Journal club: Does lithium in drinking water contribute to autism?
A study published in JAMA Pediatrics suggests that autism is more common among people born in areas with high levels of lithium in drinking water, but it is too soon to say whether prenatal lithium exposure is truly a concern.
Lithium, an alkali metal, is the 33rd most common element in the earth’s crust, commonly found in drinking water and not regulated in the U.S. by the Safe Drinking Water Act. Lithium also happens to be an established and effective psychiatric medication (some have even described it as “magic”): It is a first-line treatment for bipolar disorder and also prescribed off-label for other purposes, such as major depressive disorder and suicidal behavior. Although lithium’s use in psychiatry dates to the mid-19th century, much remains unknown about its mechanisms of action. However, lithium’s neuromodulatory effects on the brain are evident, hence its long-standing use in psychiatry.
With this context, a recent JAMA Pediatrics study by Zeyan Liew and colleagues linking lithium in drinking water during pregnancy to autism in children in Denmark is quite interesting. The study sampled lithium concentrations in Denmark’s public waterworks — mostly in 2013, with additional samples from 2009 and 2010 — for roughly half of the Danish population. The authors then used a statistical model to spatially interpolate lithium concentrations for the entire country and assigned lithium exposures for 52,706 children — including 8,842 with autism — born 2000 to 2013 based on their mothers’ residential addresses during pregnancy. Compared with children in the lowest quartile of lithium exposure, those in the highest quartile had nearly 50 percent higher odds of autism.
To echo an editorial by David Bellinger that accompanies the study, this work has two notable strengths: First, it was not a fishing expedition; it was a hypothesis-based study with plausible support from basic science research, and it was driven by a need for more safety data about an important element, with implications for public policy regarding safe drinking water as well as medication management during pregnancy. Second, the study assessed children’s outcomes using diagnostic codes listed in Denmark’s data-rich national registers, which have excellent positive predictive value — if a person has a diagnostic code pertaining to autism, there is a 97 percent chance they truly have autism.
T
here are some limitations. In a case-control study such as this one, a primary concern is whether the sampling strategy induced bias. The new work included all eligible autistic children in Denmark, and it randomly selected controls from the Danish population. If cases and controls are sampled from different geographic populations, then the findings could simply reflect geographical differences in autism prevalence or confounders rather than the geographical differences in lithium concentrations in drinking water. In countries such as the U.S. and Sweden, autism is better identified (i.e., more prevalent) in large cities, where better diagnostic resources are available. This trend is evident in Denmark as well, where Copenhagen and other large urban areas contributed 57 percent of the new study’s autistic participants but only 49 percent of its controls. One would expect these percentages to be equal if there were no sampling bias.Moreover, the urban areas had significantly higher lithium concentrations: 46 percent of the autistic participants in urban areas were exposed to the highest quartile of lithium, whereas only 14 percent of those with autism in rural areas were exposed to the highest level. Although the authors attempted to adjust for area of residence, residual bias from this sampling strategy likely remains: When the researchers removed rural persons from the analysis, lithium’s effects in the 2nd and 3rd quartiles nearly halved from 24 and 26 percent higher odds of autism, respectively, to 14 and 16 percent.
Although the authors found that a single unmeasured confounder does not explain the findings, it is still plausible that multiple factors together could. Maternal mental health and individual-level socioeconomic status are likely related to both lithium exposure and autism in children, but neither was accounted for.
The accuracy of quantifying lithium exposure is also an issue, given that there is no data available on the dose, location or timing of the participants’ actual exposures. As Bellinger pointed out in his editorial, lithium concentrations likely remain stable over time because geogenic sources generally do not change. But lithium’s association with autism risk could easily be interpreted as relevant to other periods beyond pregnancy exposure (e.g., one year before pregnancy or one year after pregnancy), which would lead to different interpretations about the nature of risk posed by lithium.
Finally, the “guesstimate” nature of lithium exposure measurement here also leads to another challenge: The authors did not appear to use any statistical method to account for the large uncertainty inherent in the exposure measurement — thus, the point estimates are likely to be biased (although in which direction is anyone’s best guess) and the confidence intervals artificially narrow.
All of this is to say we cannot tell from this one study alone whether prenatal lithium exposure is truly a concern for autism. Liew et al. are rightfully cautious to not overinterpret their findings, and their call for more scrutiny is prudent.
W
hat scrutiny, then, should be done? Randomized clinical trials, the gold standard for public health studies, are unlikely to be feasible given the ethical challenges in studying pregnant persons as well as the logistical challenges of conducting large studies over an extended period sufficient to capture autism diagnoses. Therefore, observational studies are necessary.Lithium medication use during pregnancy has never been implicated, let alone studied, in autism, even though lithium concentrations from medication are orders of magnitude higher than the highest concentrations reported in the present study from drinking water. Therefore, an obvious starting point is a study of whether lithium medication use during pregnancy is associated with autism.
Replication studies of lithium in drinking water and autism should be performed in different geographic areas, ideally with drinking water measurements of lithium that correspond well to actual biological concentrations measured in pregnant persons. The field also appears to lack animal model studies of lithium regarding neurodevelopment and what doses, durations or timings of exposure might be relevant to risk. Genetic and epigenetic analyses of response to lithium should be conducted to inform potential determinants of individual susceptibility to lithium’s effects on neurodevelopment, if any.
Finally, to jump to the finish line, what does the present study mean for how members of the general public should think about lithium in their drinking water or how public policy should regulate drinking water? In one word: nothing.
It should be noted that studies across multiple countries have suggested that higher concentrations of lithium in drinking water are associated with fewer psychiatric hospital admissions, fewer deaths by suicide, lower incidence of dementia and lower rates of violent and non-violent crimes. Some scientists have proposed to add lithium to drinking water to benefit brain health, akin to water fluoridation to improve dental health, although the evidence is still preliminary and there are obvious ethical issues.
At this stage of research, lithium’s effects on autism are uncertain. Yet this study by Liew and colleagues is still valuable for hypothesis generation and provides a valuable data point for reference by the next scientists to study this issue.
Visit our Global Autism Prevalence Map
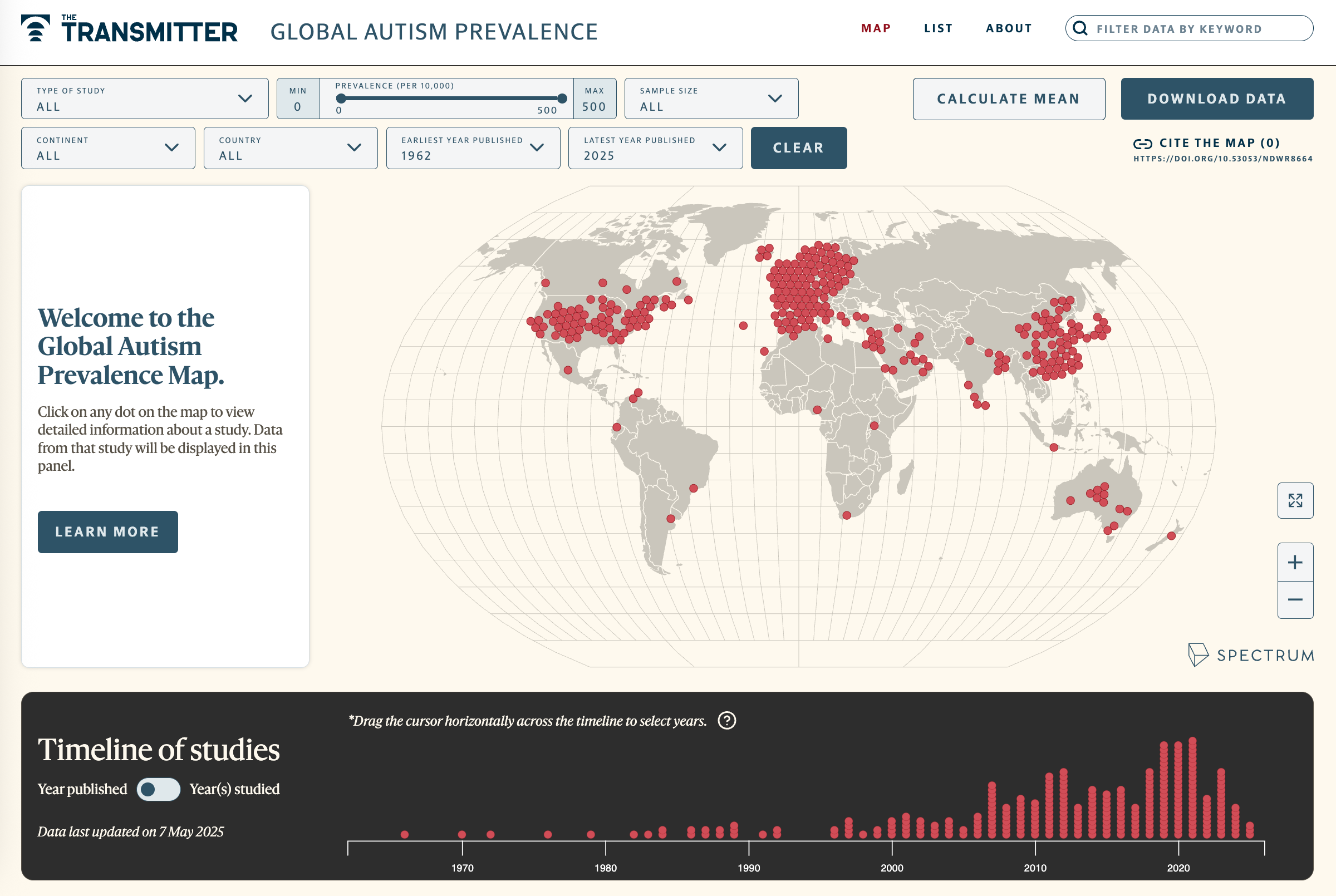
Explore more >
Recommended reading

New organoid atlas unveils four neurodevelopmental signatures
Explore more from The Transmitter

Anti-seizure medications in pregnancy; TBR1 gene; microglia

Autism prevalence increasing in children, adults, according to electronic medical records