Mighty element plays major part in autism
Probing the function of a protein in a calcium signaling pathway may lead to a diagnostic test for autism and a path toward treatments.
Calcium is important for bones and teeth, that much is well known. Less well known is its role in brain activity.
Movement of calcium ions across cell membranes is an important mechanism by which cells communicate. And in a series of studies, we have shown that this plays an underappreciated and not yet fully understood role in autism.
We came upon this discovery by taking a novel view of certain genes and proteins implicated in autism. Rapid advances in genome sequencing over the past decade have offered a glimpse into the genetic architecture of the condition, flagging hundreds of putative autism genes. These genes work together in a small number of networks, or signaling pathways.
One of these pathways is often called ‘synaptic,’ because the genes in it seemed to operate at synapses, or neuronal junctions. We noticed something else about these genes: Many of them work to regulate and respond to calcium movement.
The idea that calcium signaling plays a role in autism and related conditions is not foreign to the field: The autism-related disorder Timothy syndrome is caused by a mutation in a calcium-channel gene.
But upon detailed study of the function of the calcium pathway, we could resolve a specific component of calcium signaling that stands out as important in autism: the inositol trisphosphate (IP3) receptor. Our studies suggest that testing this protein in action may greatly aid autism diagnosis and pave a path toward personalized treatments.
Calcium bank:
We started studying the components of the calcium pathway several years ago. We thought it might represent a node at which many of the diverse genetic and environmental factors involved in autism converge1,2. In 2013, we began examining calcium signaling in human skin cells, which are easy to obtain and have the same intracellular organelles as brain cells do.
We first analyzed skin cells from people with fragile X syndrome or tuberous sclerosis type 1 or 2 — autism-related conditions, each caused by mutations in a different single gene. Using sophisticated biophysical techniques, we functionally dissected components of calcium signaling in these cells.
We found that the one mediated by IP3 receptors is functionally altered in the same fashion in all three cell types.
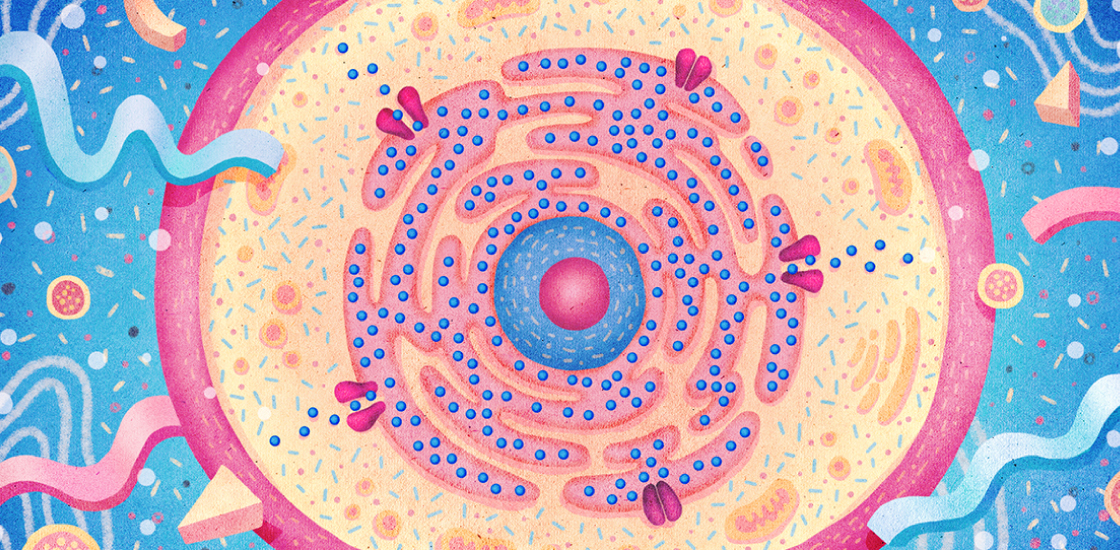
The IP3 receptor is a channel that releases calcium from the endoplasmic reticulum (ER), an organelle found inside virtually all cells of the body. The ER acts as a ‘calcium bank.’ It is involved in the release of calcium in response to a wide range of stimuli, including hormones, growth factors, neurotransmitters and other molecules that govern communication between neurons.
The IP3 receptor is not mutated in either fragile X syndrome or tuberous sclerosis. Yet we observed that intracellular calcium signaling by this receptor is significantly lower in the fragile X and tuberous sclerosis cells than in cells from neurotypical individuals3.
Distinct difficulties:
We applied an ‘optical patch clamp’ technique to visualize this channel in action in cells from individuals with fragile X syndrome and tuberous sclerosis. The method, developed by one of our colleagues, Ian Parker at the University of California, Irvine, involves a high-resolution fluorescence microscope and calcium-sensitive dyes4. The technique allows us to watch the miniscule calcium currents flow while this channel protein changes shape as it opens and closes.
We found that the channel opens just as rapidly in these cells as in controls, and calcium flows at an equivalent speed. But the channel in these cells stays open for a mere 15 milliseconds, half as long as in controls, before snapping shut3.
These molecular changes result in a drastically lowered amount of calcium being released from the ER. In neurons, a predictable consequence of this would be decreased secretion of neurotransmitters into synapses and changes in calcium-activated gene expression.
We next developed a high-throughput screen for this functional change in the channel. We used it to screen 27 people with autism enrolled in the Center for Autism Research and Translation at the University of California, Irvine. We were surprised to find that the vast majority of people in this heterogeneous group have the calcium-signaling deficit5.
The assay could serve as a biomarker that distinguishes between cells from people with autism, fragile X or related syndromes and cells from controls.
Diagnostic odyssey:
Not surprisingly, a small number of people with autism do not have this signaling deficit. So people with autism could be stratified into subtypes based on the amount of calcium released from IP3 channels. Neurotypical individuals are all ‘high signalers,’ but people with autism are likely to be ‘low’ or ‘very low’ signalers.
Each subtype might show distinct constellations of medical issues, such as seizures, gastrointestinal distress or immune deficiencies. The groups also might respond differently to treatments, potentially aiding drug discovery.
Many families go through a tragic diagnostic odyssey before finding out their child has autism. Our high-throughput test could identify at an early age children who are at risk for autism. The assay might also be used to screen novel small-molecule drugs that reverse the signaling deficit.
The IP3 receptor’s aberrant function may also explain why many people with autism experience problems that do not involve the brain. These channels are expressed throughout the body, so glitches in their signaling could disrupt various bodily systems — including the immune system and the gut.
John Jay Gargus is director of the Center for Autism Research and Translation at the University of California, Irvine. Galina Schmunk is a postdoctoral researcher in his lab.
References:
Recommended reading

Expediting clinical trials for profound autism: Q&A with Matthew State

Too much or too little brain synchrony may underlie autism subtypes
Explore more from The Transmitter

This paper changed my life: Shane Liddelow on two papers that upended astrocyte research
Dean Buonomano explores the concept of time in neuroscience and physics

