Maternal infection exacerbates genes’ effect on autism
Children with too many or too few copies of certain genes are more likely to have autism, as are children born to women who battled a severe infection while pregnant. These seemingly disparate risk factors may work together to worsen autism symptoms.
Children with too many or too few copies of certain genes are more likely to have autism, as are children born to women who battled a severe infection while pregnant. These seemingly disparate risk factors work together to worsen autism symptoms, suggests a new study1.
The study, published 27 January in the Journal of Developmental and Behavioral Pediatrics, is one of the first to look at the combined effects of genetic and environmental risk factors for autism.
“The interactions between genetics and exposure in the intrauterine environment sort of bump up the symptoms,” says lead researcher Raphael Bernier, associate professor of psychiatry and behavioral science at the University of Washington in Seattle.
Epidemiological studies indicate that having a serious infection while pregnant raises the risk of having a child with autism. Animal studies support this theory, showing that mimicking infection during pregnancy in rodents and monkeys can alter social behavior in their young2, 3. But only a small proportion of women who have infections during pregnancy have children with autism, suggesting that genetic factors are also at play.
Bernier and his colleagues sought to tease out these factors by looking closely at children with autism who have both risk factors: exposure to maternal infection, as well as at least one large duplication or deletion of DNA, known as a copy number variation, (CNV), linked to the disorder4.
They found that children with autism who have both risk factors have more severe symptoms, such as repetitive behaviors and social deficits, than children with autism who have only one or neither of the risk factors.
“Many studies suggest a role for both gene and environmental factors in autism risk,” says Elizabeth Thomas, associate professor of molecular and cellular neuroscience at The Scripps Research Institute in La Jolla, California, who was not involved in the study. “But to see real data supporting this hypothesis is exciting.”
Infection connection:
The finding comes on the heels of several epidemiological studies looking at maternal infection and autism risk. Last year, a study of more than 2 million people in Sweden found that having an infection during pregnancy raises the risk of having a child with autism by 37 percent5, and a 2012 study of nearly 100,000 Danish children found that a weeklong fever can triple the odds6.
To explore this further, the researchers looked at genetic data, detailed descriptions of autism symptoms and the mother’s history of infection or fever during pregnancy for 1,971 children with autism from the Simons Simplex Collection. (The collection contains data from families that have one child with autism and unaffected parents and siblings, and is funded by the Simons Foundation, SFARI.org’s parent organization.)
They found patterns showing how genes and environmental exposures can interact to affect specific facets of autism.
The parents filled out three assessments that evaluate patterns of repetitive behavior, social awareness, anxiety and social communication, among other measures. The children also took age-appropriate tests to assess verbal and nonverbal intelligence quotients (IQs) and adaptive functioning, a measure of how well they can handle day-to-day activities.
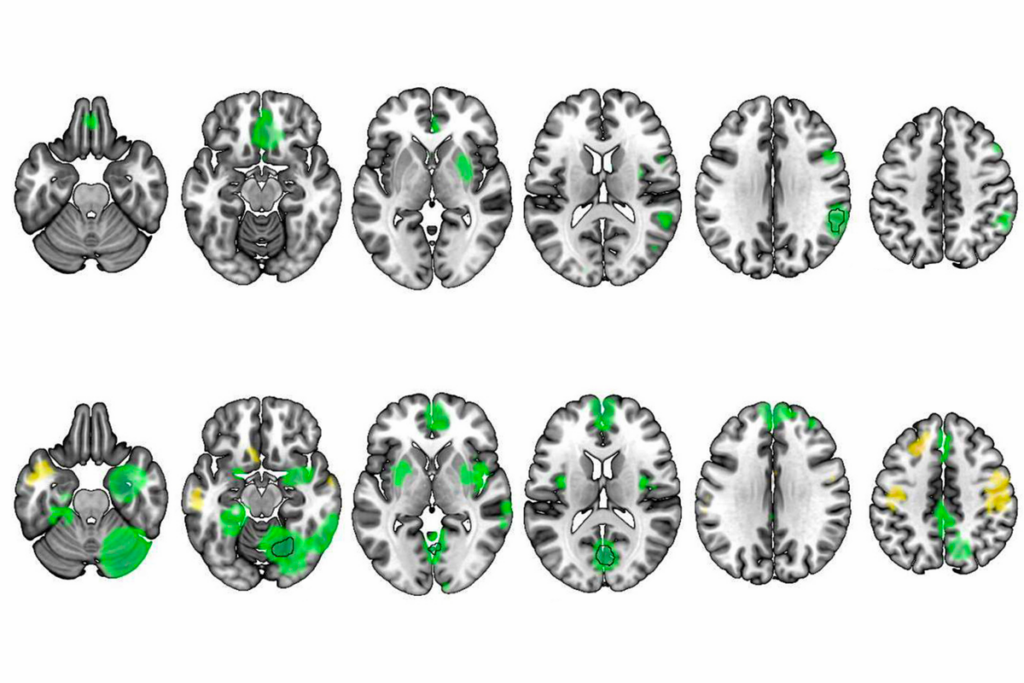
As expected, children with autism-associated CNVs score lower on measures of adaptive functioning and IQ. By contrast, children exposed to maternal infection but who don’t have any autism-linked CNVs show slightly more severe autism-related symptoms on one of the three tests. They also have no significant differences in cognitive ability compared with children who have neither risk factor.
The most significant effects emerge in children who have both risk factors: These children have more severe autism symptoms according to all three tests.
“We were surprised that the findings were specifically tied to autism symptomology and not just broader neurodevelopment,” says Bernier.
Access to the detailed genetic and clinical data allowed the researchers to parse the interaction of genetic and environmental risk factors in a way that previous epidemiological studies have not been able to do, says Brian Lee, assistant professor of epidemiology and biostatistics at Drexel University in Philadelphia, who was not involved in the study. “This is one of the few demonstrated examples in a human sample where [the gene-environment interaction] paradigm seems to be apparent,” says Lee.
These interactions may be involved in only a small proportion of autism cases. Of the 395 mothers who reported an infection or fever during pregnancy, 29 have children who carry an autism-linked CNV. This means only 1.5 percent of the 1,971 children in the study have both risk factors.
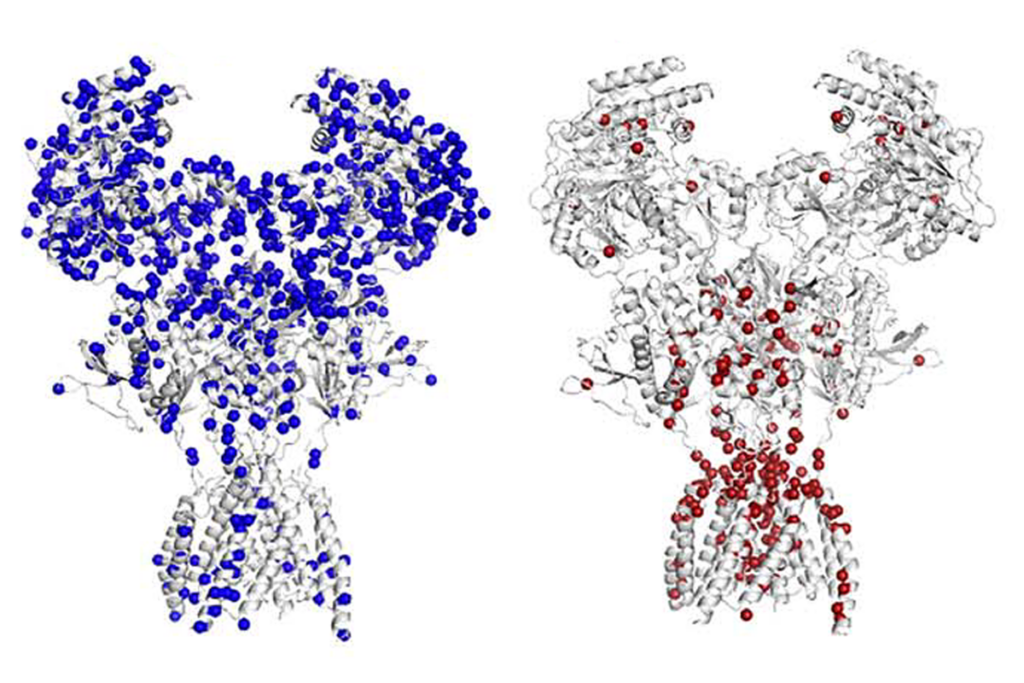
Researchers must explore exactly how exposure to maternal infection can affect genes in the developing brain. Several previous studies offer hints. For example, Thomas and her colleagues have shown that activating a pregnant mouse’s immune system produces inflammatory compounds in her pups. These compounds, called cytokines, can alter the expression of genes, including those involved in brain development and immune regulation7.
It’s possible that similar mechanisms are at work in people, says Alan S. Brown, professor of psychiatry and epidemiology at Columbia University, who was not involved in the study. Elevated levels of the cytokine interleukin-8 during pregnancy have been shown to alter the size of brain regions in people, for instance.
CNVs that affect immune-related genes might make some children more sensitive to their mother’s immune response. Alternatively, Brown says, “it is possible that the microbial infection, not the immune response, might alter brain development.”
In the meantime, Bernier’s team plans to look at the effect of maternal infection on children with a deletion in the chromosomal region 16p11.2 — one of the most common CNVs seen in people with autism. “This is the first foray,” Bernier says. “Both sides of the scale need to be further specified to get a clear answer.”
Correction: This article has been modified from the original. It has been changed to clarify that 1.5 percent of all the children in the study have both risk factors (a CNV and maternal infection).
References:
1. Mazina V. et al. J. Dev. Behav. Pediatr. 36, 61-67 (2015) PubMed
2. Schwartzer J.J. et al. Transl. Psychiatry 3, e240 (2013) PubMed
3. Machado C.J. et al. Biol. Psychiatry Epub ahead of print (2014) PubMed
4. Matsunami N. et al. PLoS One 8, e52239 (2013) PubMed
5. Lee B.K. et al. Brain Behav. Immun. 44, 100-105 (2015) PubMed
6. Atladóttir H.O. et al. Pediatrics 130, e1447-1454 (2012) PubMed
7. Tang B. et al. Brain Behav. Immun. 30, 168-175 (2013) PubMed
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys
Explore more from The Transmitter
BCL11A-related intellectual developmental disorder; intervention dosage; gray-matter volume
Grace Hwang and Joe Monaco discuss the future of NeuroAI