at age 6, their brains show no signs of normalizing in volume2. The children are now between the ages of 9 and 13, and we are scanning them again to see if their brains remain enlarged.
S: How can other teams adopt this method?
CN: To do it right, I think you need a trained behavioral analyst. It costs more, but we’ve proven that it’s effective and would be money well spent.
References:
Recommended reading

New organoid atlas unveils four neurodevelopmental signatures
Explore more from The Transmitter

Anti-seizure medications in pregnancy; TBR1 gene; microglia

Vasopressin boosts sociability in solitary monkeys