S
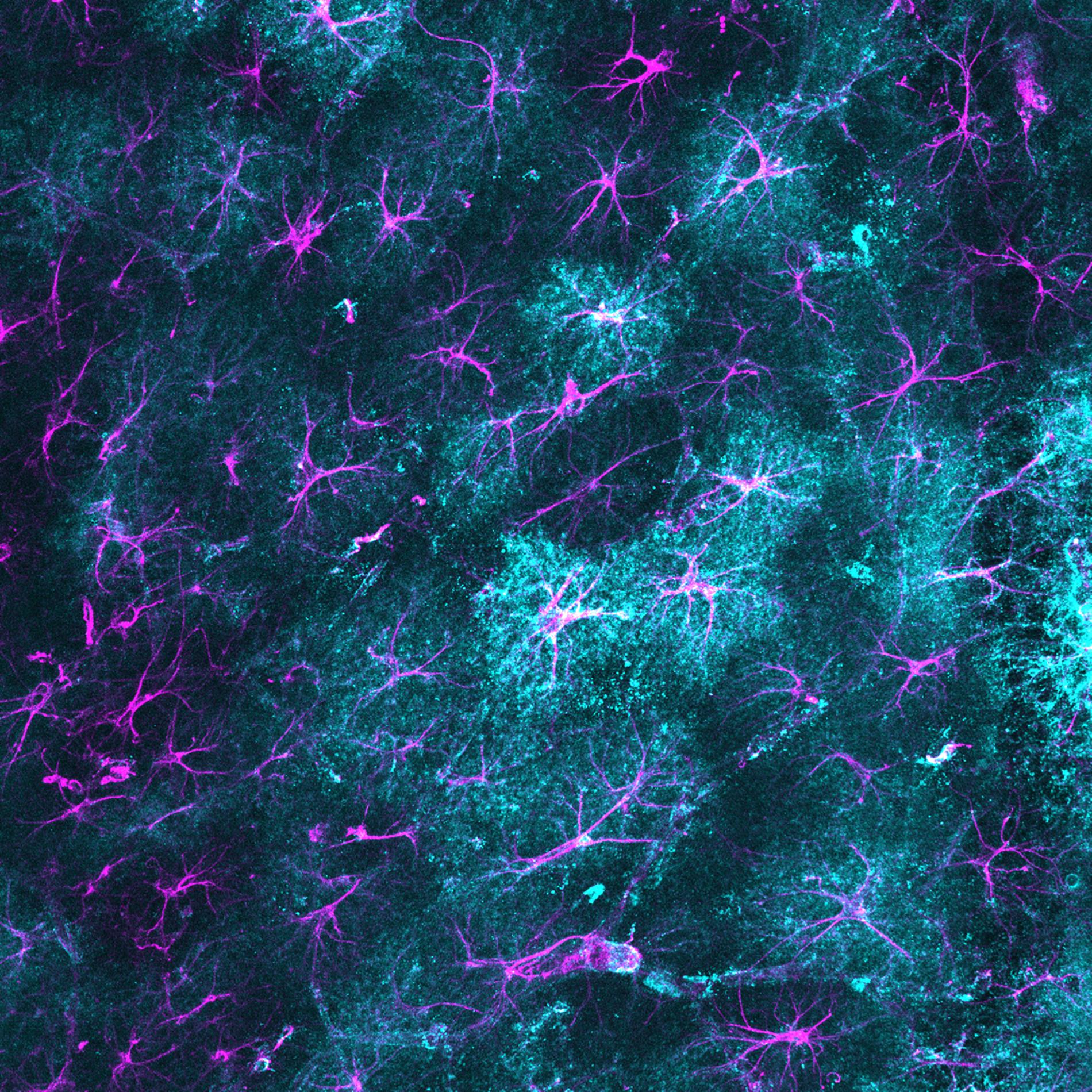
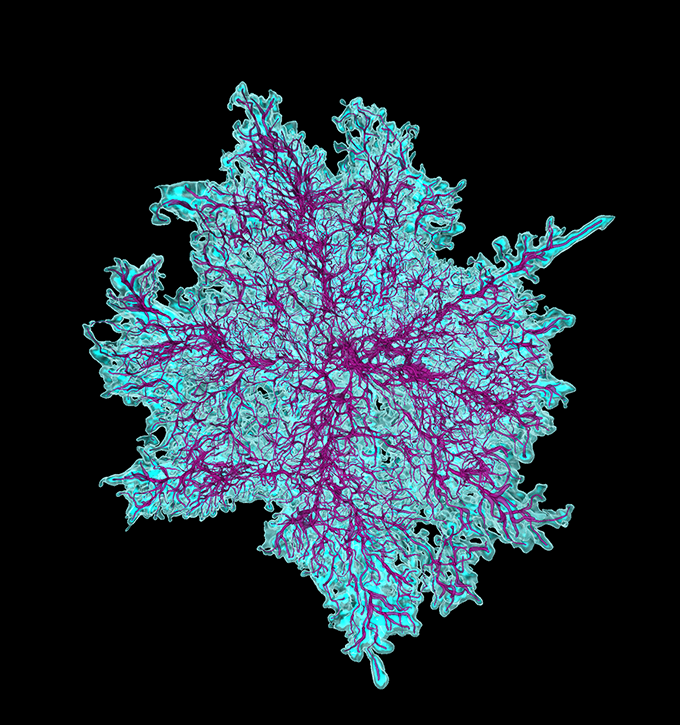
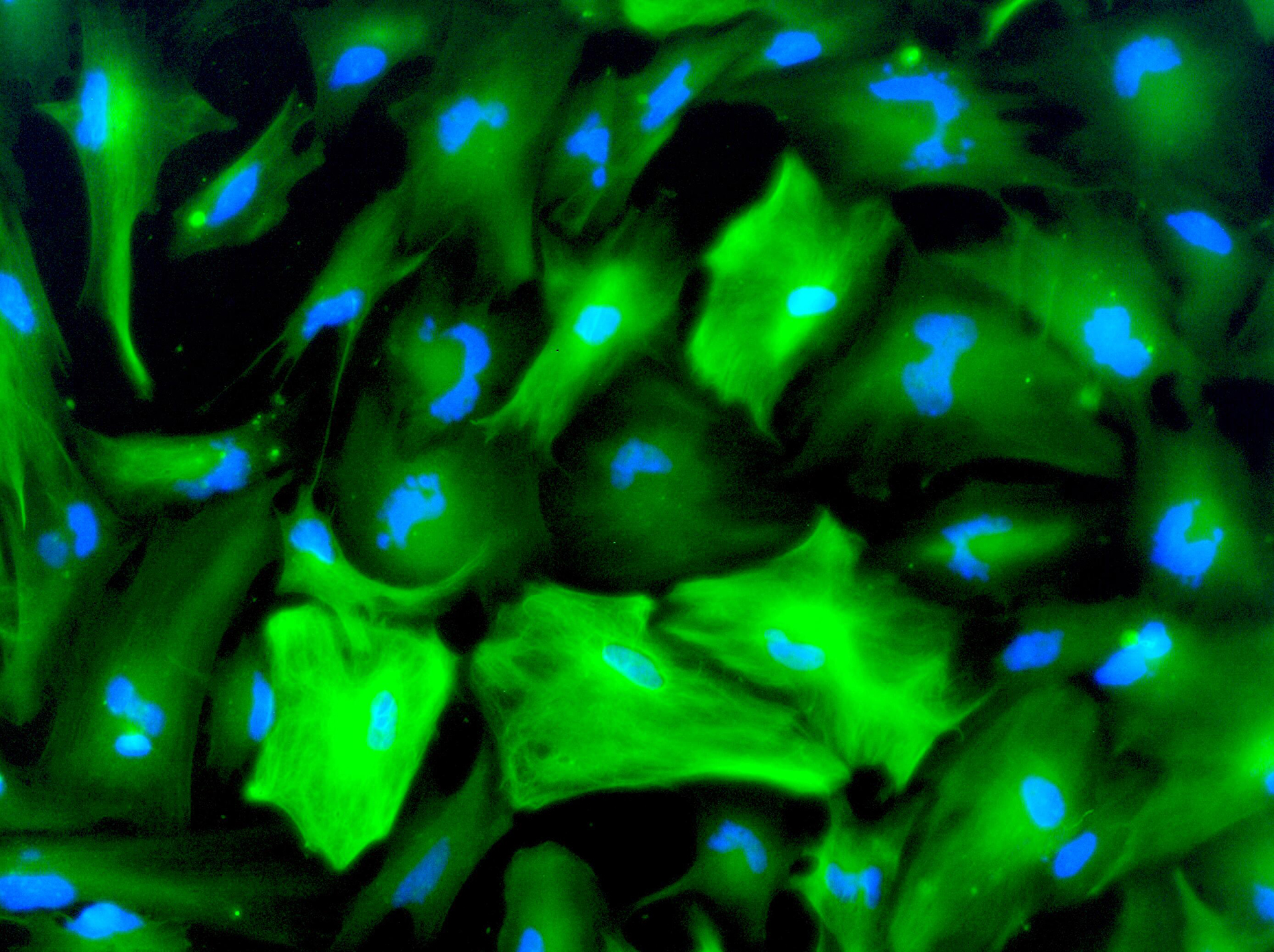
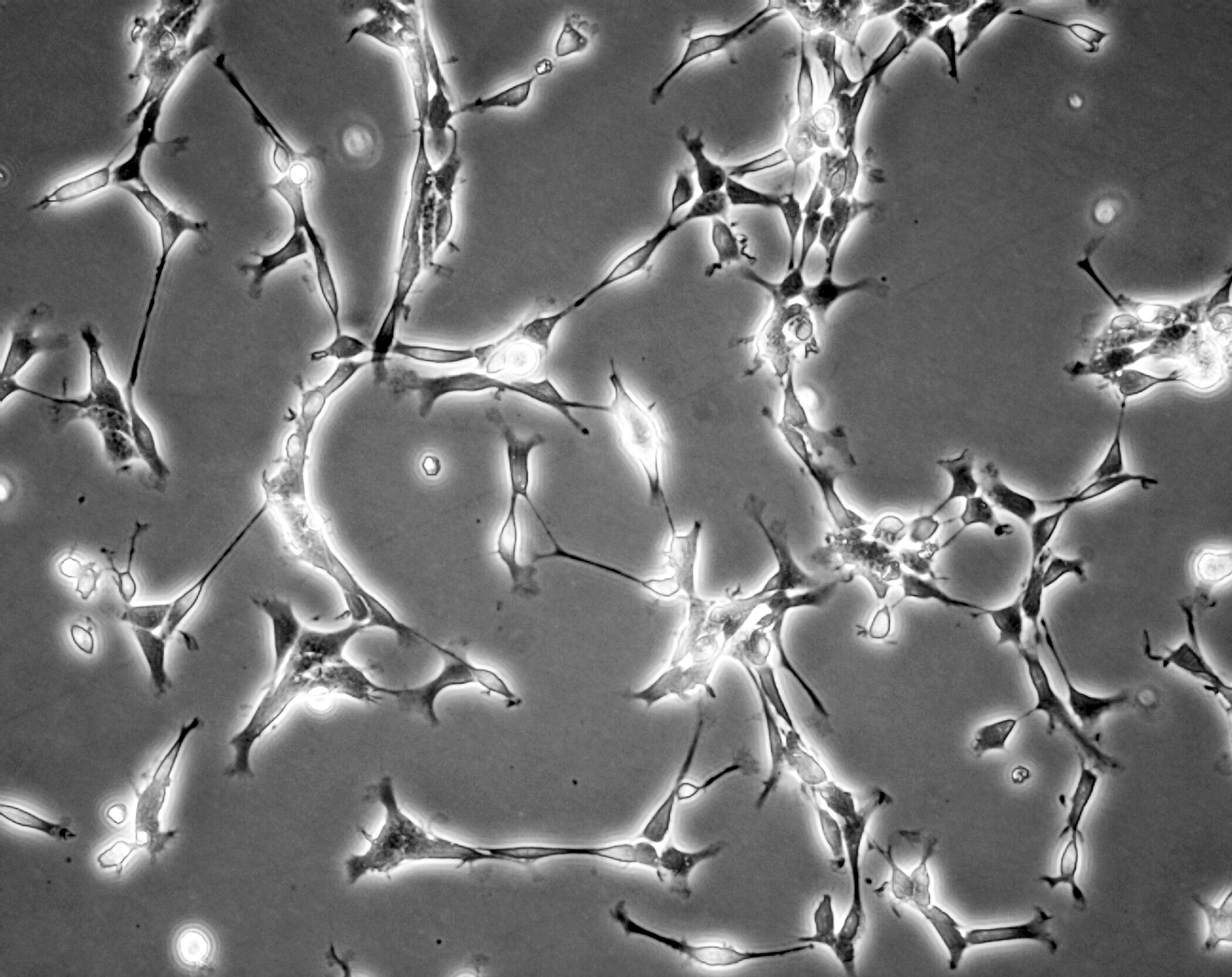
tar-shaped cells with mysterious properties: Astrocytes may sound like something out of science fiction, but they are the most abundant type of non-neuronal cell in the brain — and a growing focus for autism researchers over the past 15 years or so.“Only in recent decades we’ve started to appreciate the role of astrocytes in the nervous system and, in autism research, this followed the same trend,” says Dilek Colak, assistant professor of neuroscience at Weill Cornell Medicine of Cornell University in New York City.
The cells are known mainly for supporting roles: helping to maintain synapses, contributing to brain metabolism and helping the organ fight infection. Thanks to research on mouse models, human stem cells and post-mortem brains, however, it’s now clear that astrocytes play starring parts in autism and other neurodevelopmental conditions.
“They’re definitely emerging as key players in autism,” says Cagla Eroglu, associate professor of cell biology and neurobiology at Duke University in Durham, North Carolina, who studies chemicals astrocytes secrete during development.