Mouse studies support second chance for fragile X drug
Two new studies give a boost to arbaclofen, which failed to meet expectations in clinical trials for autism and fragile X syndrome.
Three years ago, arbaclofen was the most promising drug for the autism-linked disorder fragile X syndrome. But after two cancelled clinical trials, it fell victim to the vagaries of the drug development pipeline. Two new studies in mice hint that this early end to its story may have been premature.
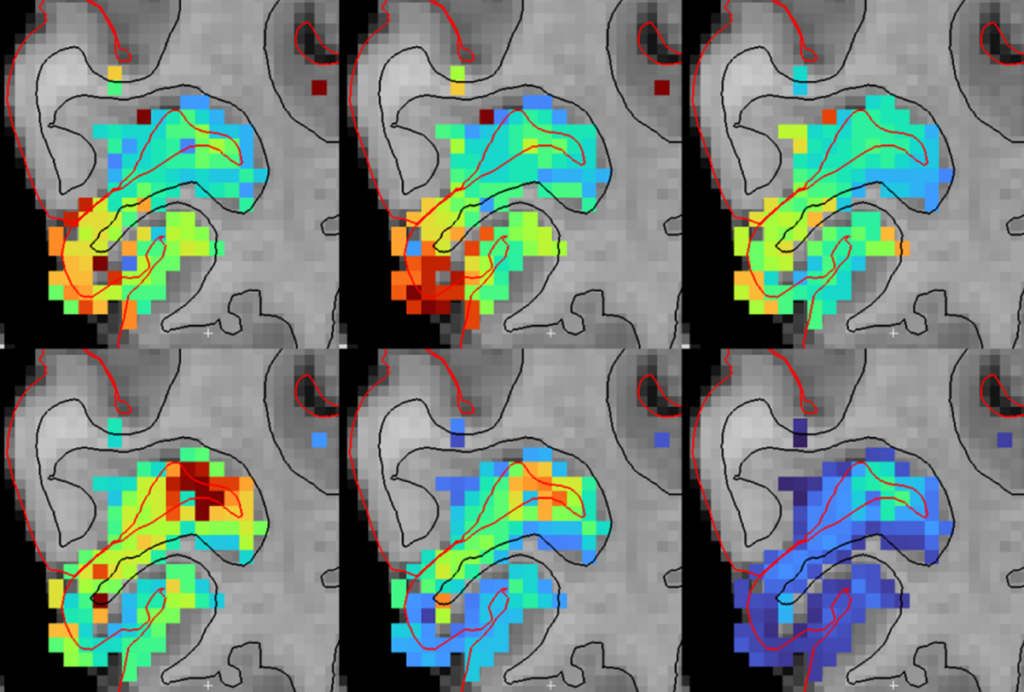
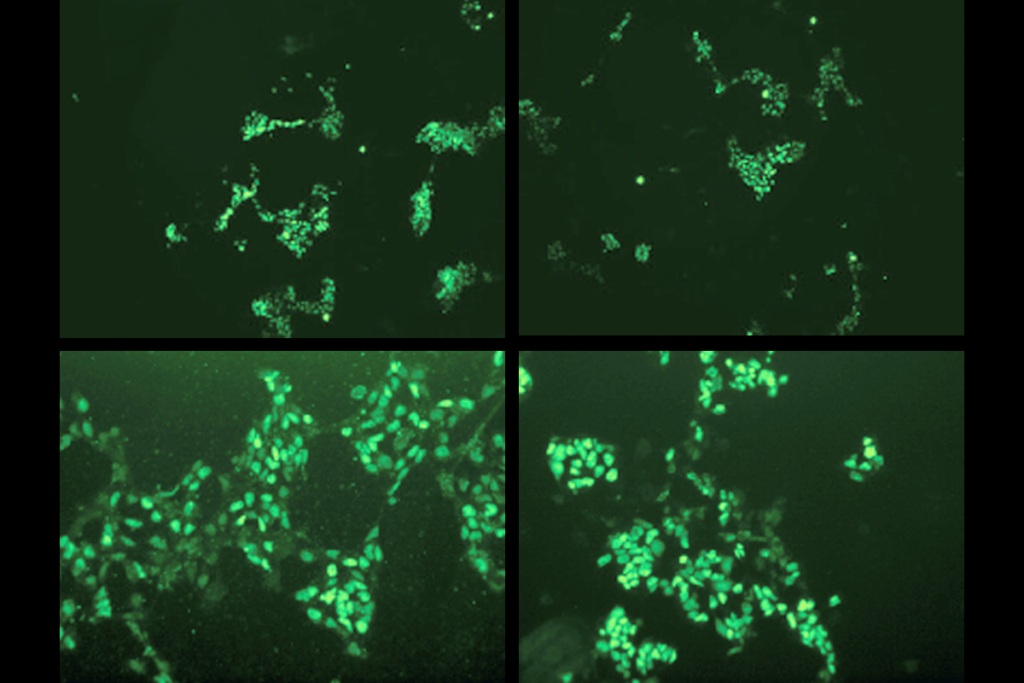
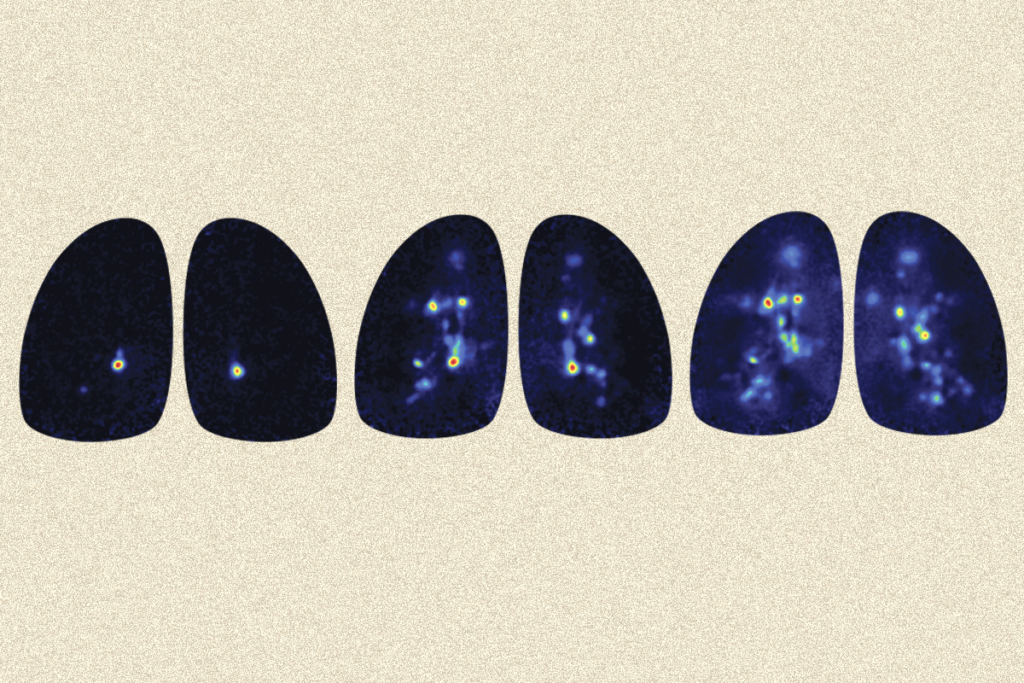
One study, published 28 March in the International Journal of Neuropsychopharmacology, showed that arbaclofen corrects abnormalities in the fragile X brain. It revealed that the drug dampens protein synthesis, which runs amok in fragile X syndrome.
The study also found that neurons in mice may ramp up production of certain proteins to compensate for the drug’s effects. This adaptation may help to explain why arbaclofen failed to significantly improve social skills in adolescents and adults with fragile X syndrome.
Another study, published last month in Neuropsychopharmacology, determined that arbaclofen eases social deficits as well as obsessive and repetitive behaviors in mice with features of autism.
Together, the findings from these studies suggest that the drug can achieve real benefit in easing the symptoms of fragile X syndrome and, perhaps, autism.
Arbaclofen stimulates inhibitory receptors known as GABA-B, an action that ultimately dampens brain activity. Mice that model fragile X syndrome have fewer GABA-B receptors. A 2012 study showed that stimulating the activity of the receptors with arbaclofen helps correct neuronal signaling in the mice and alleviates their repetitive behaviors.
These findings prompted a clinical trial that same year by Seaside Therapeutics, a Massachusetts-based biotechnology firm, in which the drug improved social behavior in children and adults with fragile X syndrome.
Encouraged by this outcome, Seaside extended its trial in people with fragile X syndrome and launched another one in children with autism.
In both trials, there were anecdotal reports that children improved in their ability to communicate and carry out daily tasks. However, the trials were designed primarily to measure social behavior, which did not improve enough to pass the requirements for drug approval. Seaside halted the trials and subsequently went under.
Since then, the Simons Foundation Autism Research Initiative — funded by the Simons Foundation, SFARI.org’s parent organization — has purchased the rights to arbaclofen and plans to revive trials in people with autism to verify the reported benefits. But there’s no question that the field lost valuable time.
The saga serves as a lesson on the importance of carefully designing clinical trials to capture all of a drug’s positive effects. The latest studies in animals are proof that there’s more to arbaclofen’s effects on the brain than the aborted trials had the time to find.
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome
Changes in autism scores across childhood differ between girls and boys
Explore more from The Transmitter
Smell studies often use unnaturally high odor concentrations, analysis reveals
‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt