Welcome to the September issue of Going on Trial, a monthly newsletter covering clinical trials and drug development for autism and related conditions. This month, we examine potential eye-tracking-based measures for clinical trials and dig into an adapted scale for Angelman syndrome.
Eyes on the prize:
Earlier this month, two new studies described an electronic tool that uses eye tracking to aid autism diagnosis. The tool, called EarliPoint, tracks where a child looks while watching videos of social interactions and detects autism with 84 percent accuracy, as measured against expert clinician diagnoses. The technology could have promise outside the world of diagnosis, too, some experts say.
“Whether it’s exactly this device or a different kind of eye-tracking assay, there’s a lot of interest in and a lot of promise for their use in clinical trials,” says James McPartland, professor of child psychiatry and psychology at Yale University, who was not involved in the studies. He is also lead investigator of the Autism Biomarkers Consortium for Clinical Trials, which tested an assortment of eye-tracking biomarkers in 2022. “There’s an extremely strong body of evidence over a long period of time that the things that they’re measuring here are meaningful and valid and reliable differences in autistic people.”
EarliPoint or other eye-tracking tools could be used to stratify autistic trial participants into different subgroups — either to home in on the group most likely to respond to a treatment or to create a more homogenous sample, McPartland says. They could also be used to quantitatively determine whether a treatment is working, he adds.
EarliPoint “is really, really interesting and useful,” but there’s more data to collect before it can be used on its own in clinical trials, says Thomas Frazier, professor of psychology at John Carroll University in University Heights, Ohio, who wasn’t involved in the study. The two studies focused on the tool’s diagnostic applications and collected data accordingly, “which is great — definitely needed, awesome. But that’s different than an outcome measure.”
For example, the tool was tested on children ages 16 to 30 months. This age range is appropriate for a diagnostic tool but too young for most drug trials, McPartland says. To be used as an outcome measure, the tool must also be shown to produce consistent results over time (also known as test-retest reliability) and be sensitive to change, and participants must not get better at the task with practice, Frazier says. To stratify subgroups, researchers must also establish that the measurements have a meaningful relationship to a phenotype, McPartland adds.
To this end, an EarliPoint clinical trial is underway and recruiting participants. It aims to evaluate how well the system can detect changes in the verbal and social skills of autistic children receiving a developmental intervention such as applied behavior analysis.
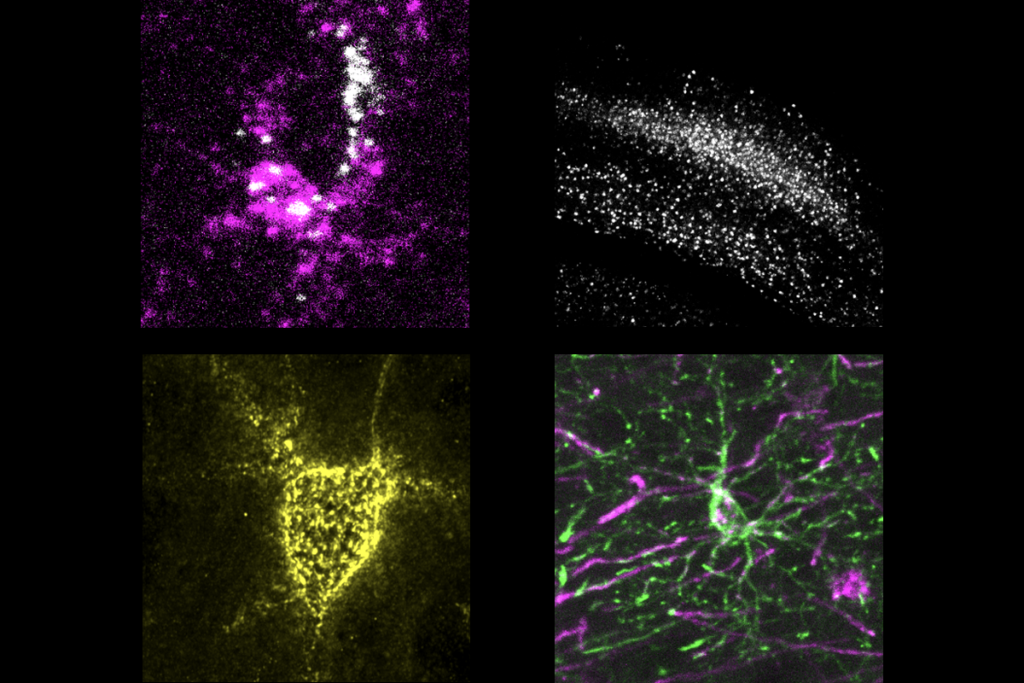
Frazier is also working on an eye-tracking-based tool specifically for use in clinical trials. It involves an app that works on any computer or tablet with a webcam and at least a 10-inch screen. The app uses artificial intelligence to analyze webcam-collected data on a person’s gaze patterns, as well as their reading speed, facial expressions and attention. Frazier, who is chief executive officer of Autism Analytica, an autism software company, says he plans to submit his tool to the U.S. Food and Drug Administration (FDA) for clearance later this year and use it in a clinical trial measuring changes in cognitive and social skills in response to applied behavior analysis.
He also sees potential for his team’s tool in drug trials. “If we keep doing the same trials we’ve been doing forever, I really worry that we’ll get failures,” Frazier says, “not because the drugs don’t work, but because we can’t detect it.”
Angelman assessments:
The drug gaboxadol did not improve Angelman syndrome traits in a 2020 phase 3 trial. But the study provided an opportunity to test a new outcome measure: an Angelman-specific version of the Clinical Global Impression (CGI) scale, published earlier this month in the European Journal of Paediatric Neurology.
Trained clinicians typically use the CGI to rate the severity of a condition and improvement after treatment. The adapted Angelman CGI includes separate ratings for four traits that tend to be altered in people with the syndrome: fine and gross motor skills, expressive and receptive communication, behavior, and sleep.
Compared with other measures, the adapted CGI accurately detected changes in sleep, socialization and behavior, but not in communication. Tweaks to the rating anchors may improve the scale’s ability to detect more subtle trait changes.
“We’re going to continue to use this outcome measure, but we’re also going to anticipate maybe there’ll be some concerns that it’s not specific enough or too arbitrary,” says lead investigator Christopher Keary, behavioral director of the Angelman Syndrome Behavioral Clinic at Massachusetts General Hospital in Boston.
It’s important to devote adequate time to training clinicians on how to use the scales to ensure consistency between scorers, he adds. But other experts say they worry extra training won’t be sufficient, and that condition-specific changes won’t make up for issues with the original CGI. “I think that there’s something inherent in the scale that’s structurally deficient,” says Wen-Hann Tan, associate professor of pediatrics at Harvard Medical School, who was not involved in the CGI adaptation.
Drug samples:
- A phase 2 clinical trial to test the effects of oxytocin on bone health in autistic children and teenagers began recruiting participants. The hormone oxytocin regulates bone health, and autistic youth tend to have lower bone density than their non-autistic peers, which puts them at heightened risk of fractures. The trial aims to enroll 96 participants.
- An experimental drug that selectively activates certain receptors for GABA decreases repetitive self-grooming in a rat model of autism, according to a preprint published 26 August in bioRxiv. It also improved social function in male rats only. But the molecule did not alter the increased dopamine neuron activity characteristic of the model.
- On 19 September, the FDA issued draft guidance on how to demonstrate a drug’s effectiveness by combining confirmatory evidence with data from a single clinical trial. The agency is accepting comments on the guidance for 90 days.
That’s all for September! Make sure you subscribe so you can receive this newsletter in your inbox every month, and feel free to get in touch with feedback or story ideas: [email protected]