Owen’s odyssey: A year and a half after an autism diagnosis
This is part 2 of Owen’s story. It tracks his early progress in treatment for autism. Part 1 described his difficult path to a diagnosis.
O
n a sunny morning in late August, 4-year-old Owen Couture, who has autism, sat on the floor of his family’s living room. “How many activities do you want? Three or four?” asked Megan Ricci, a behavior technician with Prism Autism Center, a school-like medical facility near Owen’s home in Cheshire, Connecticut.They settled on three and laid them out on the floor, each marked with a number: 1) a set of tangrams, 2) a puzzle of a train, 3) a snap-together cardboard fort just the right size for Owen to hide in. Owen’s favorite was the fort, which he called “boxes.” If he worked through the activities in order and on his own, without getting distracted, playing in the fort for a few minutes would be his reward, Ricci explained.
Ricci set a timer for 10 minutes, and Owen got to work. He put together a bee and a butterfly with the tangrams. After looking around the room, briefly distracted, he scooted over to the puzzle. “Hey, where’s the last piece?” he asked, but quickly found it in the box. “Here it is!”
Next, Owen moved to the cardboard fort, opened the door Ricci had attached to it, and hid inside. He popped his head out and hid again repeatedly, delighting himself each time. When the timer went off, he ran over to Ricci. “You did it!” she exclaimed. They jumped up and down together, cheering Owen’s progress.
There is much to celebrate. In September 2019, when Owen began intensive behavioral therapy at Prism, he could not play independently or put puzzles together on his own. He was unable to complete tasks without getting distracted, or to speak in full sentences. Back then, Owen tended to fixate on one toy for long stretches of time and to repeat other people’s words, a speech trait known as echolalia.
Spectrum went back to check in on Owen after following his story leading up to an autism diagnosis in May 2019. For many families — the Coutures included — getting an autism diagnosis is a long and difficult journey. Owen’s mother, Danyel Couture, spent two stressful years sharing her concerns about Owen’s delays and being told there was nothing wrong.
But the diagnostic odyssey often leads to another: finding services. The options depend on multiple variables, including the severity of the child’s autism traits, where the family lives and what resources are available. Both the quality and quantity of services vary between and within states, although most fund early-intervention programs for children under age 3 and provide services to older children through the school system.
How autistic children respond to therapy also varies tremendously. Roughly half of children do well with early intervention, and the other half make less rapid progress, says psychologist Aubyn Stahmer of the University of California, Davis MIND Institute. When started at around 18 months, but certainly before age 3, early intervention can boost social-communication skills and cognitive abilities, and ease challenging behaviors. “There are young children with early presentations of autism who can make dramatic progress, while others will follow a more moderated trajectory of improvement,” says psychologist Zachary Warren of Vanderbilt University in Nashville, Tennessee. It takes time to know what a child’s rate of progress will be, he says, but “there is a lot of hope in that first year.”
Over the longer term, children tend to fall into one of three groups. One group begins with significant cognitive or social delays, or both, that do not ease much. “They’re making progress, but they’re still staying behind their peers,” Stahmer says. Another group begins with stronger skills and makes steady improvement. The third group starts out quite delayed but makes significant progress.
The Coutures are feeling hopeful, they say. They are fortunate that the Yale Child Study Center, where Owen was diagnosed, referred them to Prism and Owen started therapy right away. Many parents are not even aware that facilities such as Prism exist. And although the COVID-19 pandemic disrupted services, the family was able to get a therapist to come to their home every day. During the past six months, Owen has done remarkably well. “It’s like he’s a different child,” Couture says.

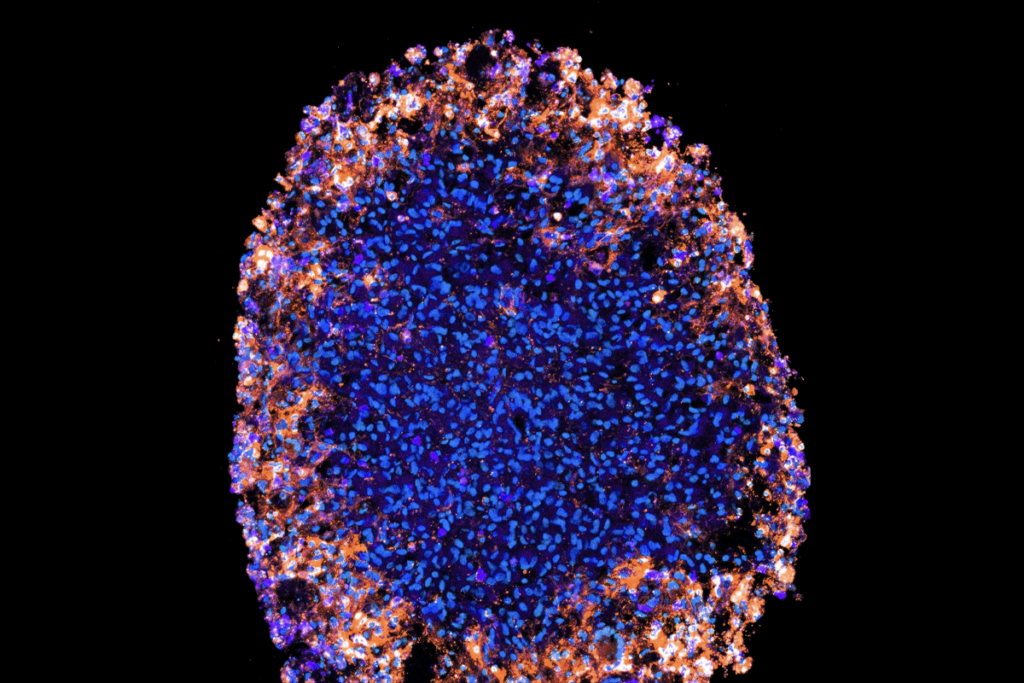
Drum roll: Owen’s love of music plays into his autism therapy.
October 2019:
W
hen Owen started at Prism in late September 2019, he took to his new routine rapidly. His father, Christian Couture, drove him to Prism each day. On the way, they listened to some of Christian’s favorite bands, including Phish, Daft Punk and Bon Iver. “They jam out,” Danyel Couture said in October last year.At Prism, Owen’s therapist met him outside every morning, and he happily took her hand to go inside. Although Prism is a medical facility, it looks a lot like a preschool, with bright decor and toys everywhere. Owen spent his days with four or five other children in a treatment room, where there was free-play time and stations set up for different activities. Like any classroom, they held morning meeting and circle time, and then each child was pulled out for individualized teaching.
Although Owen was 3 years old when he started, he tested more like a 1-year-old on social skills and a 2-year-old on language abilities, such as understanding what others say (receptive language) and verbalizing thoughts (expressive language). “Owen was very shy,” says behavior analyst Anton Yurack, who oversees Owen’s treatment. “He didn’t use much language.”
Owen also had trouble making eye contact and a limited ability to direct his attention to the same object or event as another person’s — a key skill called joint attention. Owen did not initiate conversation with or respond to the other children. He looked at them with interest but did not, in fact, interact with them at all. “He showed a desire to be social with others but didn’t yet have the skills to do so properly,” says Rebecca Giammatti, co-founder and chief clinical officer of Prism.
Teaching Owen how to play — which is essential for all learning and developing peer relationships — was an early priority. Like many other autistic children, Owen tended to play with just one thing for unusually long periods of time and not in the usual way: He would spin the wheels of a toy wheelchair but not make it move, for example. “We spent a long time teaching Owen the ins and outs of how we play, how we build with blocks, how we make a sandwich and give it to someone, and they pretend to eat it,” Yurack says.
With the help of a behavior technician, Yurack also modeled for Owen how to interact with other children, saying hello and responding to comments in ways that invited connection. For instance, if someone said, “I have a green shirt,” Yurack might prompt Owen to say, “Oh, I have a red shirt today.” And they worked on eye contact, too. “Every time Owen would hand us something, we would wait for him to look at us, to make that connection,” Yurack says.
These tactics are all part of the Early Start Denver Model (ESDM), an intervention that incorporates the teaching of new skills into play. It is a variation of applied behavior analysis (ABA), a one-on-one therapy based on rewarding children for desirable behaviors, but ESDM focuses more on developmentally appropriate skills and communication and less on compliance. Termed ‘naturalistic’ interventions, ESDM and similar therapies incorporate a child’s daily activities and interests, and include parents as partners. And they are generally thought to work. “The data from the past 20 years are pretty clear that naturalistic developmental behavioral interventions are really the state of the art and the best for kids,” Stahmer says.
Owen proved to be a quick learner. His social skills, play behavior and expressive language all improved in the first few months of therapy. He soon was saying hello to his peers right away when he entered the room in the morning. He was able to take turns, to play pretend or chase. “He developed some significant relationships,” Yurack says.
Danyel Couture saw the changes, too. Before therapy, she says, Owen often ran away from other children. But within weeks of starting therapy, when he encountered other children at his siblings’ soccer games, he brought his soccer ball up to them and asked them to play. His expanded use of language was also obvious at home. “I started noticing he was singing new songs,” Couture said in October last year. And he began to answer her questions more fully. “It used to be me asking questions and him responding with the exact same response.” If she asked what he’d had for lunch, he always said waffles, for instance. And when she asked what he had done that day, he would tell her he had played outside, even when it was raining. But two months into therapy, Owen accurately reported what she had packed in his lunchbox. “It’s blowing me away,” Couture said at the time.
By December, Owen was telling his mother about his day on their drive home every afternoon. “He tells me about other kids he’s met and describes them, their names, how old they are,” Couture says. “He’s learning social cues about how to interact in the world.” And Couture began to see Owen’s sense of humor emerge. When they were riding in her sister’s car, for example, Owen told his aunt that her car was “snazzy.” It was not a word Couture had ever used, but she says, “My sister does have a snazzy car.”
Owen’s progress was such that Couture found herself back where she had started, having to convince people that her son has autism. Owen’s skills were much improved, but she could still see the signs of autism. At family gatherings and other busy events, Owen was sometimes overwhelmed and needed to be alone. “He breaks down and gets sad,” Couture said in December. “People will say, ‘Why does he take so many naps? You coddle him too much.’”

Recipe for success: Owen learns to follow a series of steps to make pizza.
March 2020:
A
fter the COVID-19 pandemic hit, Prism gave families the option of returning to the center, switching to home-based services or signing up for telehealth guidance and coaching for parents, who could then work with their children on their own. At one point, the center closed briefly for a deep cleaning after 12 of the 39 staff members tested positive for the virus, though only 2 were symptomatic.Several families at the center chose telehealth, out of health concerns, at a potential cost to their child’s progress. The loss of similar services has led to real setbacks elsewhere. “Parents are being tasked with not just being a teacher but also being an occupational therapist or a speech and language therapist, in addition to being a cruise director of activities and a gym coach,” says psychologist Stephanie Lee of the Child Mind Institute in New York City. “If we can maintain and not regress, that should be considered a win.”
For Prism families who opted to work with their children by themselves, Yurack and his colleagues continued to help as much as possible. “We did as much training as we could fit in to support that parent to create a structure, to build consistency, to think of ways to implement play activities, things like that,” Yurack says. Data suggest that coaching parents to interact in specific ways with their children can improve a child’s social and related behaviors, though much of the evidence is in infants and involved in-person training before the pandemic. Still, with one family, Yurack used video conferencing to walk the father through ways of encouraging his son to switch between activities, which was difficult for the boy. Though limited, the interaction provided “a feeling of observing in the moment so that you could coach parents through challenging situations,” Yurack says.
The Coutures chose to move Owen’s services to their home — a switch that meant changing behavior technicians. Ricci started working with Owen from 9 a.m. to 2 p.m. every day, with help from Yurack, who has continued to oversee Owen’s progress, and Greta Russell, another behavior analyst at Prism. Yurack and Russell join Ricci at the Coutures every Friday and provide her with guidance by video chat other days.
In June, they hit a rough patch. “I would walk in, and he would just say, ‘No,’” Ricci says. “He would walk away or run away.” She suspected that Owen knew her arrival meant it was time to work. So the Prism team took a lot of time to reinforce Ricci’s rapport with him. For example, they made a point to start each day just playing and engaging in activities Owen wanted to do, as often as possible — like playing with dinosaur stickers and dinosaur books. “We worked hard to come back,” Ricci says, using “anything that doesn’t seem like work.”
The shift to home therapy, despite its challenges, turned out to have some unexpected benefits. At the center, Owen had been quiet and easy-going. At home, a different side of Owen appeared. “Danyel could not walk upstairs to do laundry and leave him alone or with the technician,” Yurack says. “He would engage in high rates of problem behavior — hitting Mom, pulling on her clothing, tantruming, crying, wanting to be held.” Moving therapy into the Coutures’ home made it possible for the technicians to address those challenges more directly.
The Prism team also noticed that at home Owen fixated on inanimate objects, such as fans and lights, and displayed some restricted and repetitive behaviors. “Owen had to do the same thing every day,” Yurack says. “He had to sit in the same chair when he had lunch. He would not allow his father to enter the room to say goodnight to him. It had to be Mom. He had to close the blinds.” The Coutures had not realized quite how unusual this behavior was.
Yurack and the team set up systems to teach Owen to be calm and to be away from his mother. “It took a lot,” Yurack says. They started by having his mother step into the next room just for a second and then pop back in. Each time Owen stayed calm, he received positive reinforcement. “We’d say, ‘Oh yeah, buddy!’” Yurack says. Owen also earned tokens toward an object or activity he enjoyed. One reward took advantage of Owen’s love of music, nurtured during car rides with his father, and gave him a chance to watch a clip of a favorite band performing at the Austin City Limits music festival. While working on his separation anxiety, the reward was simply being reunited with his mother.
“The bright side of COVID for me is that we’ve really changed their family’s life,” Yurack says. “I don’t know if we would have been able to do that if Owen continued at the clinic.”





Card game: Therapists Anton Yurack and Greta Russell evaluate Owen’s skills.
Mirror me: In another assessment, Owen tries to copy Yurack’s moves.
High five: Therapist Megan Ricci reinforces Owen’s success on a task.
No waffling: Owen has learned how to tell his mother what he had for lunch.
Dance break: Even between lessons, Owen follows Ricci’s lead.
September 2020:
D
uring a visit with the family at the end of August, Owen’s progress was plain to see. Wearing blue shorts printed with dinosaurs, he laughed while Ricci read him a book called “Three Little Dinosaurs,” in which the young dinosaurs make pine-cone pie and try to fly (no dinosaurs get hurt). Through the course of that day, he practiced writing his name, showed that he had mastered recall of patterns by laying out repeating sequences of shapes (star-triangle-square, star-triangle-square … ), and he followed a multistep recipe for making Chex Mix for a snack.“Hey Dad, I cooked snack!” he cried when his father came into the kitchen. Later, Owen happily ran down to play in the basement with Ricci and Russell while Yurack stayed upstairs with Owen’s parents. The separation anxiety appeared to be a thing of the past.
With so much success, the Prism team recommended that Owen transition to mainstream preschool with support — which might have happened were it not for the pandemic. Worried that COVID-19 would disrupt school and leave them with no services, the Coutures are continuing in-home services this year. “He’s doing awesome,” Couture says. “We didn’t want to risk losing Megan. Consistency is key.”
Owen’s progress has been unusually rapid, Giammatti says. Prism has about 48 children coming into the facility and another 10 getting in-home services. Because autism is reliably diagnosed at earlier ages now, many children come to Prism as infants or toddlers. And each year, as many as six Prism children are ready to transition to mainstream schools with support, most having spent at least 18 months, and sometimes several years, in therapy.
Owen’s plans for school may be on hold, but Couture is thrilled with her son’s progress. In September, she sent Yurack an email. “I want to tell you the coolest thing happened,” she wrote. She had given Owen directions to go upstairs, put his pajamas on and come back down. He did it with no questions while Couture finished her work and started dinner. “Six months ago, that would never have happened,” she wrote. “He couldn’t leave me. He had no idea how to get dressed.” It was a clear sign that Owen is on his way toward everyone’s shared goal: being able to live a fully independent life.
With additional reporting by Nicholette Zeliadt.

Going places: With therapy, Owen has largely overcome his separation anxiety.
Recommended reading

Among brain changes studied in autism, spotlight shifts to subcortex
Home makeover helps rats better express themselves: Q&A with Raven Hickson and Peter Kind
Explore more from The Transmitter
Dispute erupts over universal cortical brain-wave claim
Waves of calcium activity dictate eye structure in flies