Life’s blood
The first approved stem cell trial for autism will soon be under way. Is there a rationale for testing stem cells to improve symptoms of the disorder?
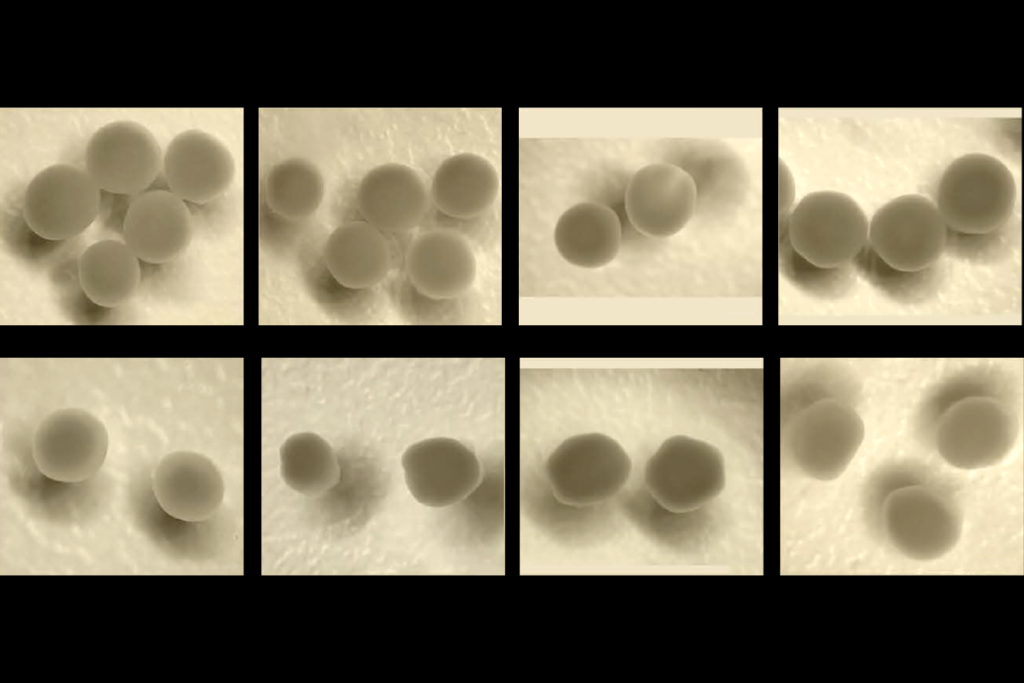
The first stem cell trial for autism, approved this month by the U.S. Food and Drug Administration, will soon be under way. Last week, researchers from the nonprofit Sutter Neuroscience Institute in Sacramento, California, announced plans to test stem cells derived from a child’s own umbilical cord blood as a treatment for autism.
The study aims to include 30 children between the ages of 2 and 7 who have been diagnosed with autism of no known genetic cause. Only children whose umbilical cords were banked with the Cord Blood Registry, a commercial stem cell bank, are eligible. Researchers plan to primarily look for improvements in language skills.
Lead investigator Michael Chez, director of pediatric neurology at Sutter Medical Center, says the rationale for the trial comes from animal research showing that stem cells can repair neuronal connections, as well as from unpublished results from cord blood transplants in children with cerebral palsy.
But whether these findings translate to treatment of autism is unclear.
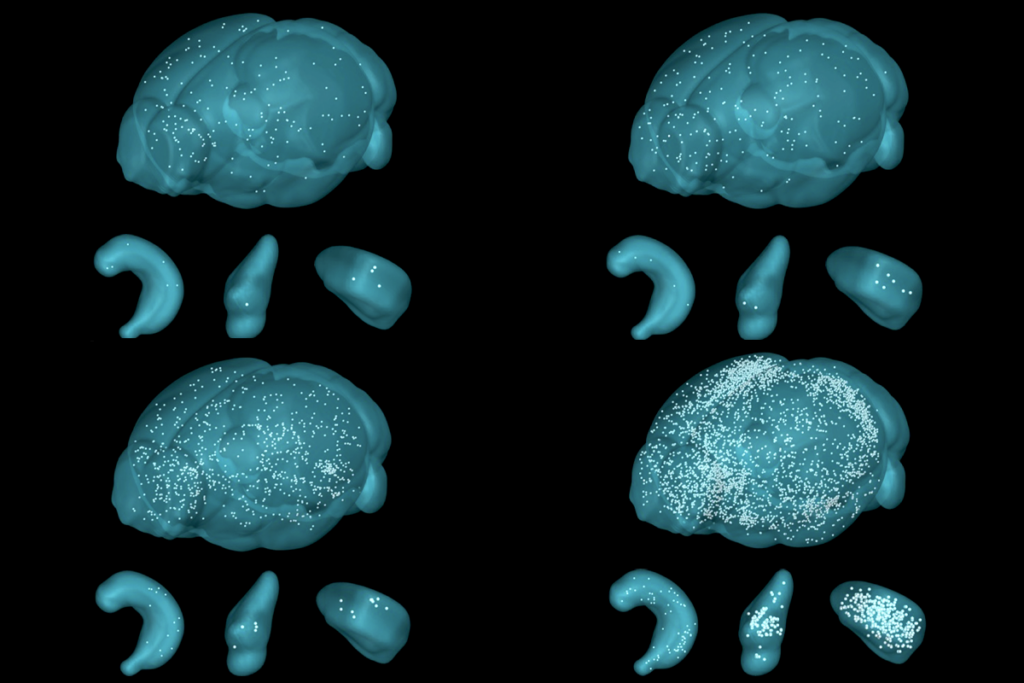
For example, it’s not known whether stem cells from cord blood transplants make their way into the human brain.
“I think the possibility of repairing central nervous system connections by adding new neurons is extremely unlikely,” says Paul Patterson, professor of biological sciences at the California Institute of Technology in Pasadena, who studies immunology and autism.
However, Patterson says he applauds the design of the trial: Half the study group will get a stem cell injection and the other half a placebo. The two groups will switch halfway through, with each child receiving one stem cell injection and one placebo over the course of the 13-month study.
Rigorous design:
The trial is also double-blind, meaning that neither parents nor the doctors running the study will know in which order a given child got the stem cell injection and placebo. That helps to eliminate the so-called placebo effect in parents and researchers who want the treatments to work. The placebo effect has been a particularly troublesome influence on autism research.
This type of rigorous trial is especially important because stem cell therapies are already being offered around the globe for autism and other disorders, with little reliable evidence on their effectiveness or safety.
Some cases of autism have been linked to problems with the immune system, and Chez speculates that stem cells might help resolve immune problems, perhaps by lowering inflammation. He says his team plans to look at measures of immune function in children in the trial, but it won’t be a primary outcome measure.
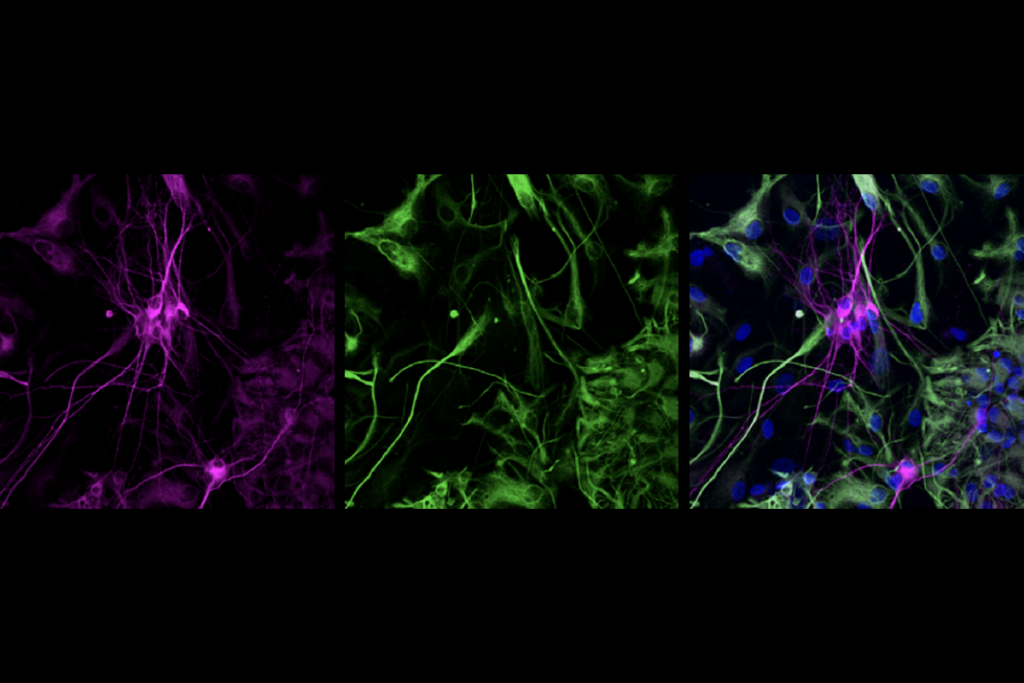
According to Patterson, considerable evidence suggests that mesenchymal stem cells, which are derived from bone marrow and other tissue, can alleviate inflammation. But there is much less data available on whether stem cells from cord blood have the same power, he says.
A study from Patterson’s lab, published earlier this month, suggests that bone marrow transplants can curb autism symptoms in mice.
But that is different from a transfusion of cord blood. In a bone marrow transplant, the individual’s existing immune system is first wiped out. (That’s a dangerous procedure and highly unlikely to be approved in a clinical trial to treat autism unless there is striking evidence of its effectiveness.)
Because the trial will use the children’s own cells, they won’t need to take drugs to suppress the immune system, which is required when patients get bone marrow transplants. But if an individual’s autism is linked to a problematic immune system, it’s unclear whether transfusion of his or her own cells will help.
It’s also unknown how long the transplanted cells might survive in these children without prior chemotherapy or irradiation, says Patterson.
“Nothing is known definitively about how stem cells act at this stage,” adds Chez. “That is what we continue to investigate.”
Recommended reading

Gene-activity map of developing brain reveals new clues about autism’s sex bias
Parsing phenotypes in people with shared autism-linked variants; and more
Boosting SCN2A expression reduces seizures in mice
Explore more from The Transmitter
Engrams in amygdala lean on astrocytes to solidify memories
Ant olfactory neurons reveal new ‘transcriptional shield’ mechanism of gene regulation
