Questions for Elizabeth Berry-Kravis: Measuring drug effects
Drugs designed to treat fragile X syndrome have yet to show substantial benefits in people. But rather than abandon them, child neurologist Elizabeth Berry-Kravis suggests a new way to measure their effectiveness.
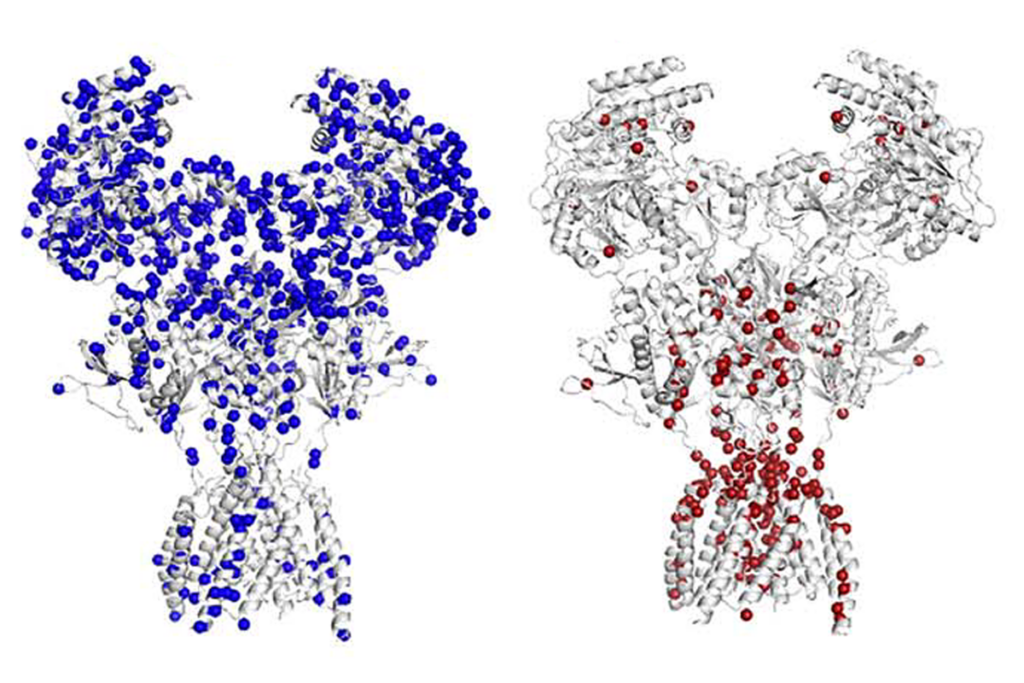
A number of drugs for fragile X syndrome, a leading cause of autism, have shown promise in animal models. For instance, drugs that inhibit a protein called mGluR5, which is overactive in people with fragile X syndrome, resolve symptoms of the disorder, such as social inhibition and repetitive behaviors, in mice.
Earlier this year, researchers reported that one class of drugs developed to treat fragile X syndrome may also work for some other forms of autism, bolstering interest in the therapies.
But so far, none of the treatments for fragile X syndrome have substantially improved behavior in people. Those negative results do not necessarily mean that the treatments are not effective, says Elizabeth Berry-Kravis, professor of child neurology at Rush University Medical Center in Chicago, who has led clinical trials of drugs for the disorder. Rather, she says researchers need to rethink how they measure the drugs’ effectiveness.
Here, Berry-Kravis advocates a more targeted behavioral measure, one that is less subject to bias and that relies on trial participants learning a specific skill.
SFARI.org: What measures have researchers traditionally used to evaluate drugs in people with fragile X syndrome?
Elizabeth Berry-Kravis: The primary outcome measure has always been behavioral reports. In other words, how has the participant’s behavior changed across the treatment period as defined by a parent-reported form, most commonly the Aberrant Behavior Checklist (ABC).
S: What are the main limitations to using parent-reported behavior as an outcome measure?
EB-K: Well, I think one issue is that a general behavioral measure such as the ABC may not be well matched to what the drug does at a neural and cellular level. Much of the data about a drug comes from basic science models such as cellular or animal models, and it’s hard to predict what the drug will do behaviorally in people based on basic science research.
For instance, drugs that block the mGluR5 receptor in the mouse improve plasticity, which means the neurons make more effective connections. Do we think that behavior in people is a good surrogate for improved neural plasticity? Well, it’s hard to know. Behavior in adults is the result of so many things that have built up all through their life that it’s really difficult to know whether a drug directed at a molecular cause of a disorder would necessarily make a specific behavior, or even general behavior, better.
S: How would you suggest measuring changes in plasticity in response to a drug treatment?
EB-K: We have to be able to measure learning. To really measure plasticity and learning, we’re going to have to do trials where we administer some kind of intensive training and then measure an outcome that would get better if that training was helpful. The measure would match what our program was designed to teach.
S: Can you give an example of a learning task?
EB-K: Leonard Abbeduto, director of the University of California, Davis MIND Institute in Sacramento, has a language-learning program that’s delivered by the parent. He has data suggesting that the training itself can accelerate language progress a little bit, so if you use the language-learning intervention in a young child along with a drug targeted to the disease process, you might see a difference in the ability of the child to learn language. You might predict that a child on the medication would have more words, or be able to express himself better than one who did not get the drug.
There’s some precedent for using language, reading, behavioral, math, social and executive training programs with people who have fragile X syndrome and showing that they seem to learn faster with the training — at least while they are doing the training. But these are small studies. I don’t know of any large, multicenter clinical trials that have employed a training method to assess drug efficacy and whether the drug can make a person learn faster.
S: What are some potential advantages to learning-based outcome measures?
EB-K: Many of these things would be direct assessments. I think one of the key things we need to get away from is having only parent-rated assessments in our trials, because parents experience a placebo effect. They really want things to work — and so things do tend to work. But I don’t think we want to stop using all those measures. We do want to know how the parent is viewing how their child is doing. We just don’t want to rely entirely on that when a more objective measure, where we’re directly observing what the child is doing, will give us more objective and more quantifiable data.
S: Do you think that’s something the U.S. Food and Drug Administration (FDA) would approve?
EB-K: I think the FDA could potentially be open to looking at this model, given the right presentation of what exactly one is trying to do, because these treatments in fragile X syndrome are a new kind of model. You can’t really apply the principles of trials for depression or maybe even attention deficit hyperactivity disorder to people with fragile X or other developmental disabilities, because these are developmental disorders that evolve over a long time. The primary problem in fragile X is not one symptom; it’s that there’s an abnormality of synaptic plasticity. In order to see if a drug is directly targeting the disorder, we have to be able to measure learning and thinking.
Recommended reading

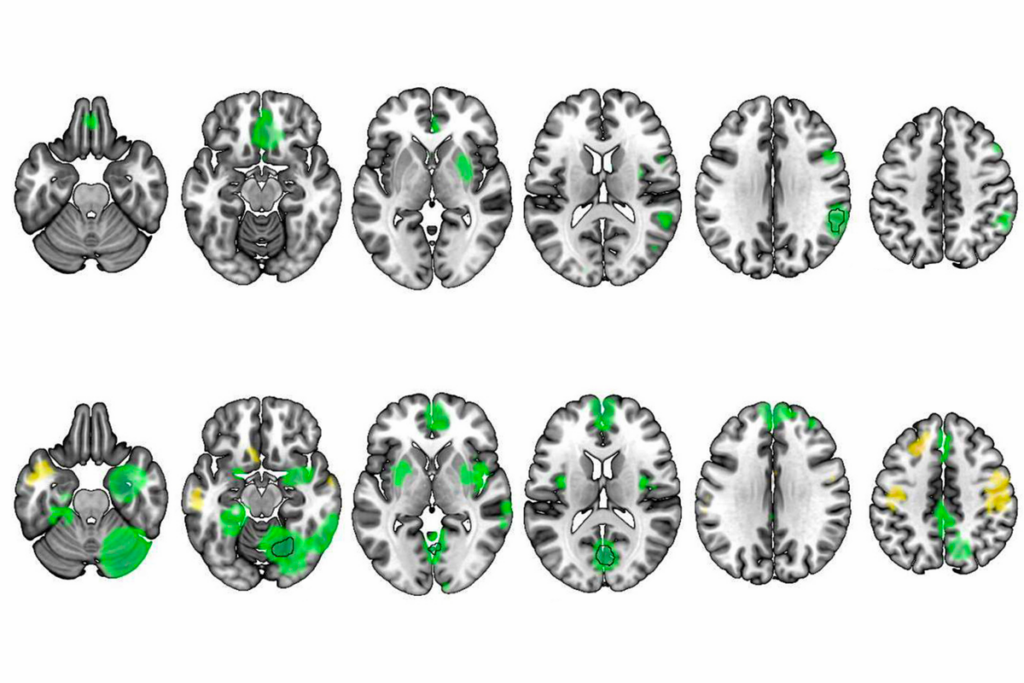
Too much or too little brain synchrony may underlie autism subtypes

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome
Explore more from The Transmitter
BCL11A-related intellectual developmental disorder; intervention dosage; gray-matter volume
Emotional dysregulation; NMDA receptor variation; frank autism
