What the placenta could reveal about autism
Understanding the interactions between the placenta and the uterine lining could explain how maternal immune activation leads to autism.
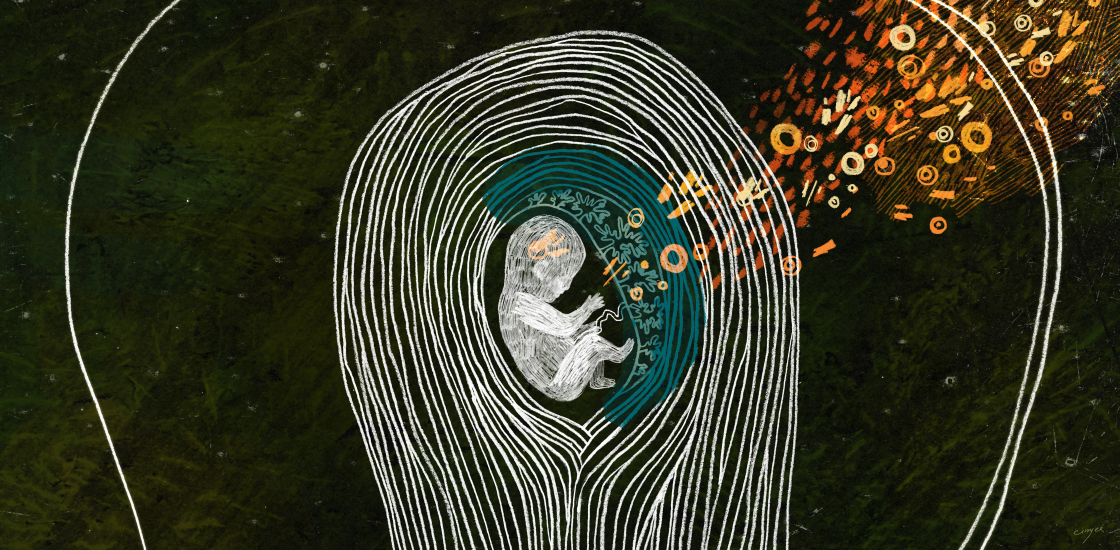
Activation of a mother’s immune system during pregnancy can increase the risk of autism in her child. New clues to the link could come from studying the placenta and the place in the womb where it resides.
The placental-uterine boundary is famously the fetus’ lifeline. Nutrients cross from the mother to her fetus across this channel, and wastes flow back for removal. The interface does more: It also protects the fetus from infections and helps keep the mother’s immune system from attacking the fetus.
A better understanding of what happens at this interface — both under ordinary circumstances and after maternal immune activation — may reveal how immune activation disrupts fetal brain development.
In the past few years, researchers have made progress in pinpointing important details of this process. They have developed tools for unraveling the molecular biology of the interface and identified several types of immune molecules that could harm the fetal brain.
Molecular dance:
We have known for some time that the mother’s immune system changes in pregnancy. Immune cells called cytotoxic T cells are suppressed because they can destroy the placenta and fetus, which they treat as a foreign body. (These are the same cells responsible for rejecting organ transplants.)
By contrast, immune cells called B cells remain protective. These cells produce antibodies that cross the placenta to the fetus and ward off pathogens. The antibodies may persist in, and protect, the newborn for months. Another class of immune cells called natural killer cells both fight invaders and combat the cytotoxic T cell response. Signaling molecules called cytokines, such as interleukin-10 and TGF-beta, also help maintain the mother’s immune tolerance of the placenta and fetus.
Many of these alterations take place at the interface between the uterine lining and the placenta, so researchers are working to decode the immune communications at this location.
In a study last year, researchers profiled gene expression in tens of thousands of cells taken from first-trimester placentas, along with those from the blood and uterine lining of the mothers. They used these profiles to generate an atlas of cell types and molecular interactions at this boundary, some of them previously unknown.
They learned that natural killer cells in the maternal tissue come in three main types. They also identified a range of molecules that restrain maternal immune responses.
Their findings reinforce the idea that the maternal-fetal interface regulates the balance between protection against infection and a healthy pregnancy, and indicate that this balance depends on the interplay of numerous molecules.
Brain changes:
Researchers can use the atlas to study how this intricate dance of molecules changes under certain circumstances — say, when a pregnant animal is exposed to a virus or is under stress. Some of these changes may affect the fetal brain and, consequently, autism risk.
Some groups have already uncovered hints about how maternal immune activation might disrupt fetal brain development. For instance, even mild immune activation in mid-pregnancy can alter the mouse placenta, depriving the fetus of oxygen and stunting the growth of neuronal precursors in the fetal brain1. The timing of the immune activation matters: The placenta appears to be more resilient later in gestation.
Other teams are exploring how maternal immune activation affects the brain through changes at the uterine-placental boundary. Some work suggests that certain potentially damaging molecules secreted by activated immune cells, such as interleukin-6, can make their way to the placenta or the fetus, or both, and alter the way the brain develops2. If this is true, efforts to block these secreted factors during pregnancy might help protect the fetus.
To fully decipher the link between a pregnant woman’s immune activity and autism, researchers need to look at all aspects of the maternal immune system. For instance, my own work suggests that some women are genetically predisposed through loss of immune regulation to produce antibodies that recognize proteins in the developing brain. These ‘autoantibodies’ recognize the same proteins in the mother; they can cross the placenta during pregnancy and bind to and harm the fetal brain3. This genetic predisposition may partly explain why autism only sometimes follows a maternal infection.
Judy Van de Water is professor of internal medicine at the University of California, Davis.
References:
Recommended reading

New organoid atlas unveils four neurodevelopmental signatures
Explore more from The Transmitter

The Transmitter’s most-read neuroscience book excerpts of 2025

Neuroscience’s leaders, legacies and rising stars of 2025


