Protein marker ties maternal inflammation to autism risk
Women who have high levels of C-reactive protein, a marker of inflammation, early in their pregnancies are at increased risk of having children with autism, reports a study published 22 January in Molecular Psychiatry.
-
Risk management: Preventing inflammation during the first and second trimester of a woman’s pregnancy may reduce the risk of autism in her child.
Women who have high levels of C-reactive protein (CRP), a marker of inflammation, early in their pregnancies are at increased risk of having children with autism, reports a study published 22 January in Molecular Psychiatry1.
Of 677 women in the study, those whose CRP levels are in the top ten percent of the group are 80 percent more likely to have children with autism compared with those in the bottom ten percent.
The study suggests that preventing certain causes of inflammation may help decrease autism risk, says lead investigator Alan Brown, professor of clinical psychiatry and clinical epidemiology at Columbia University in New York.
It also adds to growing evidence that the immune system plays a role in autism risk. Previous studies have shown that infections such as rubella or the flu during pregnancy increase the risk of having a child with autism.
“It’s not a huge effect, but it’s very significant,” says Paul Patterson, professor of biology at the California Institute of Technology, who was not involved with the study. “It’s another nail in the coffin on the case that inflammation — probably infection — during pregnancy is a risk factor for the offspring.”
CRP is produced in the liver in response to anti-inflammatory messengers called cytokines. The protein level rises in response to all types of inflammation, including infections, chronic inflammatory disorders such as arthritis, and injuries to anytissue in the body.
“The point of CRP is that it’s nonspecific, but it is sensitive,” says Thomas Insel, director of the National Institute of Mental Health, who was not involved in the study. “The fact that [risk of autism] has gone up tells you that you’ve got to do some digging to see what may be driving it, because there are lots of ways to get elevated CRP.” (The institute funded part of the study.)
Marking inflammation:
For the study, Brown’s team tapped the Finnish Maternity Cohort, a repository of 1.6 million blood samples collected from more than 810,000 pregnant women during the first to early-second trimester. These account for 98 percent of Finland’s pregnancies since 19832.
Since 1987, Finland has recorded childhood psychiatric diagnoses, allowing researchers to learn which women have children with autism. Of the 1.2 million births since 1987, researchers identified 1,132 children diagnosed with autism.
To confirm the accuracy of the diagnoses, Brown’s group randomly chose 80 children, evaluated them using the Autism Diagnostic Interview-Revised and found that 77 of them meet the criteria for autism.
“They actually did validate the diagnosis, which is usually not done,” Insel says. “They deserve a lot of credit for having done that very heavy-lifting kind of work.”
Brown’s team looked at 677 of the women whose children have autism, and compared them with 677 women whose children do not. They then examined a number of possible factors associated with autism, including maternal and paternal age and mental illness in either parent. None explain the relationship between CRP levels and autism risk.
When the researchers analyzed the autism group’s blood samples based on levels of CRP, they found the top 20 percent of women are 43 percent more likely to have children with autism compared with the lowest 20 percent.
“We’re getting now an emerging story about the possibility that inflammation is at least a fellow traveler with autism and may be involved even more directly in some causal mechanism,” Insel says.
Brown plans to explore the interplay between CRP and other maternal factors, including environmental influences such as an illness and genetic risk factors.
It’s not yet clear whether elevated CRP raises autism risk specifically or developmental disorders generally. Brown says he hopes to investigate other disorders for a link with the protein.
References:
1: Brown A.S. et al. Mol. Psychiatry Epub ahead of print (2013) PubMed
2: Lampi K.M. et al. J. Autism Dev. Disord. 41, 1090-1096 (2011) PubMed
Recommended reading

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys

PTEN problems underscore autism connection to excess brain fluid
Explore more from The Transmitter
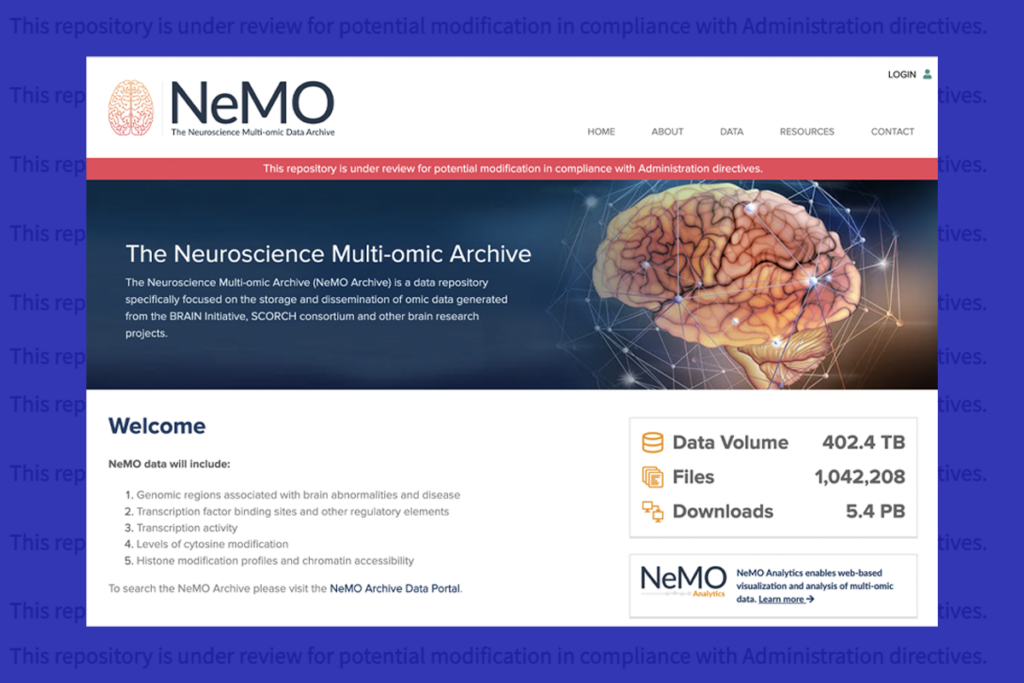
U.S. human data repositories ‘under review’ for gender identity descriptors