An intranasal form of the hormone oxytocin is no more effective than placebo at increasing social behaviors in autistic children, according to what may be the largest clinical trial of the treatment to date. The results were published today in The New England Journal of Medicine.
Because of oxytocin’s role in strengthening social bonds, researchers have considered it as a candidate treatment for autism for more than a decade. Small trials hinted that the hormone could improve social skills in some autistic people, such as those with low blood levels of oxytocin or infants with Prader-Willi syndrome, an autism-related condition.
But the new results, based on 250 autistic children, suggest that “oxytocin, at least in its current form, is probably not helpful for the majority of kids with autism,” says Evdokia Anagnostou, professor of pediatrics at University of Toronto in Canada, who was not involved in the new work.
The null results “change things,” says lead researcher Linmarie Sikich, associate professor of psychiatry and behavioral sciences at the Duke Center for Autism and Brain Development in Durham, North Carolina. “Most people still felt like there was a good chance that this would be treatment for many people with autism.”
This type of research is prone to publication bias, in which non-significant results are less likely to be published than significant ones, says Daniel Quintana, senior researcher in biological psychiatry at the University of Oslo in Norway, who was not involved in the study. For that reason, the new work is “an important contribution to the field,” he says, but “it does not alone put to rest the idea of using intranasal oxytocin as an autism treatment.”
Measuring gaps:
The autistic children in the trial, aged 3 to 17 years, inhaled a nasal spray containing either oxytocin or a placebo for 24 weeks. The participants started on a low dose of the hormone, administered once per day. If that dosage was well tolerated, it was gradually increased over time to a higher dose twice per day.
The participants’ parents or guardians filled out a series of questionnaires to rate their child’s social behaviors at the start of the trial and at regular intervals thereafter.
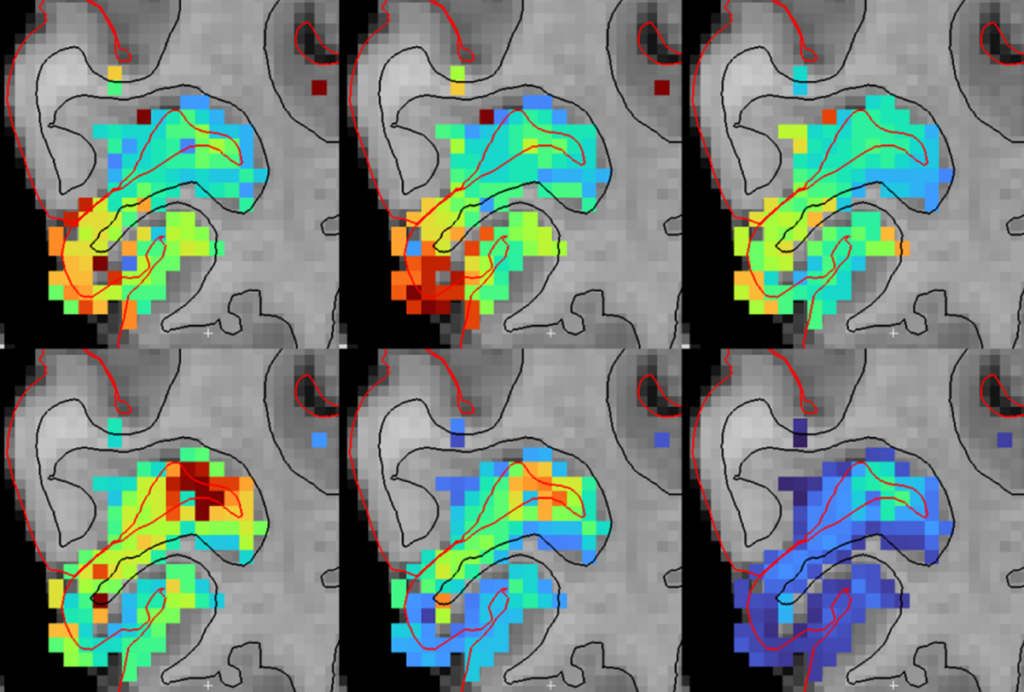
Four weeks into the trial, participants in both groups showed improvements in social withdrawal, according to a modified portion of the Aberrant Behavior Checklist, the trial’s primary outcome measure. Those changes persisted for the remainder of the trial. Both groups also showed gains in sociability and social motivation, as measured by the Pervasive Developmental Disorders Behavior Inventory and the Social Responsiveness Scale, respectively. The results did not vary with the participants’ ages, verbal abilities or blood levels of oxytocin.
“Just giving the drug is probably not enough to do anything,” Anagnostou says. But, she adds, it’s possible the treatment improves other aspects of social function — such as association, cognition, affiliation and reward — that may not be picked up by the questionnaires the new trial used.
In September, a small trial of intranasal oxytocin in children with Phelan-McDermid syndrome, a neurodevelopmental condition that often results in autism, similarly found no effect on social behaviors reported by parents.
“The issue of how we measure social behavior is one that the field is grappling with and remains unresolved,” says Adam Guastella, professor of clinical psychology at the University of Sydney in Australia, who was not involved in either study.
Salience signal:
As researchers have learned more about oxytocin’s role in the brain, ideas about how it affects social behavior have shifted, says Larry Young, director of the Translational Center for Neuroscience at Emory University in Atlanta, Georgia, who was not involved in either of the new studies. The hormone is now understood not to enhance sociability in general, but to increase the salience of social stimuli, he says, which helps people better perceive and learn from things such as facial expressions and body movements.
Given this new understanding, pairing oxytocin treatment with some type of behavioral training may prove to be a more effective way to harness the hormone’s effect as a treatment, Young says.
And considering the heterogeneity of autism, it’s possible that a subset of autistic people will still respond to an oxytocin-based treatment, Anagnostou says. The children in the trial could have had different forms of autism that affected their responses, but the study did not characterize the participants in that way, she says.
Further research is also needed to determine whether administering oxytocin intranasally is the most effective way to deliver the drug to the brain, researchers say. For one, Guastella says, it’s not clear that the hormone is taken up by the brain in this form.
Even if it does, because of the way the body regulates hormone levels, it may be more effective to use a compound that activates oxytocin receptors, or even a parallel system in the brain, rather than flooding the brain with oxytocin itself, Anagnostou adds.
It’s important to think about whether “giving oxytocin is the best way to manipulate the system, or should we think about other strategies,” she says.
Sikich says that intranasal oxytocin treatment is unlikely to have an effect on sociability, but she agrees that certain genetic subtypes — for example, people who are “particularly responsive to oxytocin, or [for whom] oxytocin is completely gone” — may still benefit.
For now, however, the study should give parents and clinicians pause when considering treating autistic children with off-label intranasal oxytocin, multiple researchers say.
“[The study] will appropriately dampen enthusiasm,” Guastella says.