Magnetic promise: Can brain stimulation treat autism?
There are hints that transcranial magnetic stimulation, which uses electricity to change how brain cells function, might improve the symptoms of autism. But hopes are running way ahead of the facts.
W
ill Robeson bounces into the neuroscience lab at the University of Louisville in Kentucky, familiarly calling out to each staff member. He makes his way to a black leather recliner positioned next to a suitcase-sized piece of equipment, with controls and a power supply, that looks like it belongs in a dentist’s office. Above his head, a piece of plastic shaped like a figure eight contains a coil capable of generating a powerful magnetic field.
Will, a 12-year-old boy with autism, is about to undergo transcranial magnetic stimulation (TMS); the magnetic field will temporarily alter the electrical activity of his brain. He has done this more than 40 times in the past four years. The goal of the treatment is to retune the way his brain cells communicate, and help him connect to the world.
Over time, he and Estate Sokhadze, the scientist who expertly manipulates the machine, have established a comforting routine. Sokhadze first places electrodes on Will’s hands to measure the boy’s breathing and pulse. He then puts a dark blue swim cap over Will’s head, the better to see the outlines of the boy’s cranium. Picking up the coil as if it were a wand, Sokhadze holds it just above the left side of Will’s head, an inch behind where his red bangs peek out from under the cap. As the machine begins emitting loud clicks, Will closes his eyes and counts along with each click, “1, 2, 3, 4 — ” until he reaches 20 and the clicks stop.
After repeating the process several more times in the same spot, Sokhadze shifts the coil to the right side of Will’s head. The boy instructs his grandmother, who is standing nearby, to count with him this time: “ — 18, 19, 20.”
Although the procedure looks as if it could be overwhelming, Will says, “It feels happy.” And it seems that the regular treatments have gradually eased some of his autism symptoms.
When Will first came to the lab at age 8, he had a limited vocabulary. He flapped his arms repeatedly, and refused to ride in the building’s elevators. “For all practical purposes, he was in sort of a fog,” says his grandfather Tom Robeson, who, together with his wife Nancy, picks Will up from his parents’ home and takes him to the sessions, more than an hour’s drive away.
Initially, Will came in every week for 18 weeks as part of a study testing TMS as a treatment for autism in the lab of Manuel Casanova, then a neurologist at the University of Louisville, with whom Sokhadze collaborates. In the years since, Will has returned periodically for ‘booster’ sessions. According to clinical evaluations, the treatments have slightly alleviated Will’s hyperactivity and repetitive behaviors. Although he still cannot hold a meaningful conversation, his grandparents say he has become much more interested in other people and is better able to control his behavior at school.
“It calmed him,” says Tom Robeson. “I think the TMS did begin his journey into the real world.”
Signs of progress in a few people like Will have fostered hopes that TMS will become a routine therapy for autism — a disorder with no reliable biological treatments. Families desperate for help are understandably eager to see TMS more widely adopted, and that interest is likely to grow next year when John Elder Robison, a well-known speaker and writer who has autism, publishes a new memoir describing how TMS has transformed his life.
The problem, however, is that the evidence for TMS’ effectiveness is still thin.
“There’s tremendous excitement at the potential to have something that’s noninvasive, non-drug-based, with potentially fewer side effects,” says Michael Platt, a neurobiologist at the University of Pennsylvania in Philadelphia who is studying the effects of TMS in monkeys. “But the fact of the matter is we don’t understand very much about how it works.”
The small studies so far have mainly used TMS as a research tool, gathering data on symptoms as an aside, so they cannot prove that it works as a treatment. Of the studies that specifically assessed it as a therapy, only one meets the highest standards for research of this type. Overall, the results have been mixed: Some people with autism benefit; others do not.
Still, some for-profit clinics have already begun treating people who have autism with TMS, a practice researchers say isn’t yet justified. “It’s worrisome,” says Lindsay Oberman, an autism researcher at Bradley Hospital in Providence, Rhode Island, who has studied, among other things, how TMS changes neuronal connections in response to experience. “You could make somebody worse if you don’t know what you’re doing.” Others with autism are experimenting on their own, using electrical stimulation devices that don’t have the same effect as the ones used in the laboratory.
”“The fact of the matter is, we don’t understand very much about how it works.” University of Pennsylvania neurobiologist Michael Platt.
Electric possibility:
I
n ancient times, the Romans treated headaches and other pain by immersing themselves in pools replete with electric torpedo fish. In the late 1700s, Alessandro Volta channeled the electricity generated by his newly invented battery to his muscles, eyes and ears. By the 20th century, scientists had learned that neurons communicate via electrical signals. One result of that knowledge was electroconvulsive therapy, developed in 1938 to treat severe depression. And in 1985, scientists used the idea of electromagnetic induction, discovered in 1830 by English physicist Michael Faraday, to develop TMS as another method of stimulating the brain.
The basic premise is this: When a powerful magnet generates a magnetic field near the head, the field travels a few centimeters through the scalp and skull, changing the electrical activity of neurons in those locations. The result is a temporary reorganization in the way brain cells communicate with one another.
Unlike electroconvulsive therapy, in which electrodes are placed directly on the scalp in order to trigger a seizure, TMS can be targeted to one brain region, and allows for more precise alterations of brain function. It also seems to be gentler than the brutal images associated with the early years of electroconvulsive therapy: TMS is not painful and doesn’t seem to cause amnesia or cognitive problems. The side effects seem limited to headaches and some muscular discomfort, though a few people have had seizures during therapy.
TMS can stimulate neurons’ activity or change the signaling patterns of cells that are already active. Given its capacity to do both noninvasively, from the start it offered the promise of a powerful treatment for a range of neuropsychiatric disorders that seem to involve dysfunctions in brain circuits, such as depression, schizophrenia, epilepsy and obsessive-compulsive disorder.
In the mid-1990s, researchers began treating depression with repetitive TMS, administering treatment in regular sessions over weeks or months. Initial trials suggested the technique was effective at least some of the time, and in 2007 the U.S. Food and Drug Administration approved it to treat depression in people who don’t respond to medication and talk therapy. It has since also been used to treat chronic pain and to aid recovery from stroke.
At the University of Louisville, Casanova’s lab has been at the forefront of some of the research on TMS. He, Sokhadze and others in his group were exploring what was so different about the brains of people with autism when it occurred to him that TMS might have potential as a treatment. “It was almost a Eureka moment,” he says. But he couldn’t interest any TMS researchers in his idea, so eventually he invested in a machine for his lab to try it himself.
Balancing act:
I
n typical brains, neurons engage in a perpetual balancing act between excitation and inhibition in response to the endless flow of stimulation that comes their way. Too much inhibition can lead to depression, and too much excitation to both autism and epilepsy. (The latter may explain why many people with autism have seizures and show extreme sensitivity to touch and sound.)Different cells specialize in one activity or the other — stirring up networks or calming things down — and work together to maintain the balance.
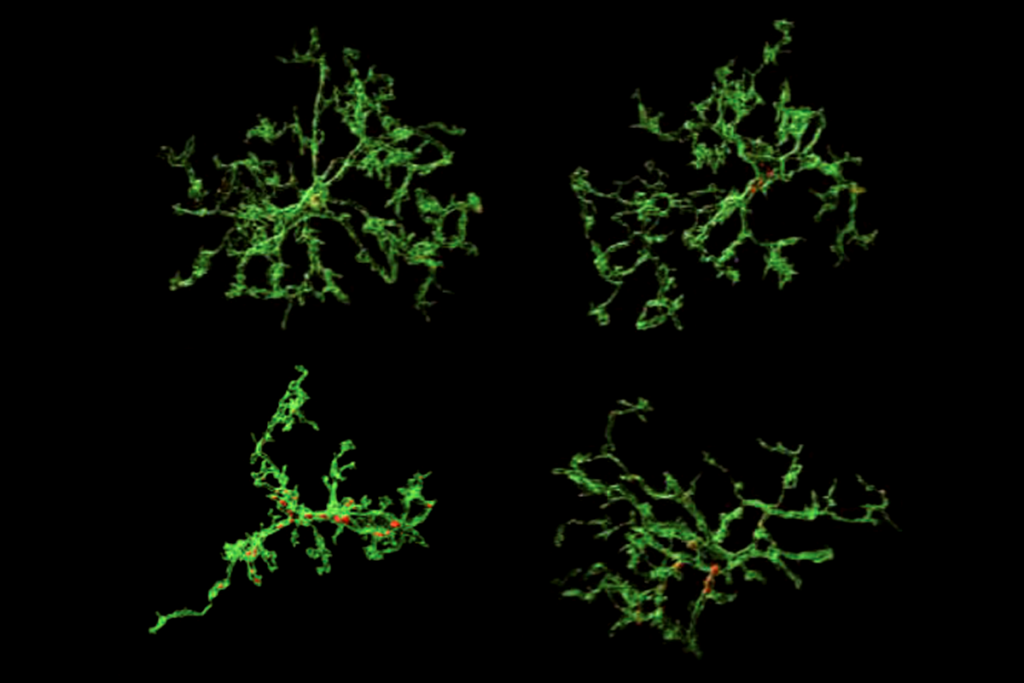
Casanova’s work suggests that some of the abnormality in autism brains occurs in mini-columns, vertical networks of cells that work together to process information. Pyramidal cells at the center of these columns are excitatory. Clustered around them, other types of cells, particularly double bouquet cells, turn down the signals so that only the most important information gets through. When this “shower curtain of inhibition” — a phrase coined by Hungarian scientist János Szentágothai — doesn’t work as it should, says Casanova, the signals spill out, drenching the nearby networks in stimulation.
In autism, the thinking is that TMS could correct the imbalance between excitation and inhibition.
The small currents created by TMS change neurons’ electrical charge and cause them to release chemical messengers, sending a ripple of activity to distant areas of the brain. High-frequency stimulation is thought to increase excitatory activity and a low frequency to increase inhibition. Preliminary results from Platt’s work with monkeys suggest that people with autism may benefit, for example, from applying TMS to increase excitation in an area of the brain associated with sociability.
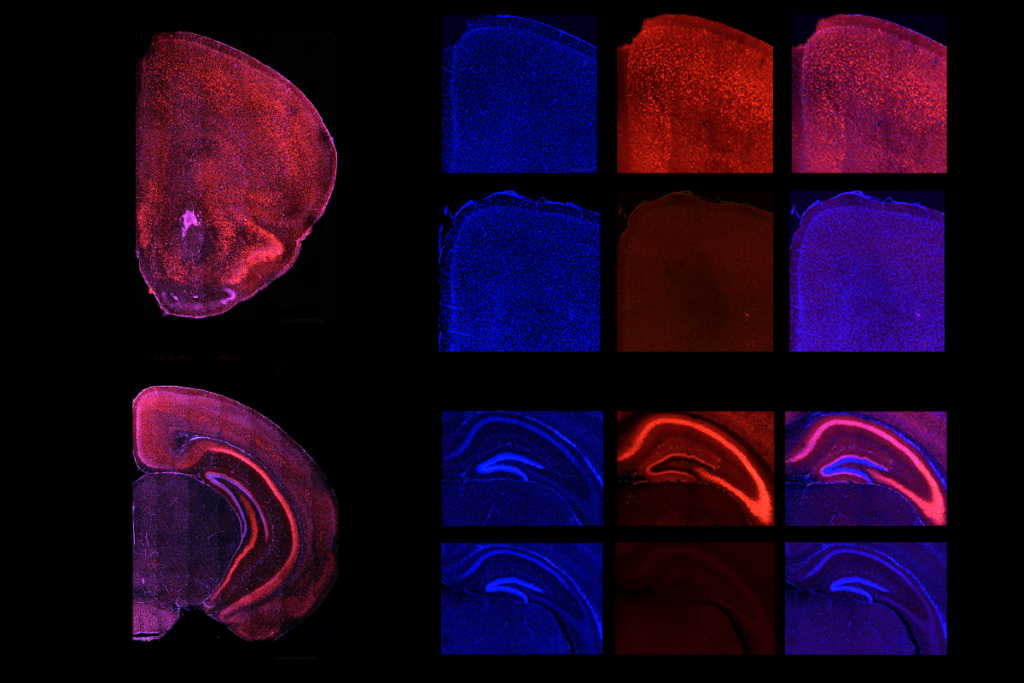
Conversely, in his experiments, including with Will, Casanova uses low-frequency stimulation to increase inhibitory activity in an area of the brain called the dorsolateral prefrontal cortex. This brain region is thought to be responsible for higher-order functions such as planning and abstract reasoning. Because the region is close to the brain’s surface, it is easily accessible to TMS, but is also well connected to the rest of the brain: As a result, any changes there may have beneficial effects in many other areas.
Since 2009, Casanova, who moved to the University of South Carolina in Greenville this summer, has published 14 clinical studies of TMS, involving nearly 200 people with autism in all. Several of the studies required the participants to perform a visual illusion task designed to trigger a high-frequency brain wave called gamma.
Gamma waves are involved in high-level attention processing and have been found to be abnormal in the brains of people with autism, often responding too strongly to distractions. Casanova’s group has found that after repeated bouts of TMS, people with autism process visual information more efficiently, making fewer errors in the illusion task. They are also less irritable and hyperactive and show fewer repetitive behaviors, at least for a while, than before the treatment. The effect is akin to rebooting a computer — something you eventually have to repeat.
Vivid changes:
A
t its best, TMS can produce dramatic changes.In 2008, Robison, author of the bestselling memoir “Look Me in the Eye,” enrolled in a TMS study led by Oberman and neurologist Alvaro Pascual-Leone at Beth Israel Deaconess Hospital in Boston.
Before that study, Robison says he was blind to other people’s emotions. “It’s as if you knew the world was black and white, but people talked about reds and blues and greens, and eventually you just became angry because you thought people were putting you on,” he says. “And then suddenly you go into the lab, a scientist does something to you and you walk out and see all the colors in the world. And you realize: It’s real.”
That first time, the effect only lasted a day or two, but that was enough for Robison. “You will never be the same because now you know from experience that there is this world of color, only you can’t perceive it,” he says. “It is a life-changing experience for a person who is fairly self-aware.”
Robison participated in several more TMS studies in 2009 and 2010 and was so affected by the experience that he made it the subject of his next book, “Switched On,” set to be published early in 2016.
However, Oberman and other scientists say they worry people with autism will extrapolate too much from Robison’s experience. No one else Oberman has worked with has undergone as dramatic or long-lasting a change as Robison did, she says.
For example, 17-year-old Nick (his real name has been changed for privacy reasons) was diagnosed with autism when he was in seventh grade. When he was 14, Nick joined a study in Oberman’s lab, and after one session of TMS, the team noted only one change: Nick became much more assured when asked to assign emotions to pictures of eyes.
But Kim Hollingsworth Taylor, Nick’s mother, saw significant differences in the way he carried himself afterward. “He turned his head and upper body to me as we talked, he did less toe-walking, and he walked an appropriate distance from me,” she says.
The effects lasted just a few days, but were encouraging enough that Nick’s father took him back to Oberman’s lab for several more off-label treatments of TMS, culminating in a 10-week period in 2013 during which he received TMS twice per week. This arduous schedule required father and son to move temporarily from their home in Minneapolis to Boston, where Oberman was then based.
“It seemed like the stimulation turned down the static for him,” says Taylor. “I told him how different he was and he said, ‘It’s like there’s more of me here now.’” For four months, she says, nearly all of Nick’s autism traits went away.
Flush with success, Taylor asked Oberman why TMS isn’t more widely available. When Oberman explained that the research is still in an early stage, Taylor, who has a background in medical technology, created a small nonprofit organization to help bring researchers together, raise funds for TMS research and provide information about the clinical use of TMS. Called the Clearly Present Foundation because of Nick’s comment about feeling more present, the organization has sponsored two conferences.
At the second, which took place in May in Salt Lake City, Utah, researchers took the first steps to organize a multisite trial of TMS. They hope to have thousands of participants, and to report results in two to three years.
Taylor says she dreams of the day when TMS is a proven treatment, widely available to anyone who walks into a clinic. Yet in the past year, all of the benefits Nick experienced from TMS have disappeared. His repetitive behaviors, obsessive-compulsive disorder and social isolation have all returned. “He is truly back to being stuck,” she says.
What’s more, Nick refuses to have anything to do with the treatment. “I’m in the painful position of working hard to push an agenda while my son gets worse and worse since he never wants any ever again,” says Taylor.
Early days:
N
ick’s story is a cautionary tale for anyone who reads too much into TMS’ benefits. Among scientists, even the most gung-ho TMS advocates admit that the research so far has severe limitations.
For example, none of Casanova’s studies were fully randomized or controlled for a placebo effect, a phenomenon in which people with a condition — and their families — see improvement because they so badly want to.
To account for the placebo effect, researchers would need to create a sham TMS, but that has proven to be tricky. The electrical current causes twitching in the muscles of the face and hands, which so far has been difficult to simulate. Depending on the part of the brain that is being targeted, the sensation can be unpleasant: “It feels like someone is snapping a rubber band against your head,” says Oberman. In other words, anyone who has experienced TMS will find the experience unmistakable.
The only rigorously controlled trial of TMS took place at Australia’s Deakin University, where cognitive neuroscientist Peter Enticott and his colleagues used a different kind of TMS machine for both the real treatment and the placebo.
The machine, called Brainsway, employs a helmet instead of a handheld coil, and is designed so that its magnetic field penetrates more deeply into the brain than with traditional TMS. This deep-brain TMS has its own limitations: It creates a broader magnetic field and so is more difficult to target precisely than is traditional TMS. But Enticott’s team was able to fit a helmet with a sham TMS device that clicks and vibrates without delivering a field. That isn’t a perfect solution, but the researchers did not know which of the 28 adults with autism participating had received TMS and which had not.
Enticott’s team also used high-frequency TMS to target a different area: the dorsomedial prefrontal cortex. This brain region is thought to be involved in theory of mind, the ability to recognize others’ emotions and beliefs, something people who have autism struggle with.
The team stimulated the brains of 15 adults with autism for 15 minutes a day for two weeks, and assessed their social skills before the treatment, immediately after, and one month after that. The participants showed a small but statistically significant improvement in social relating at the one-month mark, as well as a small dip in social anxiety, compared with the 13 participants who received sham treatment. It was a promising result, but, stresses Enticott, “we’re nowhere near being able to say that TMS is going to be an effective treatment for autism.”
TMS generates 1 Tesla of power, as much as a magnetic resonance imaging machine, so it must be administered only by skilled professionals in a lab. Because it is still an experimental approach, anyone trying it ought to do so only as part of a research study.
That hasn’t stopped the proliferation of for-profit TMS labs. “People are paying tens of thousands of dollars for this completely unvalidated treatment,” says Enticott. “It’s obscene.”
Buoyed by TMS’ promise, many people with autism have also begun experimenting with brain stimulation on their own — a testament to the lack of therapies available for autism.
Do-it-yourself treatment uses an entirely different method, transcranial direct current stimulation (tDCS), to try to change brain function. Electrodes placed on the forehead deliver a weak current — usually between 1 and 2 milliamps — to the brain. This is almost certainly too weak to have the same effect on neurons’ activity as TMS does, says Oberman. Still, she is launching a study of the method just to be sure.
TMS’ effectiveness in autism may well turn out to mirror what’s been learned in depression: The treatment works only for some people, and usually requires maintenance sessions. By using TMS to study the brains of people with autism, researchers may be able to predict who is most likely to benefit from the technique.
So far, Casanova says, he has found it to be most effective in people with autism who have an intelligence quotient above 70. Sadly, that means he hasn’t been able to help his own grandson, who was diagnosed with severe autism long after Casanova became an expert in the field.
Casanova’s work does seem to have helped Will, who finished sixth grade this spring in a mainstream school with a full-time aide. Will’s grandfather says the past year has been “a perfect storm” of progress, with Will more attuned to other people and able to do things he used to fear.
To take just one example: This time leaving the lab after his TMS session, Will was nearly as excited as when he’d arrived. He was looking forward to a treat that previously would have been unimaginable: riding downstairs in the elevator.
Syndication
This article was republished in Newsweek.
Recommended reading
Functional connectivity links with autism, not ADHD; and more
Ramping up cortical activity in early life sparks autism-like behaviors in mice

New method identifies two-hit genetic variation in autism; and more
Explore more from The Transmitter
Daniel Nicholson discusses how Schrödinger’s book ‘What is Life?’ shaped years of biology, research

Our searchable repository of useful research can restore trust in federally funded basic science
