Mouse model hints at Alzheimer’s therapies for fragile X
Lowering the levels of proteins associated with Alzheimer’s disease can improve symptoms of fragile X syndrome in mice, according to a poster presented Wednesday at the Society for Neuroscience annual meeting in San Diego.

Beta blockers: Targeting beta-amyloid, the molecule that forms plaques in Alzheimer’s disease, may also help people with fragile X syndrome.
Lowering the levels of proteins associated with Alzheimer’s disease can improve symptoms of fragile X syndrome in mice, according to a poster presented Wednesday at the Society for Neuroscience annual meeting.
Fragile X syndrome is the most common inherited cause of cognitive disability, and the most common known cause of autism. It is caused by a mutation in the FMR1 gene, which encodes FMRP, a regulatory protein.
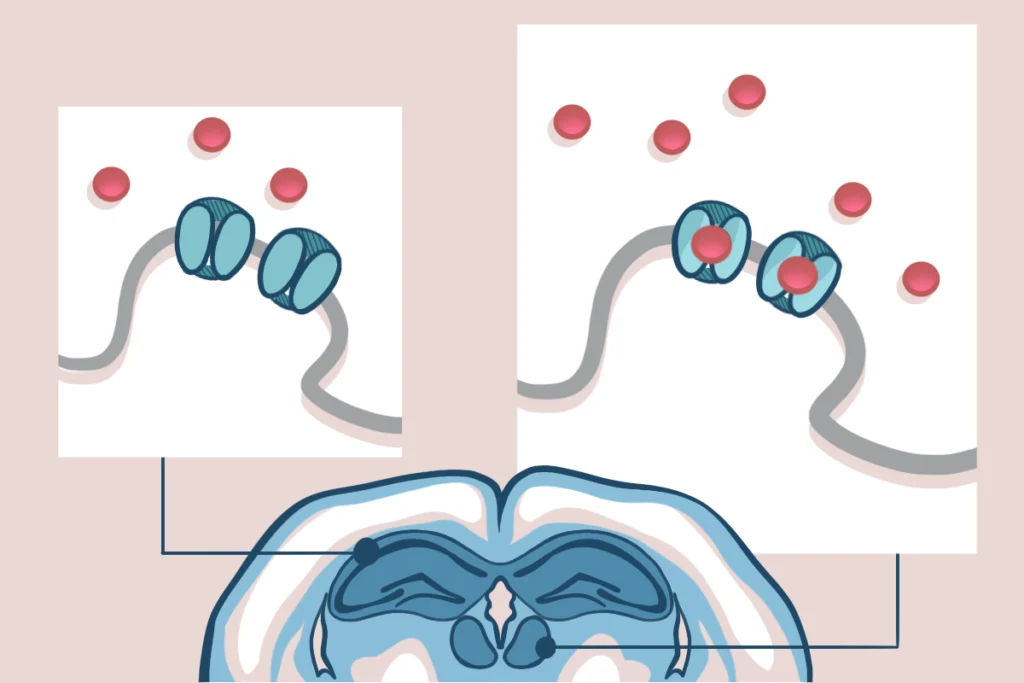
One of FMRP’s targets is amyloid precursor protein, or APP. In turn, APP can be processed by the body to form beta-amyloid, the molecule that forms plaques in the brains of people with Alzheimer’s disease.
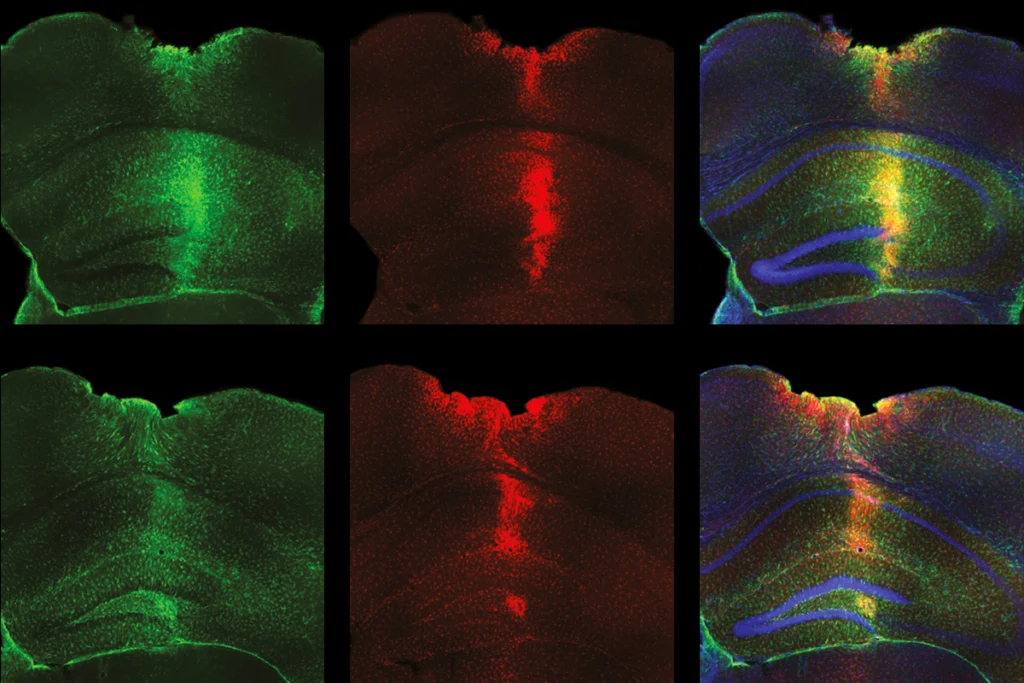
“Our previous work has shown that amyloid precursor protein and beta-amyloid are increased in FMR1 knockout mice,” says study leader Cara Westmark, associate scientist in pathology and laboratory medicine at the University of Wisconsin-Madison.
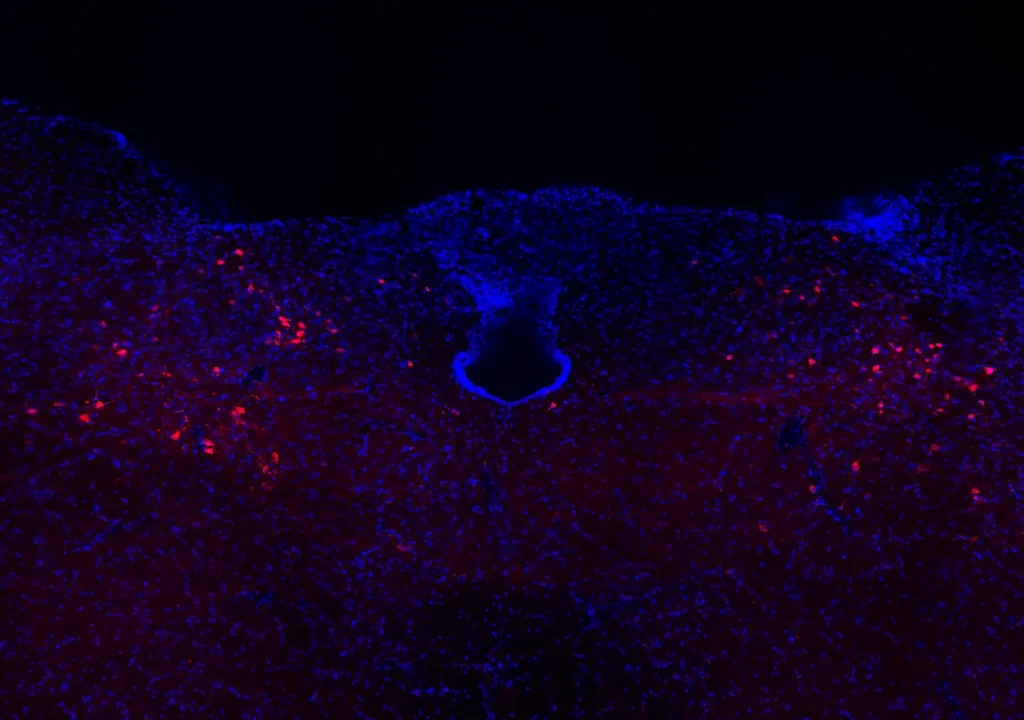
These mice lack the fragile X protein and recapitulate symptoms of the disorder, including anxiety, seizures in response to certain sounds, and abnormal dendritic spines — the parts of nerve cells that receive chemical signals from other nerve cells.
In the new study, Westmark’s team found that decreasing the levels of APP and beta-amyloid in these mutant mice diminishes or even eliminates their fragile X-related symptoms.
In one group of fragile X mice, the researchers inactivated one copy of the APP gene. These mice produce less APP than normal, and their fragile X symptoms partially or completely disappear.
As another way of decreasing beta-amyloid in the brain, the researchers injected a second group of fragile X mice with an antibody to the molecule. This treatment stops the characteristic seizures in response to sound that occur in fragile X mice.
It’s not yet certain whether people with fragile X syndrome also have higher levels of APP and beta-amyloid in the brain. Few postmortem brains from people with the disorder are available to study, Westmark says — but she has examined four of them, and found higher levels of beta-amyloid.
“It’s quite an insight to see that the fragile X protein regulates synthesis of amyloid precursor protein,” says William Ted Brown, director of the Institute for Basic Research in Developmental Disabilities in New York, who was not involved with the work. “I think it’s quite exciting work.”
Earlier this year, a study suggested connections between fragile X and presenilin, a gene linked to early-onset Alzheimer’s disease. Westmark says cross-pollination between Alzheimer’s and fragile X research could be fruitful in both directions. “The two disorders could be related, and therapies helpful for one could also be helpful for the other,” she suggests.
For more reports from the 2010 Society for Neuroscience meeting, please click here.
Recommended reading

In updated U.S. autism bill, Congress calls for funding boost, expanded scope
X-chromosome genes; neurobiology of infant crying; MCHAT in preemies

Task swap prompts data do-over for autism auditory perception study
Explore more from The Transmitter
Cell population in brainstem coordinates cough, new study shows
Ketamine targets lateral habenula, setting off cascade of antidepressant effects