Immune molecule may mediate effects of maternal infection
Infections during pregnancy increase levels of an immune molecule in the placenta that alters brain development and behavior in mice.
Infections during pregnancy increase levels of an immune molecule in the placenta that affects brain development and behavior in mouse pups. Mice born to mothers missing the receptor for the molecule, called interleukin-6 (IL-6), do not show these effects.
Researchers presented the results yesterday at the 2016 Society for Neuroscience annual meeting in San Diego. The study could help explain the link between maternal infection and autism risk.
The findings also appeared 9 November in Brain, Behavior, and Immunity1.
“Viruses and bacteria, they cannot be directly transmitted to the fetus,” says Wei-Li Wu, postdoctoral researcher in Sarkis Mazmanian’s lab at the California Institute of Technology in Pasadena, who started the work in the lab of the late Paul Patterson. “So immune activation in the mother can be a potential mechanism for psychiatric disorders.”
Previous studies have shown that infections during pregnancy raise the risk of having a child with autism by as much as 37 percent. Maternal infections also alter the brain and behavior in mice. In January, researchers showed that blocking IL-17 prevents these alterations.
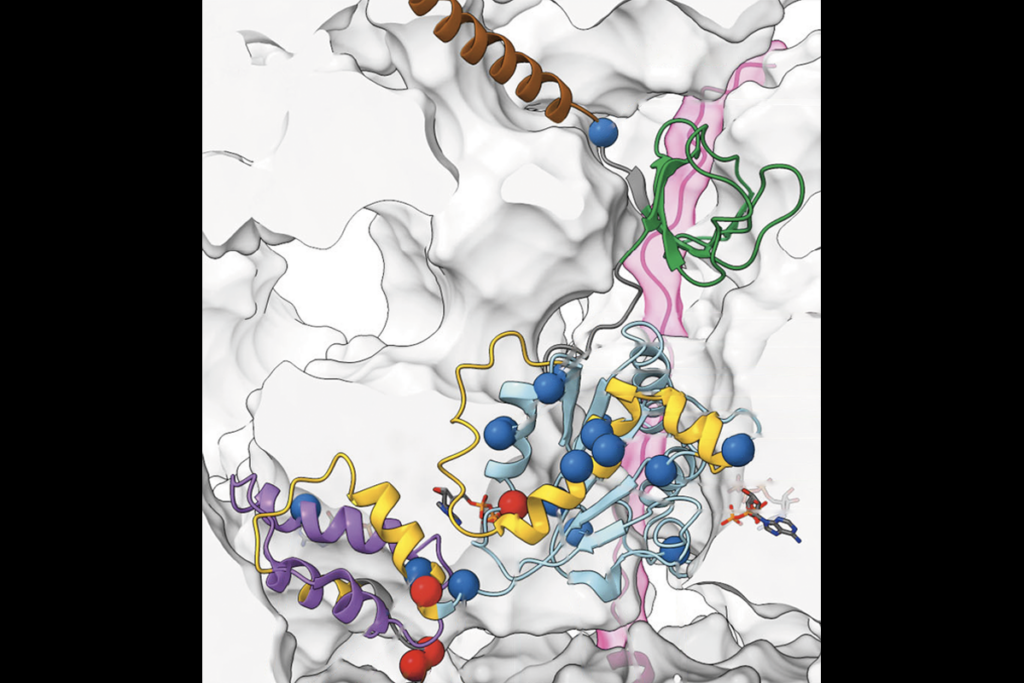
Wu and his colleagues focused on IL-6, which acts upstream of IL-17. They found that maternal infection leads to a surge of IL-6 activity in the placenta and in the fetal brain. Inhibiting the IL-6 pathway in mouse mothers eases autism-like behaviors in the pups.
“Now we have a target,” says Mazmanian, professor of biology at Caltech. “This is still way off in the future, but neutralizing IL-6 in mothers who are at risk for having a child with autism may result in improvements in the child later on.”
Infection connection:
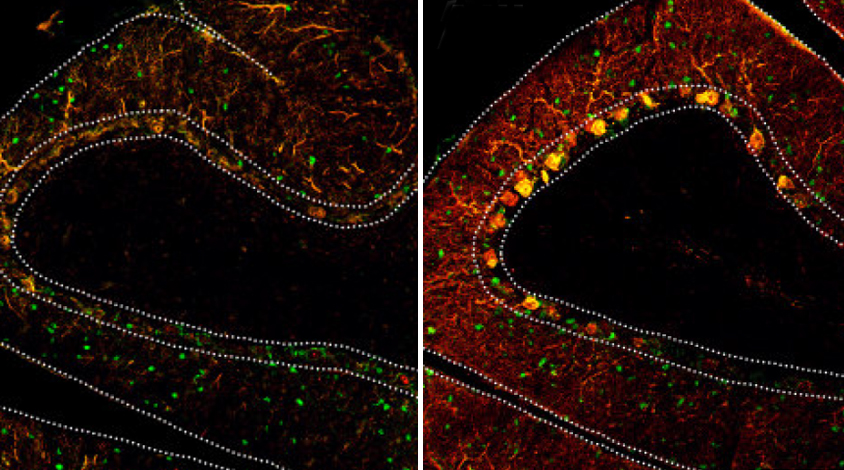
Wu and his colleagues gave typical pregnant mice an acid called poly(I:C) that mimics an infection and stimulates the immune system. The pups spend less time than controls interacting with another mouse and more time burying marbles, a feature reminiscent of the repetitive behaviors seen in autism. The mice also have fewer neurons than typical mice in the cerebellum, a brain region involved in motor coordination and implicated in autism.
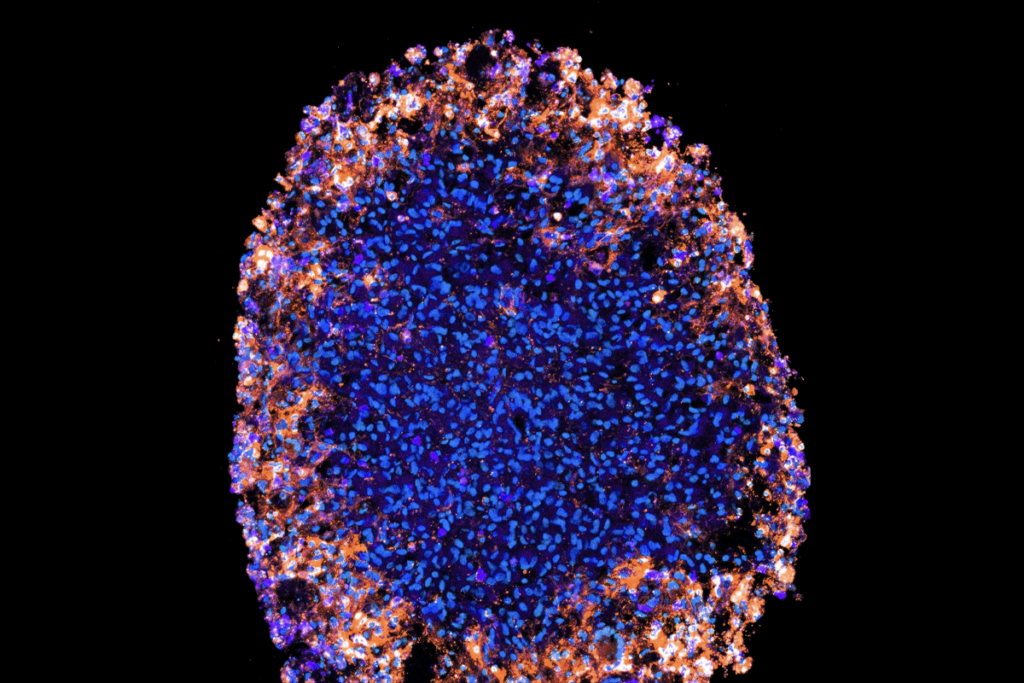
The researchers found high levels of IL-6 and signs of inflammation in the placenta and the fetal brains of the acid-treated mice.
But when the scientists repeated the experiment in pregnant mice lacking the IL-6 receptor, the animals did not mount an inflammatory response in the placenta. The pups from these mice had a typical number of cerebellar neurons and did not act antisocial or show repetitive behaviors.
The findings support the idea that a pregnant woman can pass to her baby molecules she produces in response to infection.
“I think the conclusion is that there are many soluble molecules made by immune cells that can alter brain development,” says Betty Diamond, head of the Center for Autoimmune and Musculoskeletal Disorders at the Feinstein Institute for Medical Research in Manhasset, New York, who was not involved in the study.
The next step, Mazmanian says, is to figure out how exposure to IL-6 in the womb might affect behavior later in life.
For more reports from the 2016 Society for Neuroscience annual meeting, please click here.
References:
- Wu W.L. et al. Brain Behav. Immun. Epub ahead of print (2016) PubMed
Recommended reading

Among brain changes studied in autism, spotlight shifts to subcortex
Home makeover helps rats better express themselves: Q&A with Raven Hickson and Peter Kind
Explore more from The Transmitter
Dispute erupts over universal cortical brain-wave claim
Waves of calcium activity dictate eye structure in flies