Human ‘mini-brains’ make themselves at home in mice
Spheres of brain cells derived from people and implanted into mouse brains recruit blood vessels and integrate with mouse neurons.
Editor’s Note
The findings discussed in the conference report below were published 16 April 2018 in Nature Biotechnology1.
Spheres of brain cells derived from people and implanted into mouse brains recruit blood vessels and integrate with mouse neurons. The work represents a technical leap in the field of brain organoids, also known as ‘mini-brains.’ It also raises ethical questions.
Researchers presented the unpublished findings today at the 2017 Society for Neuroscience annual meeting in Washington, D.C.
Scientists can generate organoids from human stem cells, or even skin. After several weeks in culture, the stem or skin cells transform into brain-like clumps of neurons, astrocytes and other brain cells. Depending on the method used, the cells can form layers of tissue similar to those seen in the human brain.
Organoids are more realistic than traditional cell cultures. But they lack the complexity of living organisms, says Abed Mansour, a postdoctoral fellow in Fred Gage’s lab at the Salk Institute in La Jolla, California, who presented the work. “What we wanted to do in these experiments is increase the physiological relevance of the model,” Mansour said during his talk.
Even before the conference, news of the findings raised concerns about creating this sort of ‘humanized’ mouse. The National Institutes of Health’s guidelines don’t allow implanting human stem cells directly into a mouse brain, but the rules don’t apply to the implantation of organoids.
Some say the fears are overblown, however.
“Several people have injected human fetal cells into rodents and monkeys,” says Alysson Muotri, associate professor of pediatrics and of cellular and molecular medicine at the University of California, San Diego. “I don’t think this is new territory, because the authors did not show that the organoids are having any sophisticated brain waves or that the animal has changed its behavior.”
Of mice and men:
Mansour and his colleagues generated organoids from human stem cells. When the organoids grew to about 2 millimeters in diameter, they implanted them into the brains of mice.
The researchers first removed a small piece of the animals’ skulls to expose their brains. They then removed a small piece of the mouse brain to make room for the organoids. They inserted the organoids and then closed the animals’ skulls with a clear window. All of the implants targeted one hemisphere of the brain.
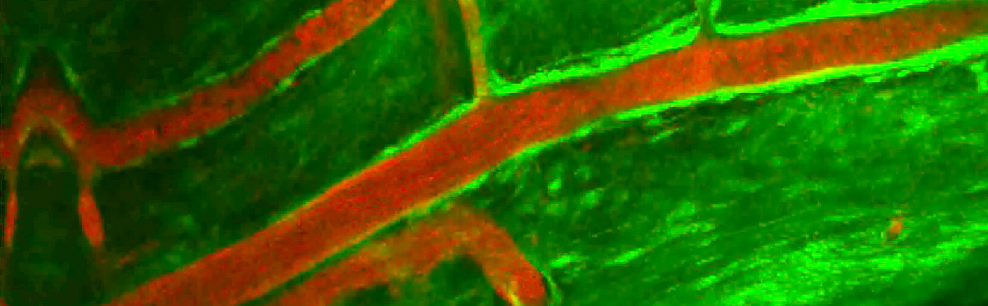
After 14 days, the researchers inspected the hybrid brains. This revealed a mix of neurons and star-shaped support cells called astrocytes. After eight months, neurons in the organoids send projections called axons out across the implanted hemisphere.
“We were quite surprised by how many axons projected from the implant to the host,” Mansour says.
The researchers investigated whether the neurons form functional connections, using a method called live calcium imaging. They found that neurons from the implanted organoid fire in sync with mouse neurons, suggesting the two sets are communicating with each other.
The team also examined whether the implanted organoids receive a blood supply. They injected a marker into the blood and visualized the blood vessels through the clear window. Live brain imaging revealed blood coursing through the vessels. The researchers determined that the vessels and the blood inside come from the mice.
Muotri and others are exploring ways to hook organoids up to a blood supply in a lab dish. This would allow them to supply the cells with human blood, limiting any confounds from the mouse blood, Muotri says. “We want to stay away from the mouse as much as possible,” he says. That method would also allow them to study thousands of organoids at once, which is necessary for screening drugs.
Beyond offering a way to study organoids, the new work suggests that mini-brain transplants could provide a therapeutic option for certain conditions. Because the cells form functional connections with the host’s own neurons, it is possible they could replace damaged neurons or fix faulty circuits.
For more reports from the 2017 Society for Neuroscience annual meeting, please click here.
References:
- Mansour A.A. et al. Nat. Biotechnol. 36, 432-441 (2018) PubMed
Recommended reading

New organoid atlas unveils four neurodevelopmental signatures
Explore more from The Transmitter

The Transmitter’s most-read neuroscience book excerpts of 2025

Neuroscience’s leaders, legacies and rising stars of 2025


