Autism, some say, is all in the gut
Many cases of autism originate not in the brain, but in the gut, according to a few controversial studies published in the past year.
Many cases of autism originate not in the brain, but in the gut, according to a few controversial studies published in the past year.
Stomach upsets are among the most frequent and puzzling symptoms of autism. About 70% of children with autism have gastrointestinal problems throughout their lives, including frequent abdominal pain, constipation and vomiting, compared with 28% of typically developing children, according to a 2006 study1.
Many parents of these children say that tailored diets ― lacking wheat and gluten, dairy or both ― dramatically improve language skills, or decrease tantrums and hyperactivity, although few studies have borne out that hypothesis.
Still, the anecdotal evidence has led some researchers to ask whether the brain and behavioral abnormalities associated with autism ― and perhaps the dramatic rise in autism diagnoses ― stem from problems in the gut.
“We cannot ignore the fact that these children don’t just have something wrong with their brain. A lot of them have something wrong with their gut,” says Derrick MacFabe, director of the Kilee Patchell-Evans Autism Research Group at the University of Western Ontario.
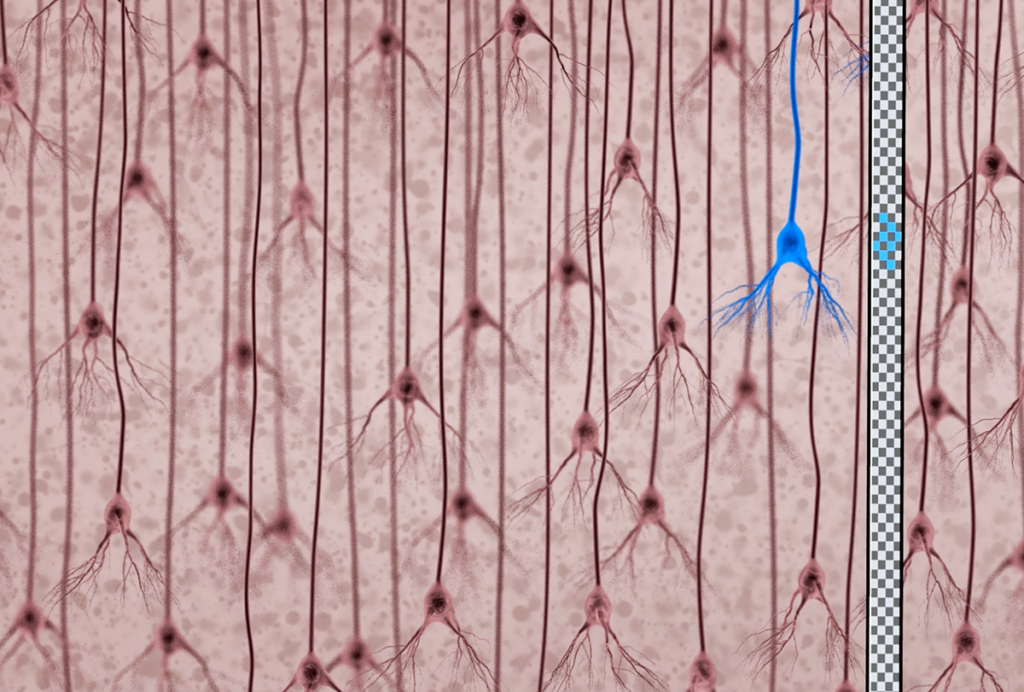
| The rat’s brain tissue shows inflammatory changes in glia and microglia (right top and bottom) similar to tissue obtained from the brains of people with autism. |
Over the past year, MacFabe has published two studies showing that in rats, fatty acids produced by gut bacteria can cause abnormal behavior and brain patterns2,3.
Few others are rigorously studying the gut’s link to autism, and many are skeptical of its ties to the field of alternative medicine. But as mounting evidence points to the heterogeneity of autism spectrum disorders, many experts agree that it’s time to start looking at possible environmental factors.
“Some of my geneticist colleagues think we’ll have to study the genes first, before we start the environmental part ― that’s a mistake,” says Martha Herbert, a pediatric neurologist at Harvard Medical School. “Each one is going to give us clues about the other, and the whole thing will move faster if we work together.”
Leaky gut:
In a healthy digestive system, wheat and milk proteins get broken down into peptides and then into amino acids. These smaller particles are absorbed by the intestine and then enter the bloodstream.
In 1991, Norwegian researchers hypothesized that children with autism have a ‘leaky gut’ that doesn’t fully metabolize these proteins, leaving them to leak into the brain and act like opiates, directly causing autism symptoms4.
However, several follow-up studies have since refuted the leaky gut theory, showing that children with autism do not have excess opioid peptides in their urine5.
In 2002, microbiologists at the University of California, Los Angeles, came up with a different gut connection. They found that, compared with normally developing children, children with regressive autism have large numbers of clostridial bacterial species in their feces.
Chemical substances made by these bacteria, they suggested, could affect the brain.
Clostridial bacteria are present in everyone’s gut, and are vital to normal digestive functions. What’s more, a high-carbohydrate diet is not unusual in modern Western diets. So why would these dramatic behavioral and neurological effects only manifest in a few children?
MacFabe says that children with autism probably have a genetic propensity that, when combined with a high carbohydrate diet or a high load of antibiotics, leads to an extreme imbalance of bacteria in their gut.
He says this idea is bolstered by the fact that children who abruptly regress into autism often do so after taking antibiotics for ear or other routine infections.
“Because there are so many biological connections between the brain and the gut and the immune system, I think a geneticist who’s enterprising enough to look for genes that play roles in all of those systems may well hit it good in investigations of candidate genes,” notes Herbert.
Bacterial byproducts:
To determine how these bacterial byproducts might affect the brain, MacFabe and his colleagues looked at propionic acid (PPA), a fatty acid that’s produced by clostridial bacteria and found in high levels in the gut.
“When we feed certain bacteria in the digestive tract refined carbs, like a lot of wheat, they produce these fatty acids,” MacFabe says.
People who, because of rare genetic disorders, have abnormally high levels of PPA are usually developmentally delayed or exhibit repetitive movements. “They’re not identical [to autism], but they have a lot of similarities with autism,” he says.
MacFabe’s team injected PPA into the lateral ventricle ― a chamber under brain surface that holds cerebrospinal fluid ― of adult rat brains. Adding PPA in this way, MacFabe says, exposes the whole brain, mimicking what happens if PPA travels to the brain through the bloodstream.
Within about two minutes of the injection, the rats become hyperactive, show repetitive movements, and have frequent seizures.
“They showed these remarkable repetitive behaviors, spinning around and turning quickly, and they also had a remarkably social impairment,” MacFabe says. The behaviors cease after 30 minutes, presumably after the animals metabolize the PPA.
The brain tissue of these rats also shows inflammation in glial cells of the hippocampus. Some post-mortem studies of brain tissue of people with autism have found similar abnormalities6.
To better mimic the scenario in humans, the researchers next plan to inject PPA into the rat’s bloodstream, rather than directly into the brain. They are also investigating the effects of other short-chain fatty acids, including acetate and butyrate, made by clostridial bacteria.
These experiments are far from conclusive, however. As with all animal models of autism, it’s difficult to define ‘autisticʼ behaviors in a rat. Nearly all of the rats injected with PPA show some degree of seizure activity, whereas between 5 to 40 percent of individuals with autism are diagnosed with epilepsy7.
“He drew a lot of comparisons to the behavioral characteristics of autism, but the high percentage of seizures isn’t really comparable to the percentage of kids with autism who have epilepsy,” says Susan Levy, director of the Regional Autism Center of the Children’s Hospital of Philadelphia.
MacFabe counters that because mild, infrequent or non-convulsive seizures are difficult to detect, seizures in children with autism are most likely under-reported.
“A lot of data now supports that there are immune factors in autism, that there are [gastrointestinal] difficulties, that there are differences in neurotransmitters both in the gut and the brain,” Levy says, “but I think it’s just one piece of puzzle.”
References:
- Valicenti-McDermott M. et al. J. Dev. Behav. Pediatr. 27, S128-36 (2006) PubMed ↩
- MacFabe D.F. et al. Behav. Brain Res. 176, 149-69 (2007) PubMed ↩
- Shultz S.R. et al. Neuropharmacology 54, 901-11 (2008) PubMed ↩
- Reichelt K. L. et al. Brain Dysfunction 4, 308-319 (1991) Abstract ↩
- Cass H. et al. Arch. Dis. Child. (2008) Epub ahead of print. Abstract ↩
- Vargas, D.L. et. al. Ann. Neurol. 57, 67-81 (2005) PubMed ↩
- Canitano R. Eur. Child Adolesc. Psychiatry 16, 61-66 (2007) PubMed ↩
Recommended reading

Expediting clinical trials for profound autism: Q&A with Matthew State

Too much or too little brain synchrony may underlie autism subtypes
Explore more from The Transmitter

Mitochondrial ‘landscape’ shifts across human brain