Oxytocin boosts social skills in autism-related syndrome
One week of treatment with the hormone oxytocin improves social skills and feeding in infants with Prader-Willi syndrome.
One week of treatment with the hormone oxytocin improves social skills and feeding in infants with Prader-Willi syndrome1.
About one in four children with the syndrome also have autism2. So the findings, from a new clinical trial, suggest that the hormone may also ease social difficulties in people with autism.
“Oxytocin may be a possible early treatment that can modify social skills,” says lead investigator Maïthé Tauber, professor of pediatrics at the University of Toulouse in France. The work appeared in the February issue of Pediatrics.
Prader-Willi syndrome results from a loss of expression of genes inherited from fathers in a chromosomal region called 15q11-13. Mutations in one of these genes, called MAGEL2, are linked to autism.
People with Prader-Willi syndrome have low brain levels of oxytocin, as do mice that lack MAGEL23,4. The mice also show autism-like social difficulties. A 2015 study showed that these problems disappear in mice after daily injections of oxytocin for a week shortly after birth5.
The new study extends the findings to people.
The study is small and lacks a control group of babies who did not receive treatment. But it represents “a promising first step,” says Alexander Kolevzon, professor of psychiatry and pediatrics at the Icahn School of Medicine at Mount Sinai in New York, who was not involved in the research. “It draws from translational research in animal models, and that general developmental strategy, to me, is an important one.”
Short course:
Newborns with Prader-Willi syndrome have difficulty sucking and swallowing, and typically require a feeding tube. They also have life-threatening breathing problems.
Tauber and her colleagues delivered liquid oxytocin into the noses of 18 infants under the age of 6 months with the syndrome. The babies received the hormone either every other day, every day or twice a day, for a week.
A speech and language pathologist rated the infants’ sucking patterns and swallowing before and after treatment. Two other researchers, who were unaware of which dose each child received, judged the infants’ social skills and interactions with their mothers. The researchers also collected blood samples and assessed brain activity patterns using functional magnetic resonance imaging.
The treatment normalized sucking and swallowing in all but two of the infants, no matter the dosing regimen. Of the 15 babies whose social skills the researchers evaluated, 12 were more active, expressive and engaged with their mothers after treatment than they were before. None of the babies had adverse reactions to oxytocin.
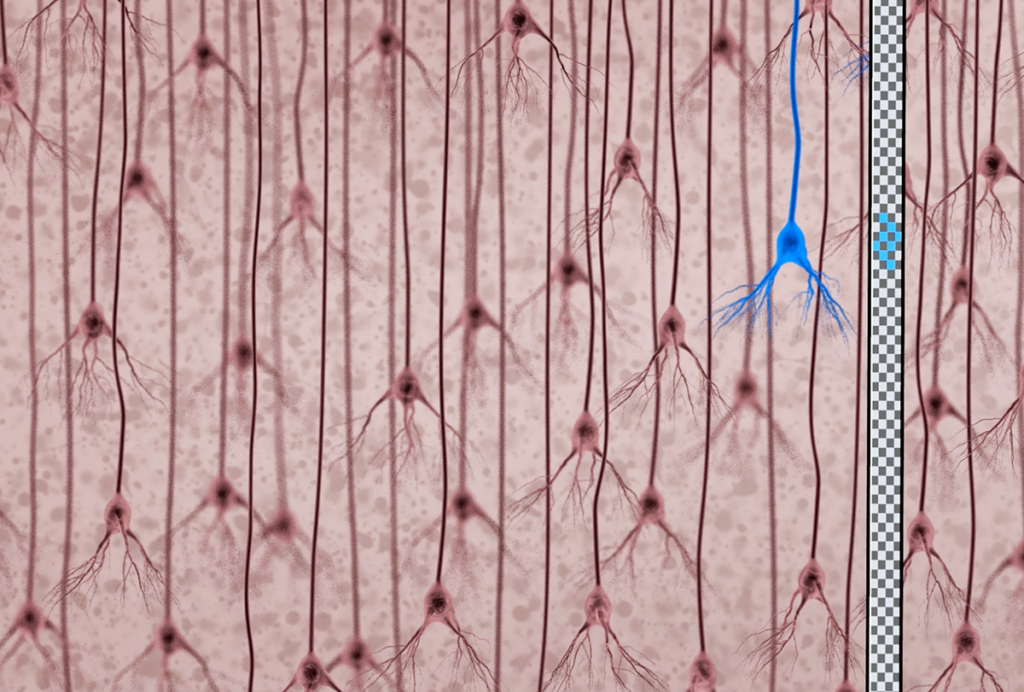
The babies’ behavioral changes were accompanied by an increase in their blood levels of ghrelin, a hormone that regulates appetite. The babies also showed an increase in the synchronous activation of brain areas within the right superior orbitofrontal cortex, which processes tastes and smells, as well as other people’s gestures and facial expressions.
Lasting impact:
The researchers re-evaluated 16 of the children when they were 1 to 3 years old and compared them with 16 toddlers with Prader-Willi syndrome who had not received oxytocin. They found that 81 percent of the treated children could crawl, compared with only 13 percent of the untreated toddlers.
This finding suggests that oxytocin leads to lasting changes in motor abilities.
The researchers also observed that the treated toddlers appeared to have better social skills and were more engaged with others than those who had not received oxytocin.
“They only get it for a week — that’s pretty wonderful, because you’re not dealing with a chronic situation that requires the child to constantly get the drug,” says Sue Carter, executive director of the Kinsey Institute at Indiana University, who was not involved in the study. It is unclear how the findings relate to the early treatment of autism, which is diagnosed after infancy, Carter says.
The benefits seen in the Prader-Willi children could be inflated, because the study’s open-label design means that the parents and researchers (with the exception of the social skills raters) knew which treatment the children received. “The responses are very dramatic,” Kolevzon says. “But when you do an open-label study, there’s a heavy risk for bias.”
Tauber says her team plans to try to replicate the results in a larger trial with a control group that receives a placebo treatment.
References:
- Tauber M. et al. Pediatrics 139, e20162976 (2017) PubMed
- Bennett J.A. et al. Am. J. Med. Genet. A 167A, 2936-2944 (2015) PubMed
- Swaab D.F. et al. J. Clin Endocrinol. Metab. 80, 573-579 (1995) PubMed
- Schaller F. et al. Hum. Mol. Genet. 19, 4895-4905 (2010) PubMed
- Meziane H. et al. Biol. Psychiatry 78, 85-94 (2015) PubMed
Recommended reading

Expediting clinical trials for profound autism: Q&A with Matthew State

Too much or too little brain synchrony may underlie autism subtypes
Explore more from The Transmitter

Mitochondrial ‘landscape’ shifts across human brain