Injecting CRISPR into fetal brain may correct autism mutations
Researchers are edging closer to a therapy for Angelman syndrome — a condition related to autism — that involves injecting the gene-editing enzyme CRISPR into the fetal brain.

Researchers are edging closer to a therapy for Angelman syndrome that involves injecting molecules that can edit genes into the fetal brain. They have already succeeded in mice and say the approach could eventually treat people with the syndrome.
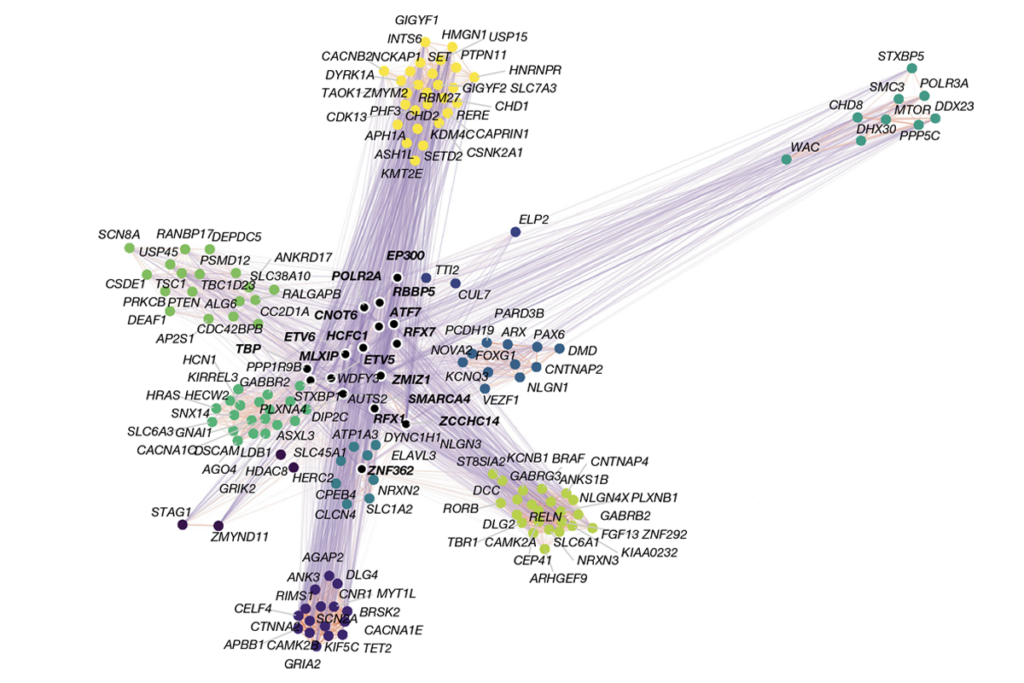
The work is of high interest because a similar strategy could also work for other genetic conditions linked to autism.
But the prospect of injecting molecules into fetal brains poses ethical questions, experts caution.
People with Angelman syndrome have severe developmental delays, seizures, impaired speech and, often, autism. They have a missing or mutated copy of a gene called UBE3A on the copy of chromosome 15 they inherit from their mother. The paternal copy is generally silent, so they have virtually no activity of the protein in neurons, where it is needed to modulate signals between neurons.
Other teams have tried to introduce a healthy copy of the gene or to unsilence the paternal copy in mice. But these strategies are ultimately impractical because they involve drugs with harsh side effects or giving children injections every few months.
In the new research, presented at a conference in February, Mark Zylka’s team injected the gene-editing enzyme CRISPR-CAS9 into the brains of embryonic mice. The method unsilenced the paternal copy of UBE3A in the mice. The researchers also rescued UBE3A expression in cultured human neurons, according to the unpublished findings.
Research suggests that the syndrome’s traits can be avoided if UBE3A is turned on before birth1. The work underscores the importance of intervening early in development.
“The earlier you put the genes back and try to fix the problem, the better the therapeutic benefit will be,” says Zylka, director of the Neuroscience Center at the University of North Carolina at Chapel Hill. “There’s a lot of interest in trying to break down this barrier to being able to treat prenatally.” The treatment may be tried in people within three to four years, Zylka says.
Experts caution that the work must be repeated in mice before it can be tested in people — and that scientists will first need to resolve the ethical concerns.
“Doing any gene manipulation in the fetal brain is kind of a dangerous thing to do, so that does concern me,” says Antonio Bedalov, associate member of the Fred Hutchinson Cancer Research Center in Seattle.
Scientists should move carefully because this is evolving research, others say.
“The idea that you could treat a fetus with [an enzyme] is just a very uncharted area, and there could contain a lot of risks,” says David Segal, professor of chemistry at the University of California, Davis, who was not involved in the research. “We need to move with caution.”
Over the goal line:
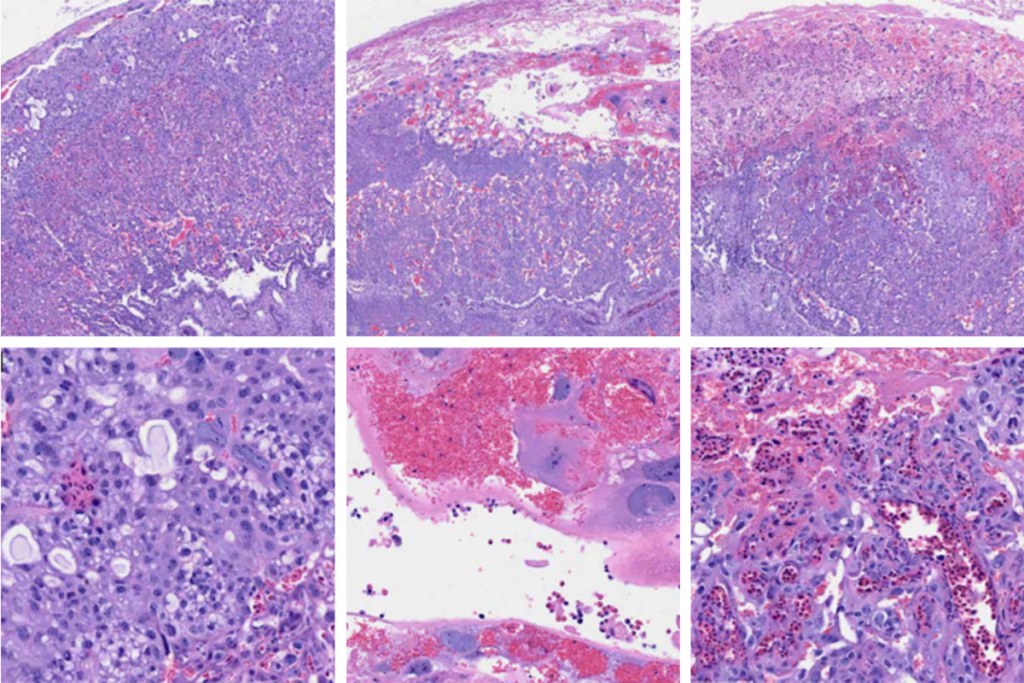
The team made an incision in pregnant mice and used a microscope to look into the near-transparent brains of the embryos. They used glass needles to inject a modified virus carrying a version of CRISPR-CAS9 into 10 embryonic brains lacking UBE3A, about three days before birth. They attached the enzyme to an RNA ‘guide’ that directs it to bind near the UBE3A gene.
The enzyme blocks a strand of noncoding RNA that typically prevents the paternal copy of the gene from being expressed. It is unclear whether it does so by snipping that section of DNA or by simply sticking to the DNA and mucking up the works.
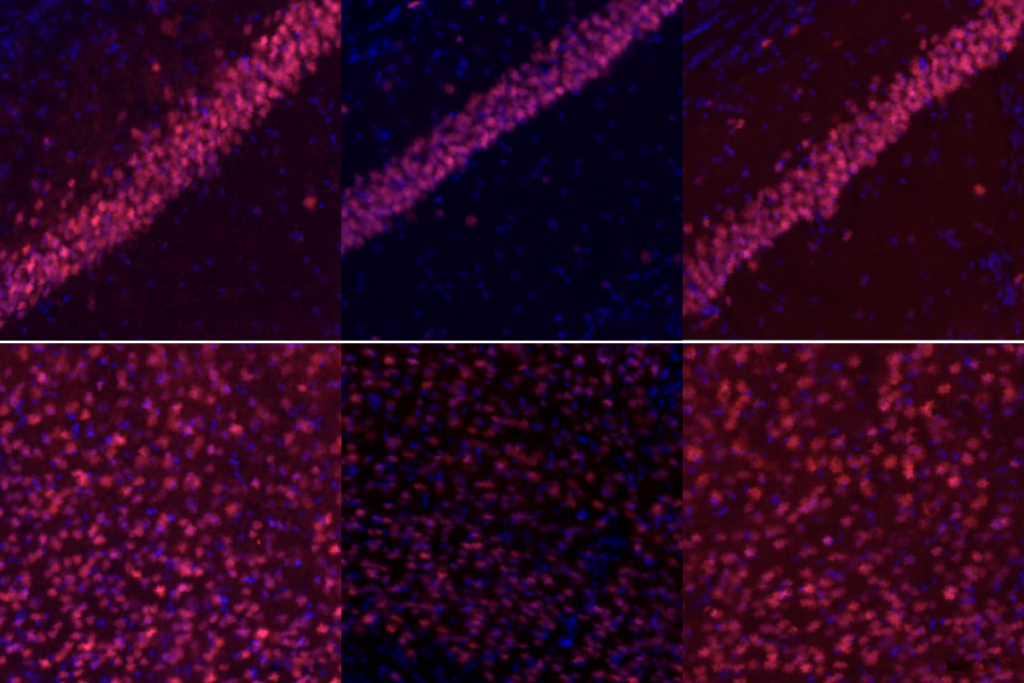
Regardless, UBE3A is expressed in about half the neurons in the mice’s cerebral cortex at 5 months of age, compared with none at all in controls.
Some people have a rare, mild form of Angelman in which UBE3A expression is at about 10 percent of the usual levels2. So restoring expression to 50 percent may be enough to make a difference for people with the syndrome, Zylka says. “We think that’s going to push us over the goal line.”
The researchers have not yet tested whether the therapy alters the mice’s behavior. Nor have they screened the mice for unintentional mutations elsewhere in the genome. (Zylka says the results are likely to be published later this year and will include behavioral data.)
Safe solution:
The chances of rogue mutations are high with viral delivery of CRISPR-CAS9, says Hye Young Lee, assistant professor of neuroscience at University of Texas at San Antonio, who was not involved in the research. Nanoparticles — miniscule packaging molecules that break down after delivering the enzyme — are less likely to introduce such mutations and may be safer, she says.
Zylka says they may also be able to avoid editing the genome entirely. His team delivered a disabled version of the enzyme to cultured human neurons missing UBE3A, and he says this seemed to be just as effective at restoring UBE3A expression as the functional form.
Zylka’s team plans to try this approach in mice. They also would like to explore dialing up UBE3A expression in specific brain regions, which is easier to do than transfusing molecules across the whole brain.
The strategy also holds promise for other conditions involving single genes. For example, Bedalov says his team plans to test a similar approach for treating Rett syndrome, caused by mutations in a gene called MECP2.
References:
Recommended reading
Post-infection immune conflict alters fetal development in some male mice
In-vivo base editing in a mouse model of autism, and more
Organoid study reveals shared brain pathways across autism-linked variants
Explore more from The Transmitter

Dendrites help neuroscientists see the forest for the trees
