Powerful memory system may compensate for autism’s deficits
A brain system called declarative memory may help people learn scripts and strategies that alleviate autism symptoms, say Michael Ullman and Mariel Pullman.
Autism has been the focus of intensive research, especially in the past few years. Not surprisingly, most of this research has targeted the impairments found in autism, and their underlying causes.
However, what remains unimpaired can also be important. Relative strengths can play a crucial role in helping individuals compensate for deficits, leading to a more productive and fulfilling life. People without hands may learn to use their feet to grasp objects, and even to write and paint. Blind people can learn to read using touch. Compensation can also take place within the brain. For example, the right hemisphere may compensate for some left hemisphere damage, helping individuals recover from language impairments.
We have proposed — as outlined 15 January in Neuroscience and Biobehavioral Reviews — that a single brain system can compensate for numerous and diverse deficits in autism and related neurodevelopmental disorders1. This brain system is declarative memory.
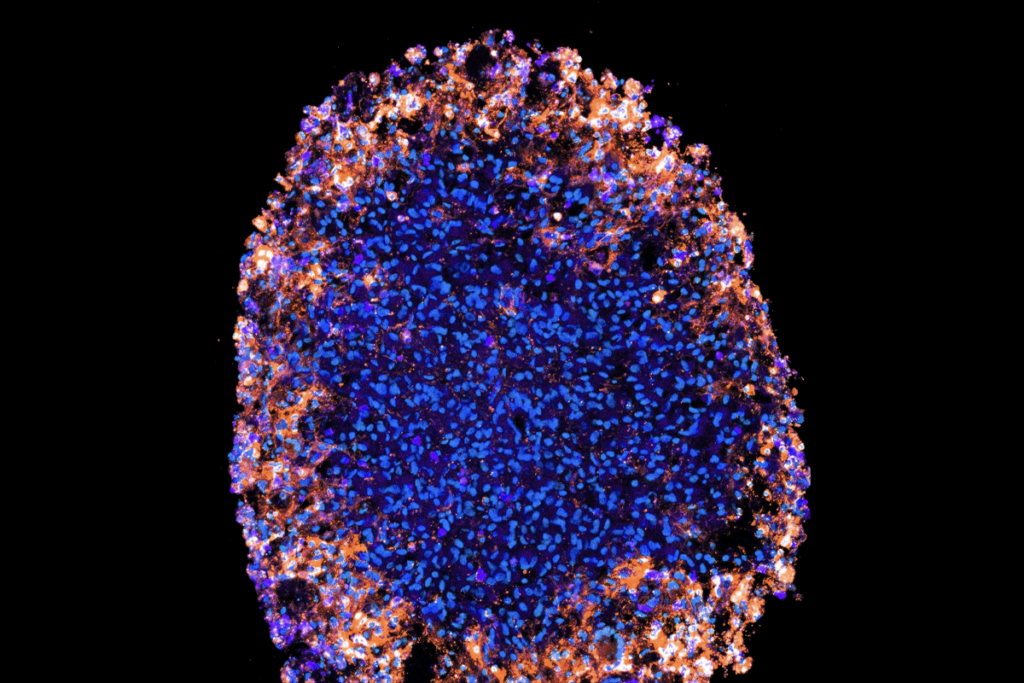
Rooted in the hippocampus and nearby structures in the medial temporal lobe, declarative memory is what we refer to when we talk about learning and memory in broad terms. It’s what we use to remember our first-grade teacher or what’s on the shopping list or the yummy risotto we had for dinner last night. It’s important for learning language, concepts, images and much more. In fact, it may allow us to learn just about anything.
Declarative memory can be thought of as the brain’s superstar for learning and memory. By contrast, other brain systems for learning and memory, such as those that help us learn movements or acquire emotional memories, appear to be more specialized.
Given its flexibility, declarative memory is a potentially powerful engine for compensation across diverse deficits and disorders. Importantly, evidence suggests that it remains largely untouched in multiple neurodevelopmental disorders, including obsessive-compulsive disorder (OCD), Tourette syndrome, dyslexia and specific language impairment (SLI). It also remains in working order in both high- and low-functioning autism, though it seems to be generally better in people with high-functioning autism2,3. Individuals across the autism spectrum can also have enhanced or even savant-like memory.
Scripts and stories:
Because declarative memory generally remains intact and is so powerful, we expect it to help individuals compensate for multiple deficits in autism and other disorders. This appears to be the case. Declarative memory seems to help individuals with autism compensate for social deficits by memorizing scripts for navigating social situations. It supports the learning of strategies to overcome language or reading difficulties not only in autism, but also in SLI and dyslexia. And it appears to help people with OCD or Tourette syndrome learn to control compulsions and tics.
Evidence for compensation by declarative memory comes from several sources. Behavioral evidence suggests that individuals with autism or other disorders often learn compensatory strategies explicitly, by consciously mastering the steps involved — a process that requires declarative memory4,5.
Temple Grandin, a noted scientist with autism, said in a 2010 interview for The Wall Street Journal, “The thing about being autistic is that you gradually get less and less autistic because you keep learning, you keep learning how to behave. It’s like being in a play.” Individuals with autism seem to instinctively turn to explicit strategies to better communicate and understand the world around them.
In fact, therapies that rely on explicit knowledge — such as scripts and stories that guide children through different social situations — seem to be particularly effective in autism and other neurodevelopmental disorders6-13.
What’s more, many people with autism use phrases and sentences that are memorized in declarative memory. Often referred to as ‘formulaic speech,’ this tactic may help people compensate for both linguistic and social deficits14-16. For example, they may learn stock phrases to help them interact with others in social contexts.
Similarly, children with SLI seem to memorize phrases to help compensate for their difficulties with grammar. For example, they may memorize ‘the mouse’ rather than combining ‘the’ and ‘mouse’ grammatically17-19.
Brain evidence from techniques such as functional magnetic resonance imaging (fMRI) also supports a role for declarative memory in compensation. A number of studies have found that people with autism, OCD or SLI, but not controls, show activation in regions of the brain responsible for declarative memory when performing tasks involving social skills, planning or grammar20-26. In some tasks that show this pattern, individuals with these disorders actually perform as well as controls, suggesting that their compensation is successful.
What’s more, correlational evidence has shown that people with SLI, dyslexia, OCD or Tourette syndrome who seem to have better declarative memory have fewer or milder deficits — such as obsessions, tics, grammar or reading problems — than those whose declarative memory is weaker27-31. We are not aware of any studies examining this type of correlation in autism. But the declarative memory weaknesses seen in people with low-functioning autism might help explain why this group is more severely affected in the first place.
Treatment tool:
Knowing that individuals with autism or other disorders may be able to use declarative memory to compensate could inform treatment. First, designing new therapies that expressly rely on declarative memory, or that improve learning in this system, might enhance compensation and thus reduce symptoms. For example, drugs known to improve declarative memory — such as acetylcholinesterase inhibitors or memantine32,33 — might ameliorate symptoms, particularly if paired with behavioral therapies that depend on explicit knowledge.
Second, designing interventions that prevent individuals from using declarative memory to compensate for their deficits might strengthen the dysfunctional circuitry. This strategy is akin to therapies that prevent stroke patients from using their good hand so they are forced to use their bad one, which can improve its functionality.
Declarative-memory-based compensation also has implications for diagnosis. Good declarative memory might mask symptoms of a disorder. Understanding that such compensation exists makes it possible to work around it. For example, diagnostic instruments could target symptoms and deficits that cannot easily be compensated for by declarative memory. Note that individuals who avoid diagnosis due to strong compensation could still benefit from diagnosis and therapy.
Underdiagnosis resulting from compensation may also help explain a major conundrum: why diagnoses of autism and related developmental disorders are more common in boys than in girls. Declarative memory seems to be better, on average, in girls and women than it is in boys and men34. As a result, girls may be better able to compensate than boys, even compensating themselves out of diagnosis more often than boys do.
Compensation by declarative memory may also be found in other disorders, including attention deficit hyperactivity disorder and debilitating adult-onset disorders such as Parkinson’s disease and aphasia, in which damage to the brain’s language centers leads to severe communication difficulties. Given the power and flexibility of declarative memory, it may play compensatory roles in a wide range of disorders.
Declarative-memory-based compensation might plausibly be widespread and could have important therapeutic, diagnostic and other implications. Further research on exactly how and when people depend on this powerful memory system could yield substantial benefits.
Sometimes it behooves us to look not where problems lie, but where they do not.
Michael Ullman is professor of neuroscience at Georgetown University in Washington, D.C. Mariel Pullman is a medical student at the Icahn School of Medicine at Mount Sinai in New York.
References:
1. Ullman M.T. and M.Y. Pullman Neurosci. Biobehav. Rev. 51, 205-222 (2015) PubMed
2. Boucher J. and A. Mayes Autism 16, 603-611 (2012) PubMed
3. Boucher J. et al. Psychol. Bull. 138, 458-496 (2012) PubMed
4. Ullman M.T. and M. Gopnik Appl. Psycholinguist 20, 51-117 (1999) Abstract
5. Landa R. (2000). In A. Klin, F.R. Volkmar and S.S. Sparrow (Eds.), Asperger syndrome. New York, NY: The Guilford Press.
6. Alexander A.W. and A.M. Slinger-Constant J. Child Neurol. 19, 744-758 (2004) PubMed
7. Ehri L.C. et al. Rev. Educ. Res. 71, 393-447 (2001) Abstract
8. Thiemann K.S. and H. Goldstein J. Appl. Behav. Anal. 34, 425-446 (2001) PubMed
9. Crozier S. and M. Tincani J. Autism Dev. Disord. 37, 1803-1814 (2007) PubMed
10. Ivey M.L. et al. Focus Autism Other Dev. Disabl. 19, 164-176 (2004) Abstract
11. Himle M.B. et al. J. Child Neurol. 21, 719-725 (2006) PubMed
12. Frank M. and A.E. Cavanna Behav. Neurol. 27, 105-117 (2013) PubMed
13. Watson H.J. and C.S. Rees J. Child Psychol. Psychiatry 49, 489-498 (2008) PubMed
14. Tager-Flusberg H. and S. Calkins J. Child Lang. 17, 591-606 (1990) PubMed
15. Dobbinson S. et al. Clin. Linguist. Phon. 17, 299-307 (2003) PubMed
16. Walenski M., Tager-Flusberg H. and Ullman M.T. (2006). In S.O. Moldin and J.L.R. Rubenstein(Eds.), Understanding autism: From basic neuroscience to treatment. (pp. 175-203). New York, NY: Taylor and Francis Books.
17. Ullman M.T. and E.I. Pierpont Cortex 41, 399-433 (2005) PubMed
18. Oetting J.B. and J.E. Horohov J. Speech Hear. Res. 40, 62-74 (1997) PubMed
19. van der Lely H.K.J. and M.T. Ullman Lang. Cognitive Proc. 16, 177-217 (2001) Abstract
20. Dichter G.S. et al. J. Autism Dev. Disord. 42, 147-160 (2012) PubMed
21. Vaidya C.J. et al. Dev. Sci.14, 911-924 (2011) PubMed
22. Rauch S.L. et al. Biol. Psychiatry 61, 330-336 (2007) PubMed
23. Rauch S.L. et al. J. Neuropsychiatry Clin. Neurosci. 9, 568-573 (1997) PubMed
24. Rauch S.L. et al. Adv. Neurol. 85, 207-224 (2001) PubMed
25. van den Heuvel O.A. et al. Arch. Gen. Psychiatry 62, 301-309 (2005) PubMed
26. Fonteneau E. and H.K. van der Lely PLoS One 3, e1832 (2008) PubMed
27. Lum J.A. et al. Cortex 48, 1138-1154 (2012) PubMed
28. Hedenius M. et al. PLoS One 8, e63998 (2013) PubMed
29. Plessen K.J. et al. J. Psychosom. Res. 67, 559-573 (2009) PubMed
30. Worbe Y. et al. Brain 133, 3649-3660 (2010) PubMed
31. Peterson B.S. et al. Arch. Gen. Psychiatry 64, 1281-1291 (2007) PubMed
32. Dommett E.J. et al. Learn Mem. 15, 580-586 (2008) PubMed
33. Repantis D. et al. Pharmacol. Res. 61, 473-481 (2010) PubMed
34. Ullman M.T., Miranda R.A. and Travers M.L. (2007). In J.B. Becker et al. (Eds.), Sex differences in the brain: From genes to behavior (pp. 291-309). New York, NY: Oxford University Press.
Recommended reading

Among brain changes studied in autism, spotlight shifts to subcortex
Home makeover helps rats better express themselves: Q&A with Raven Hickson and Peter Kind
Explore more from The Transmitter
Dispute erupts over universal cortical brain-wave claim
Waves of calcium activity dictate eye structure in flies