Neurons that inhibit brain signals are key in Rett syndrome
Deleting MeCP2 from a subset of neurons that mediate inhibitory signals recapitulates many of the symptoms of Rett syndrome in mice. Conversely, expressing the gene only in that subset, but not in the rest of the brain, protects the mice from some of those same symptoms. The results were published last week in Nature Neuroscience.
Deleting MeCP2 from a subset of neurons that mediate inhibitory signals recapitulates many of thesymptoms of Rett syndrome in mice. Conversely, expressing the gene only in that subset, but not in the rest of the brain, protects the mice from some of those same symptoms.
The results, published last week in Nature Neuroscience, suggest that this group of neurons is intimately involved in Rett syndrome1.
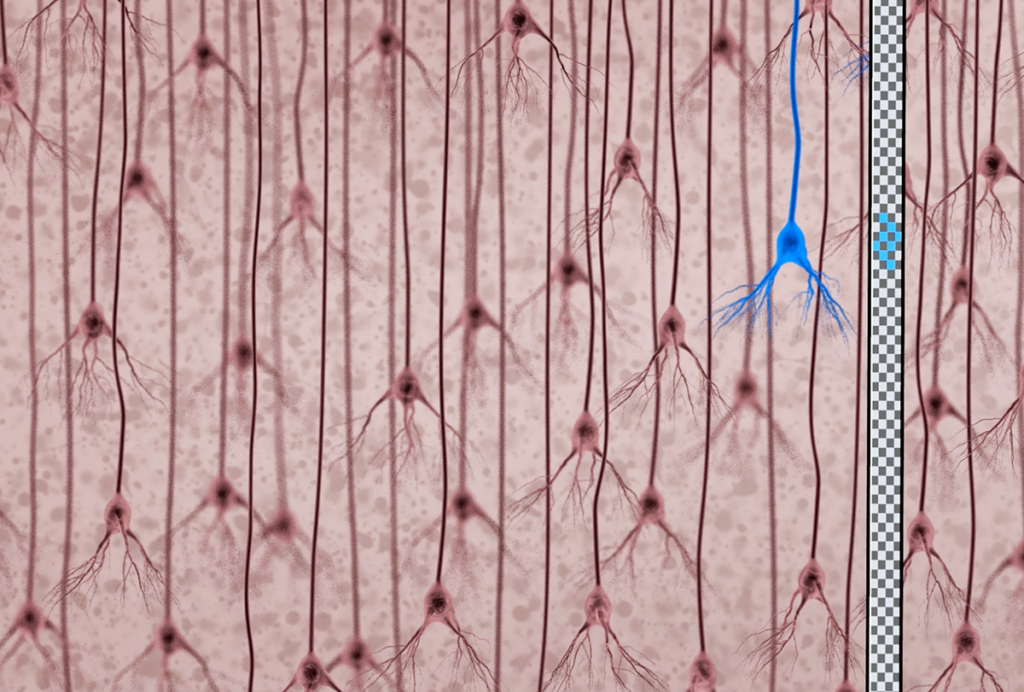
These neurons mediate signaling by the chemical messenger gamma-aminobutyric acid (GABA), sending signals that shut down the activity of other neurons. The researchers looked in particular at the forebrain, which includes part of the cortex and the hippocampus and regulates higher-order functions such as speech and emotion.
The study adds to a growing body of evidence that links both Rett syndrome and autism to GABA signaling. Deleting MeCP2 in forebrain neurons that release excitatory signals has only mild effects on the mice.
“We think it’s these GABAergic interneurons that are very critical to regulating the balance of activity in the brain,” says lead researcher Zhaolan Zhou, assistant professor of genetics at the University of Pennsylvania. “If you can therapeutically target this particular class of interneurons, maybe that can help us to narrow down treatments.”
Rett syndrome predominantly affects girls and results from mutations that inactivate the MeCP2 gene. Girls with the syndrome begin to lose their language and motor skills starting at about 1 year of age. They also show symptoms of autism and have breathing problems and frequent seizures.
In a 2010 study, researchers deleted MeCP2 from GABA neurons throughout mouse brains. These mice show most of the symptoms of the full disorder, including breathing problems, motor difficulties and social deficits, the researchers reported then in Nature2. The mice also die young.
In another set of mice, the researchers removed the gene from GABA neurons in the forebrain. These mice have problems with their motor and social skills, but breathe normally and live as long as controls do.
Hearing blips:
In the new study, Zhou and his colleagues tested the effects of deleting MeCP2 from various subsets of neurons in the brain, essentially conducting a ‘genetic dissection’ to test the role of different brain circuits in Rett syndrome.
The researchers used a noninvasive technique called electroencephalography (EEG), which measures neuronal activity. They found that mice that lack MeCP2 only in GABA neurons in the forebrain have problems with motor and social skills. The mice also show a weak, delayed brain response to blips of white noise broadcast in their cage, and suffer from frequent seizures.
By contrast, mice that express MeCP2 only in forebrain GABA neurons, but not in other cells in the forebrain, are sluggish but respond normally to sound. (These mice still have MeCP2 in cells in other brain regions.) Taking this setup even further, mice that express MeCP2 only in forebrain GABA neurons but not anywhere else in the brain have motor and social deficits and die young.
Intriguingly, however, these mice respond normally to sound and do not have seizures.
Together, these results suggest that GABA neurons in the forebrain play an important role in Rett syndrome, says Stephen Shea, assistant professor at Cold Spring Harbor Laboratory in New York, who was not involved in the study.
“This kind of dissection strategy is really important for pulling apart the pieces of really complex disorders like Rett syndrome,” he says.
The results also suggest that disrupting inhibitory neural circuits may tip the balance in the brain toward excitability, perhaps explaining the seizures associated with the disorder.
Abnormal sound responses detected using EEG may serve as a biological marker for Rett syndrome, says Zhou. Rett syndrome and autism are both associated with delays in sound processing.
In the new study, the researchers detected the delayed response to sound in neurons of the hippocampus, which processes sensory information. Neurons in the auditory cortex seem to respond normally, indicating that the mice’s hearing is intact.
This suggests that their neurons each have subtle glitches in sound processing, which accumulate between the auditory cortex and the hippocampus, says Michael Kilgard, professor of neuroscience at the University of Texas at Dallas, who was not involved in the study.
“I would interpret this as death by a thousand cuts,” he says. “Every synapse is adding a little bit of noise, and the higher up you go, you get the consequences.”
Studies have also suggested an important role for glia, or ‘support’ cells, in Rett syndrome. For example, a 2012 study notably found that a bone marrow transplant that restores one type of glia, called microglia, alleviates the breathing difficulties in Rett syndrome mice and lengthens their lifespan.
The new study, however, found that mice lacking MeCP2 in glia in the forebrain are normal. These mice still express MeCP2 elsewhere in the brain, which may allow the mice to breathe normally, notes Zhou.
The fact that mice with MeCP2 in only the forebrain GABA neurons still die young is interesting because its supports the theory that glia are critical in Rett syndrome, says Jonathan Kipnis, professor of neuroscience at the University of Virginia, who was the lead researcher on the bone marrow study.
“Either the forebrain is really not all that important for survival,” he says, “or maybe the rescue of GABAergic neurons is not enough and glia are indispensable in this disease.”
References:
Recommended reading
Documenting decades of autism prevalence; and more

Expediting clinical trials for profound autism: Q&A with Matthew State
Explore more from The Transmitter
‘Perturb and record’ optogenetics probe aims precision spotlight at brain structures