Most autistic people — 87 percent, according to the latest estimate — have some sort of motor difficulty, ranging from an atypical gait to problems with handwriting1. These issues are distinct from the repetitive behaviors considered to be a hallmark of autism. And yet, despite their prevalence, motor problems are not considered a core trait of autism, because they also occur with other conditions, such as Down syndrome, cerebral palsy and attention deficit hyperactivity disorder.
Here, we describe what experts know about the causes, characteristics and consequences of motor difficulties, which they say are among the least understood and most neglected aspects of autism. They also call on researchers to better assess motor difficulties in autistic people and for clinicians to treat these problems, especially because motor setbacks may have consequences far beyond simply impeding movement.
What types of motor issues do autistic people have?
They may have gross-motor problems, such as a clumsy, uncoordinated gait; and difficulties with fine-motor control, such as manipulating objects and writing. Some may have trouble coordinating movements between the left and right side of the body among different limbs, making it difficult to do actions like pumping their legs on a swing, jumping, skipping or hopping. Others may have low muscle tone and problems maintaining their posture or balance. Still others seem to have trouble with actions requiring hand-eye coordination, such as catching a ball or imitating the movements of others, and with planning a series of movements or gestures, known as praxis. These difficulties can range from mild to severe and can impact any motor system of the body2.
At what age do motor issues start?
They can appear in infancy. For instance, 1-month-old infants who are later diagnosed with autism tend to move their arms less than typical infants do3. By about 4 months of age, a typical child can keep her head in line with her shoulders when pulled up into a sitting position, but a baby with autism often lacks that strength, and her head will flop back4. And at 14 months — an age when most typical children are able to walk — autistic children may still be unable to stand. Other motor issues can include struggling to grasp objects or sit up, and not clapping and pointing2,5.
How are motor problems linked to genetic factors that influence autism?
Some mutations that predispose people to autism may also contribute to motor issues. For example, every one-month delay in beginning to walk increases a child’s odds of having a spontaneous mutation in an autism gene by 17 percent, according to a 2017 study6. And some ‘syndromic’ forms of autism — those that have a single genetic cause — include particular motor issues among their defining characteristics: People with Phelan-McDermid syndrome often have low muscle tone, and children with dup15q syndrome tend to have a characteristic gait.
Although motor issues tend to be most severe in autistic people who have intellectual disability, they can affect anyone on the spectrum. For example, people with autism who carry spontaneous mutations have an increased likelihood of motor problems, regardless of whether they have intellectual disability, according to a 2018 study. Other studies have found that children on the spectrum have more motor issues than do typical controls who are matched for intelligence quotient7. Some researchers say that particular motor issues may help distinguish syndromic forms of autism from non-syndromic autism, but this idea remains unproven.
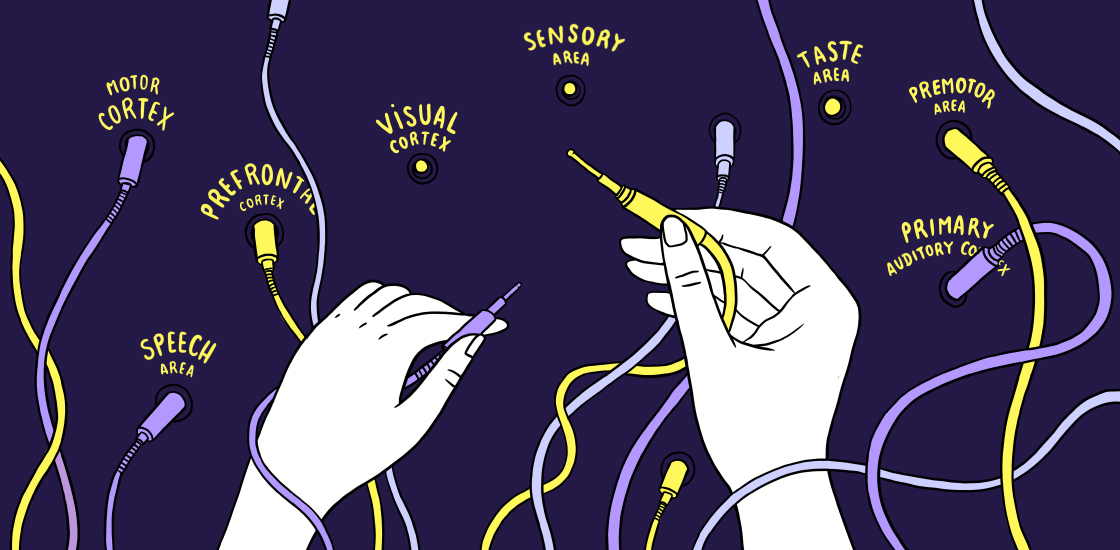
What could be going on in the brain?
Differences in connectivity between brain regions could help explain some autistic people’s motor difficulties. For instance, children with autism have decreased synchrony in the activity between their visual and motor regions; the less synchronization there, the more severe their social deficits, based on a standard scale. Their motor issues may also stem from less connectivity between the inferior parietal lobe, a region involved in hand-eye coordination; and the cerebellum, which helps guide and correct movements8. Other evidence implicates weak connections between sensory and motor regions and atypical activity in a network important for motor planning9.
People with autism also seem to discount visual information and rely more on proprioception, or their internal sense of their body’s position, than typical people do when learning to use a new tool. The more that people with autism rely on proprioception, the more severe their social deficits, although researchers are not yet sure why this is the case.
Can motor issues contribute to autism traits?
Perhaps. Motor issues in infancy have been tied to delays in babbling, gesturing and acquiring new vocabulary, and they may have other ‘cascading effects’ on cognitive, social and emotional development10. That is because motor abilities, such as sitting up, reaching for objects and walking, give babies access to new experiences that prompt learning. Also, babies who do not move much or cannot grasp objects tend not to elicit interactions from their caregivers, thereby limiting opportunities to learn language and other skills from adults.
Poor motor skills later in childhood may make autistic children reluctant to engage in physical activities such as sports, limiting their opportunities to interact with other children and potentially hampering social development. In a more subtle way, having trouble coordinating head movements could make it difficult to follow social interactions in a large group, and trouble with handwriting could affect academic performance.
The visual-motor integration skills that autistic people struggle with the most are also crucial to imitating and learning from others and participating in social interactions.
Although motor issues undoubtedly hamper social and cognitive development, it’s unlikely that they are the sole cause of social difficulties, some researchers say. Instead, motor and social differences in people with autism may have the same root cause in the brain, they say.
How do doctors and researchers measure motor skills?
A few standardized tests can reveal whether a child can do certain motor tasks. But these are not precise enough to capture and measure the motor impairments of children with autism. Also, the tasks, which were designed for typical children, may be difficult or impossible for children with intellectual disability or cognitive impairment.
Some researchers have been devising new ways to probe motor issues, using handwriting, virtual reality, motion capture with sensors and infrared cameras, accelerometers and gyroscopes (to measure the intensity and angle in limb movements), mats equipped with pressure sensors (to detect differences in gait), and electromyography (a technique that measures the electrical activity of muscles). But researchers say they are still a long way off from standardizing these measures. Finding measures that capture autistic people’s motor differences is the first step.
How are motor problems treated?
The standard treatments typically include physical and occupational therapy, but these may not fully address autistic children’s needs, researchers say. What’s more, only 32 percent of children with autism get treatment for their motor issues1. Some experts have begun trying out new treatments, such as adapted sports programs, yoga, martial arts and movement therapies involving music, although there is little evidence yet whether any of these approaches are effective.