Neurons made from stem cells reveal cellular flaws in autism
Researchers have uncovered cellular abnormalities in Timothy syndrome by regenerating neurons from individuals with the rare autism-related disorder, according to a study published 27 November in Nature Medicine.
Researchers have uncovered cellular abnormalities in Timothy syndrome by regenerating neurons from individuals with the rare autism-related disorder, according to a study published 27 November in Nature Medicine1.
Using a mix of chemicals in a dish, the researchers reprogrammed skin cells from individuals with Timothy syndrome into so-called induced pluripotent stem (iPS) cells and then coaxed these cells to differentiate into neural precursor cells and neurons.
The cells derived from individuals with Timothy syndrome show a host of defects, including abnormal calcium signaling and low numbers of cells that can form long-range connections. Notably, Timothy neurons produce more catecholamines, a class of chemical messengers, compared with neurons reprogrammed from healthy individuals. These chemicals have been linked to autism and, more often, to bipolar disorder and depression.
This chemical excess is largely reversed when researchers expose the cells to a drug called roscovitine, which blocks the flow of calcium across the cell membrane.
The Timothy syndrome gene, CACNA1C, makes a protein needed for a certain type of calcium channel. Mutations in the gene, reported in only a few dozen people, cause heart defects, physical malformations and, usually, autism.
Using the iPS cell approach with rare forms of autism, “you can find things that are interesting potential clinical leads,” says lead investigator Ricardo Dolmetsch, assistant professor of neurobiology at Stanford University in Palo Alto, California. “In a way, it gives you a better preclinical model than we’ve had before.”
Suggestive signatures:
In the past year, researchers have created iPS-cell-derived neurons from individuals with Rett and fragile X syndromes, two autism-related disorders, and those with schizophrenia.
The new study “is probably one of the top papers in the field,” says Alysson Muotri, assistant professor of pediatrics at the University of California, San Diego, who led the Rett study.
The new work used skin samples from two children with Timothy syndrome and four healthy controls and created dozens of neuronal cell lines. This allowed the researchers to account for differences among individuals and among cells from the same individual.
By analyzing specific genetic markers, the researchers found that the iPS cell cultures include a mix of cell types. After 45 days of differentiation, about 65 percent of the cells are neurons. Of these, about 85 percent express markers for the lower layers of the cortex, and the rest for the upper layers.
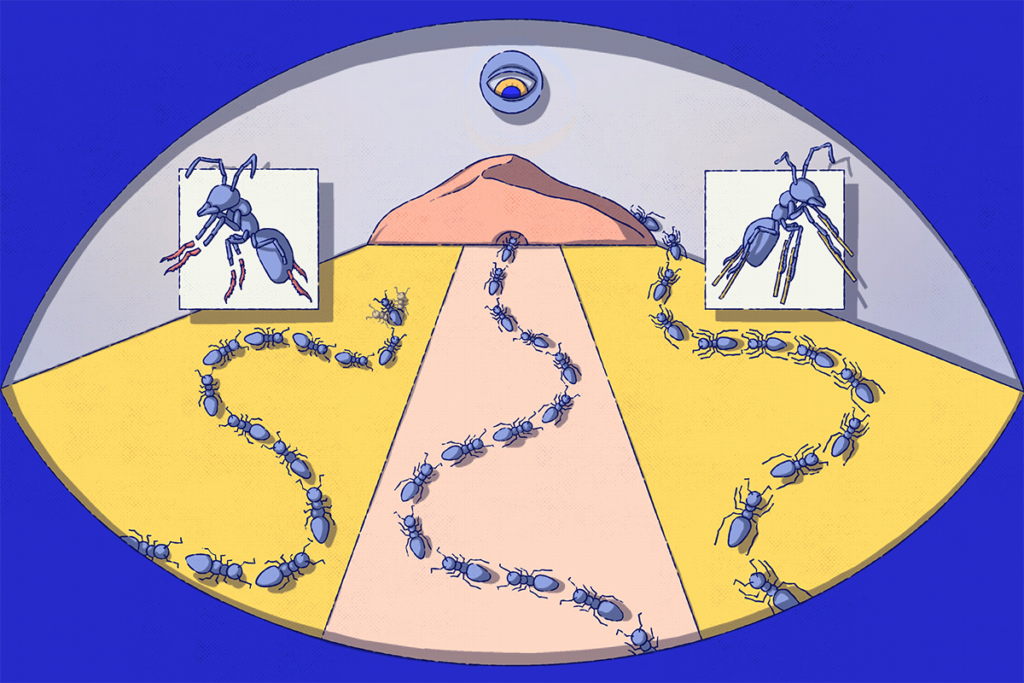
Compared with controls, the mix of cells that derive from the Timothy iPS cells have too few of the neurons destined to form the corpus callosum, the large bundle of fibers that connects the brain’s two hemispheres. Defects in this neural bridge have been associated with impaired social judgments and autism.
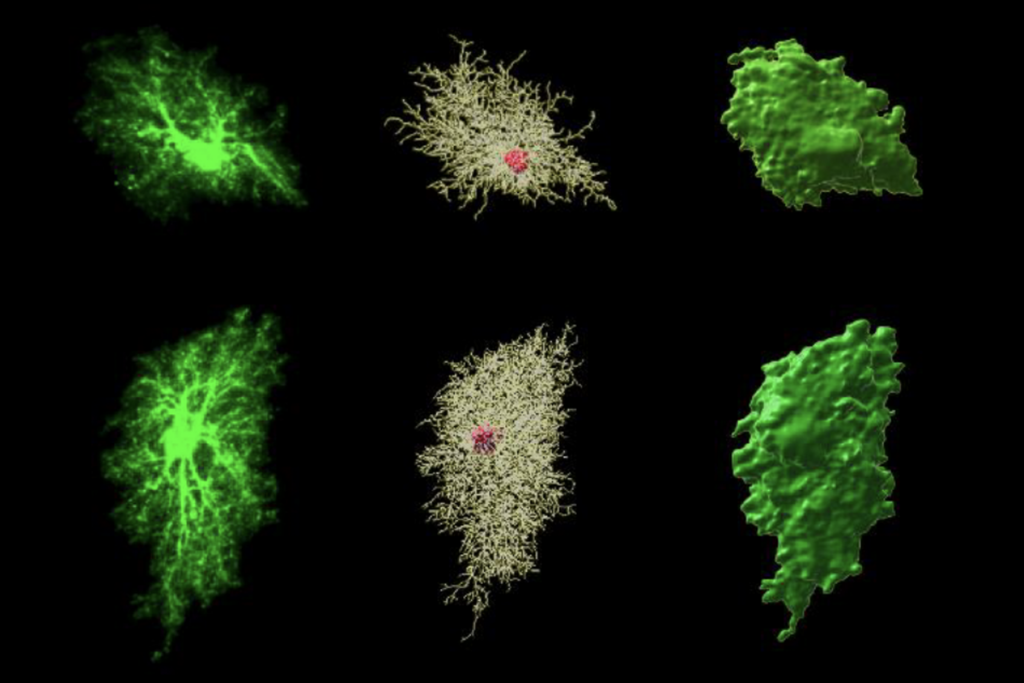
Timothy neurons also have shorter dendrites, the skinny branches that receive electrical signals, than control cells do, according to unpublished work from Dolmetsch’s lab.
But the most unexpected abnormality is the difference in catecholamine chemical messengers. Compared with controls, Timothy syndrome neurons make four times as much norepinephrine, which is important for stress response, and twice as much dopamine, known to be involved in reward, movement and mood.
The most valuable aspect of the new work, according to Muotri, is that some abnormalities seen in the Timothy neurons, including the catecholamine surge, do not show up in mouse models of the syndrome.
“Cells in a dish cannot represent the entire brain, because in the brain there are lots of compensatory networks that you don’t have in a culture dish,” Muotri says. “But you can still take advantage of the cell model to learn something new. It could be offering you a therapeutic opportunity that otherwise you wouldn’t have.”
Other researchers say, however, that features seen only in iPS cell lines may be less meaningful, because it’s unclear which precise brain region or regions the cells are modeling.
“It’s a very interesting paper, and I’m convinced that some of the abnormalities that they mimic, especially if they’re the same in mice that have the mutation, are true,” says Flora Vaccarino, professor of child psychiatry and neurobiology at Yale University.
Vaccarino’s group is creating iPS cell lines from hundreds of children with autism and unaffected family members included in the Simons Simplex Collection, a repository of genetic and clinical data from families that have only one child with autism and unaffected parents and siblings, led by SFARI.org’s parent organization.
Cellular defects that don’t show up in mouse models of the disorder, however, could be unique to the iPS cell approach, rather than true features of the disorder in people, Vaccarino says.
One way to find out, she says, would be to compare the RNA transcripts made by the cells to those in postmortem brain tissue from individuals with autism.
Common threads:
As the iPS cell technique gains popularity, researchers are beginning to compare cellular features of different forms of autism.
The new study, for example, found that the catecholamine increase is not present in neurons created from skin cells of individuals with Phelan-McDermid syndrome, another autism-related disorder.
But some of the other cellular defects may be shared by several autism disorders. For example, short dendrites are also seen in neurons from people with Rett syndrome, Muotri says. Preliminary work on postmortem brain tissue from individuals with autism has also shown abnormally short and dense spines, the stubby ends of dendrites.
“All of these forms of autism may have some overlapping molecular and cellular phenotypes in cells,” Muotri says. “As soon as we have more models in a dish, we’ll be able to figure out what’s common and what’s unique about specific diseases.”
Dolmetsch’s team has also made neurons from individuals with three other rare forms of autism: DiGeorge syndrome, Dravet syndrome and deletions of chromosomal region 16p11.2. Dolmetsch plans to dramatically expand this collection so that it includes a wide variety of autism cases with both known and unknown causes.
“I don’t think that there is going to be a common signature for all autism, but on the other hand, I don’t think we’ll find 800 different classes of autism,” Dolmetsch says.
The iPS cell approach is growing rapidly, he notes, and getting cheaper: The cost has dropped from $10,000 per cell line a few years ago to about $1,200 today. He predicts that clinicians will use information from iPS-cell-derived neurons to help guide treatment of children with unknown causes of autism.
“That’s absolutely the future,” Dolmetsch says. “It’s going to give us a biological diagnostic that allows you to group somebody into a specific class, and make predictions about whether certain drugs will work.”
References:
1: Paşca S.P. et al. Nat Med. Epub ahead of print (2011) PubMed
Recommended reading
Explore more from The Transmitter

Computational psychiatry needs systems neuroscience
This paper changed my life: John Tuthill reflects on the subjectivity of selfhood