Brain organoids — nodes of neural tissue grown from stem cells — showed new potential to mimic autism-linked conditions in two unpublished studies presented last week at Neuroscience 2022 in San Diego, California.
In one of the studies, researchers generated cortical organoids that carry a mutation in the gene CDKL5, which causes CDKL5 deficiency disorder (CDD) — a condition linked to synaptic defects, epileptic seizures and autism traits. Researchers grew clusters derived from the cells of a person with CDD, along with control organoids derived from the cells of that person’s mother, who does not have the condition.
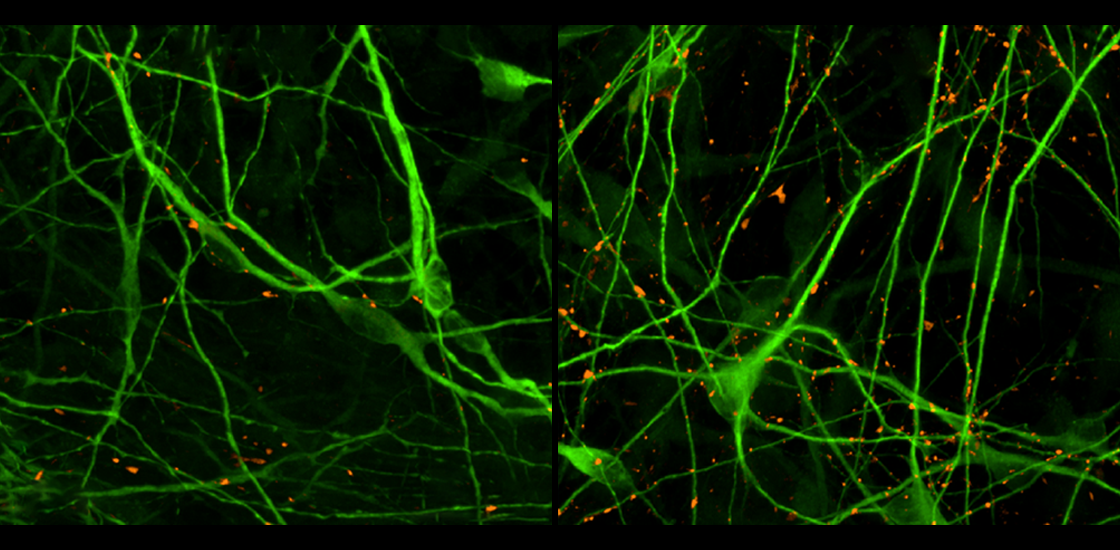
Both sets of organoids are made mostly of excitatory neurons and astrocytes, but they also contain immature neurons, oligodendrocytes, inhibitory neurons and neural progenitor cells, according to single-nuclei RNA sequencing. The CDD organoids display significantly stronger and more frequent calcium-signaling spikes than the controls do, and they have more synapses.
Among 5,000 different drug candidates the team exposed the organoid batches to one at a time, 22 reduce the number of calcium spikes in the CDD group but not in the controls.
The researchers are screening similar compounds that theoretically hit the same target as the 22 in the organoids, to home in on the drugs’ shared mechanisms of action.
“Rather than something that’s just treating symptoms, we want to be hitting something that’s in the pathway of CDKL5,” says study investigator Matthew Green, screening scientist at VyantBio, a drug discovery company in Cherry Hill, New Jersey.
A
n independent study employed ‘assembloids,’ clusters of cells representing multiple brain regions — in this case, the striatum and the cerebral cortex — to examine the effects of deletions in chromosomal region 22q13.3, which cause Phelan-McDermid syndrome. People with Phelan-McDermid have speech problems, seizures and, often, autism.These assembloids, grown from cells donated by people with the condition, grow long-range neuronal projections that form synapses with distant neurons and show neuronal activity that is not seen in striatal organoids, according to a 2020 study.
The unpublished findings include new data on calcium activity in the complex organoids, says study investigator Yuki Miura, research scientist in the lab of Sergiu Pasca, associate professor of psychiatry and behavioral sciences at Stanford University in California.
In three sets of assembloids grown from cells of people with a 22q13.3 deletion, Miura and his colleagues found no significant size difference compared with three sets of control assembloids. They also saw that neuronal projections had grown to unite the cortical and striatal sections of both sets, as evidenced by calcium signaling in striatal neurons in response to optogenetic activation of the cortical sections.
The 22q13.3 assembloids, however, showed reduced network synchronization indicative of synaptic defects — results that are consistent with what is seen in people and mice, he says. The similarity supports the usefulness of organoids for experimentation and drug screening to address the clinical effects of this variant, such as seizures.
“We can see synaptic formation, but I want to improve the system with more mature cells, which can capture a later time point of development,” Miura says. He is also working on adding more cell types and additional brain regions to the model.
Read more reports from Neuroscience 2022.