The interplay of common, rare variation in autism
Autism researchers should ditch the false dichotomy between common inherited variants and much rarer random mutations.

Two seemingly different genetic influences contribute to autism: inherited factors and spontaneous mutations. We are racing to discover more about each of these paths, and yet this should not be viewed as a race. Indeed, an ‘either-or’ framing may well shortchange what we can learn about how these two influences may interact to govern an individual’s risk of developing autism spectrum disorder.
Genetic variation, like autism itself, occurs along a spectrum.
First, the basics: Autism is common in the population, affecting at least 1 in 100 people. And it runs in families, which suggests that most risk factors for the condition are inherited. But people with autism have fewer children on average than their neurotypical peers.
These general features are nearly identical to those of another heritable condition: schizophrenia. The pattern is so distinctive and so precisely matched that coincidence is unlikely. Also, the two conditions share genetic risk factors.
Autism and schizophrenia are serious conditions that, by the rules of genetics and natural selection, permit scientists to predict how frequently inherited, associated genetic variants should appear. For example, a mutation that arises and confers a small, two-fold increase in risk for autism is expected to be found only at a frequency of 0.01 percent.
Variants with such a low frequency and impact cannot be detected in case-control studies until the study includes hundreds of thousands of people. However, variants that increase risk by only 10 to 20 percent — a tiny effect on the individual — can be quite common and relatively easy to detect. Indeed, a 2014 schizophrenia study of close to 40,000 people documented more than 100 such sites.
That means common variants with weak effects can contribute significantly to autism risk. Conversely, and perhaps counterintuitively, variants with larger effects — increasing risk by 50-500 percent — make smaller contributions to inherited risk. That’s because these higher risk variants are less likely to be passed onto the next generation and almost never reach a meaningful population frequency.
At the same time, de novo mutations — mutations that arise spontaneously before or shortly after fertilization — may exist and carry high risk because natural selection has not yet had an opportunity to remove them from the population. With few exceptions, de novo mutations do not contribute to heritability.
Polygenic risk:
Over the past decade, the primary engine for discovery in human disease genetics has been genome-wide association studies (GWAS). This technique screens whole genomes in order to identify gene variants, generally common and inherited ones, that show up more often in people with a condition than in controls.
The sum of risks carried by all these common genetic variants across a genome is referred to as the polygenic risk score, and can be used to estimate individual risk.
In autism research, GWAS are only now reaching the scale at which the first robust findings were achieved for schizophrenia. Statistically speaking, the small sample sizes to date have not allowed researchers to confirm individual variants as risk factors. Overall, however, common variants account for roughly 50 percent of the heritability of autism1.
Several studies over the past few years, each with fewer than 10,000 participants, have revealed significant overlap between genetic risk for autism and for schizophrenia. Unexpectedly, these studies also found a positive correlation between genetic risk for autism and intelligence scores and educational attainment2,3,4. Common risk for autism is also associated with problems in social communication in the general population5.
Results from an unpublished Danish study of more than 15,000 people with autism — including more than 10,000 who had never been studied before — has found robust evidence for at least five common variants and reinforced the positive overlap with schizophrenia risk and higher intelligence scores. These findings suggest that autism researchers are following in the footsteps of schizophrenia researchers in terms of understanding the common inherited component of a complex neurological condition.
Ultra-rare variation:
Extremely rare genetic variants, including de novo mutations, may contribute less to heritability than common variants do. But there’s no question that these rare events have provided the majority of known genetic markers and can be much more individually impactful.
Influential early papers described a surprising role for de novo copy number variants (CNVs) — duplication or deletion of specific chromosomal regions — in autism6. Well-known examples of deletions at chromosomal region 22q11 or 16p11.2 arise de novo with some frequency — as often as 1 in 10,000 births.
Discovery of these events provided the first concrete link between a specific variant and autism. However, because these events delete 20 or more genes, they did not immediately point to a specific causal biological process.
What’s more, many of the same CNVs are enriched in schizophrenia and other neurodevelopmental conditions. This discovery provided the first solid evidence that genetic events associated with autism do not underlie only features associated with autism. Rather, they are general risk factors for features that span a variety of clinical diagnoses.
The same CNVs are sometimes seen in controls and so are estimated not to cause autism but to confer a perhaps 10- to 20-fold increased risk. By the laws of genetic probabilities, these variants are unlikely to survive more than a few generations. That means they don’t contribute much to inherited risk, though because of their high mutation rates they contribute meaningful population risk.
Pointed risk:
As genome sequencing has become faster and cheaper, researchers have scaled up their search for point mutations — alterations of a single nucleotide in DNA — particularly those that might severely damage a protein-coding gene. By sequencing the genomes of parents and their children, researchers can identify rare de novo point mutations. Landmark studies published in 2012 demonstrated that people with autism carry an excess of mutations that disable one copy of a gene.
As studies of this kind have increased in size, the de novo point mutations seen in autism have been shown, like common variants, to be distributed over hundreds of genes, such that mutations in any one gene contribute to only a tiny fraction of cases.
Some 10 to 20 genes have reached a robust level of ‘genome-wide significance,’ with point mutations showing up over and over again. Below this is a more numerous group of genes on a ‘false-discovery rate’ list, containing genes in which de novo point mutations are found at collectively higher rates than expected by chance. However, it remains unclear which of these genes are genuine autism risk factors.
Because rare mutations are gene-specific, they can yield important insights into the clinical and biological aspects of autism. For instance, some of the first genes associated with autism (such as ARID1B, SYNGAP1, DYRK1A, ADNP and SCN2A) are also strongly associated with more severe conditions such as intellectual disability and epileptic encephalopathy. At the same time, people with autism who carry these mutations are more likely to also have intellectual disability, seizures and motor delay.
Working together:
We and others continue to work on these two fronts — trying to identify common polygenic variants and rare de novo variants. Our results may help advance knowledge of the underlying biology. However, it is not too early to consider how these two categories of genetic variation may interact to govern an individual’s risk of autism.
A novel family-based analytic method allows us to explore, for the first time, the combination of common polygenic and rare de novo contributions7. This approach has shown clearly and robustly that polygenic risk contributes equally to autism with and without intellectual disability.
Common genetic variants provide at least part of an explanation for why some people with severe, damaging mutations develop autism and others do not.
These interpretations are compelling and intriguing, but we’re still in the earliest stages of understanding the full genetic architecture of autism. What is clear is that studies of common and rare variants both still need substantial increases in scale to articulate a complete set of contributing genes.
More than anything, researchers should view these studies as mutually informative, rather than competitive, as we aim for a fuller understanding of autism.
Mark Daly is chief of the Analytic and Translational Genetics Unit at the Massachusetts General Hospital.
References:
- Gaugler T. et al. Nat. Genet. 46, 881-885 (2014) PubMed
- Clarke T.K. et al. Mol. Psychiatry 21, 419-425 (2016) PubMed
- Hagenaars S.P. et al. Mol. Psychiatry 21, 1624-1632 (2016) PubMed
- Bulik-Sullivan B. et al. Nat. Genet. 47, 1236-1241 (2015) PubMed
- Robinson E.B. et al. Nat. Genet. 48, 552-555 (2016) PubMed
- Sebat J. et al. Science 316, 445-449 (2007) PubMed
- Weiner D.J. et al. Nat. Genet. (2017) PubMed
Recommended reading

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys

PTEN problems underscore autism connection to excess brain fluid
Explore more from The Transmitter
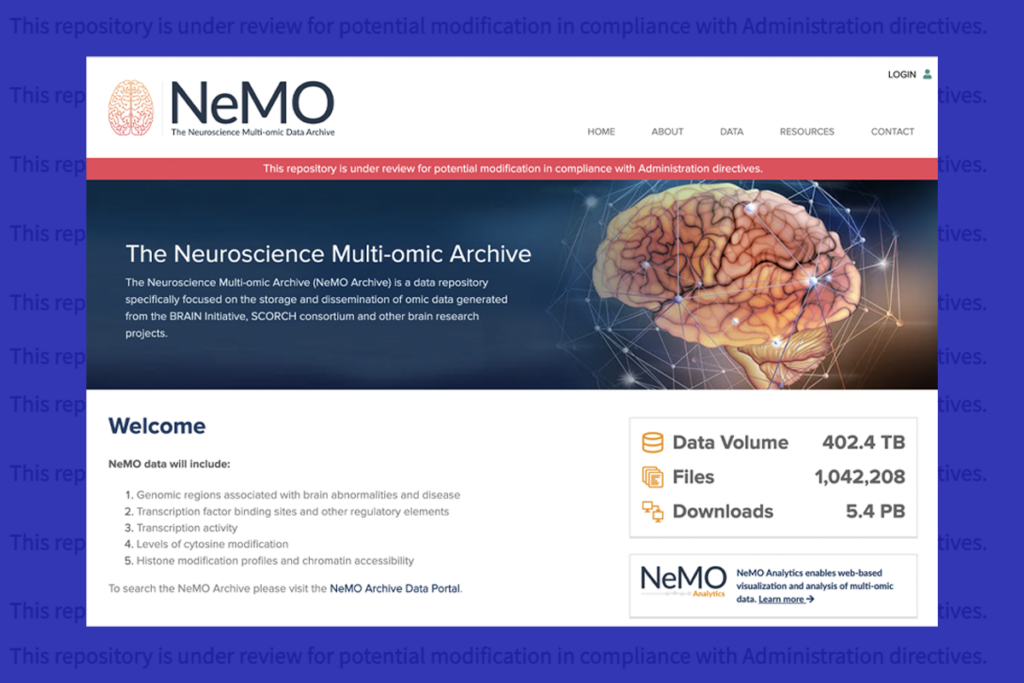
U.S. human data repositories ‘under review’ for gender identity descriptors