How aripiprazole’s promise for treating autism fell short
Aripiprazole, marketed as Abilify, is widely thought to be safer than risperidone, the only other drug approved for use in autistic children. A decade’s worth of data suggests that is not true.

E
ven as a toddler, Jaymes Lesovoy was violent. He hit and bit his parents, and he tore apart his and his sisters’ toys. At 18 months of age, he was diagnosed with autism.Jaymes’ pediatrician suggested behavioral and speech therapy, but neither approach reined in the boy’s aggression. In 2006, when Jaymes was 2, the doctor prescribed risperidone — an antipsychotic medication that had been approved earlier that year to treat irritability in autistic children aged 5 and older. A few years later, he added a second medication to the mix — the seizure drug valproic acid — although Jaymes does not have seizures.
Still, Jaymes acted out at home and at school, and continued to do so for years. When he was 10, another doctor suggested Jaymes try a different antipsychotic: aripiprazole. That drug had been approved in 2009 to treat irritability in autistic children aged 6 and older.
Jaymes’ mother, Amber Lesovoy, was familiar with aripiprazole. She had taken the medication herself a year earlier for her own autism and bipolar disorder, and she had experienced an unusual side effect: trouble urinating, which disappeared after she stopped taking the drug. She worried Jaymes might also experience side effects but felt she had few choices left. “I was a teen mom,” she says. “I didn’t have a lot of life experience, so all I knew to do was what the professionals told me.”
Jaymes was underweight when he started taking aripiprazole, but within a few weeks, he was always hungry: “He would sneak food; he would eat huge amounts at mealtimes. Any chance he got to get food, he would take it,” Lesovoy says. The pounds started to pile on.
There were other, more disturbing changes. When he started with aripiprazole, his mother says, he began to flail his arms, kick his legs and scrunch up his face without warning — severe involuntary muscle spasms called tardive dyskinesia. (Jaymes was later diagnosed with Tourette syndrome, which his doctors say explains the leg-kicking.) After a year on the drug, Jaymes had gained 50 pounds. He had fewer angry outbursts, but Lesovoy decided the side effects were not worth it. Of all the drugs Jaymes had been prescribed, aripiprazole was “one of the worst,” she says.
It has been 11 years since the U.S. Food and Drug Administration (FDA) approved aripiprazole for children with autism. The drug, marketed as Abilify, initially had a reputation of having fewer side effects than risperidone, its only competitor in this population. But a decade’s worth of data suggest that is untrue. As with many antipsychotic medications, long-term use of aripiprazole can lead to tardive dyskinesia, as it did for Jaymes. It might also be linked to heart problems in autistic children. And perhaps most concerning, aripiprazole appears to cause just as much weight gain as risperidone, compounding a problem many children with autism already have.
“The weight gain is not subtle,” says Eric London, director of autism treatment research at the New York State Institute for Basic Research in Developmental Disabilities. He says he has discontinued the drug’s use in 15 to 20 percent of the autistic people he treats, one or two of whom have gained more than 100 pounds.
A string of lawsuits over the past several years have charged that aripiprazole’s developers, the pharmaceutical companies Otsuka Pharmaceutical and Bristol-Myers Squibb, did not adequately warn users of the drug’s potential side effects — including compulsive behaviors such as gambling, sex addiction and excessive shopping. Other lawsuits alleged that the companies marketed the drug illegally for conditions it may not help. Most doctors interviewed for this story were aware of the risks. One described aripiprazole as a “last resort” in his treatment arsenal — a drug intended only for children who harm themselves or others. Still, a few say they consider aripiprazole a cure-all that can ease minor behavioral problems such as general agitation. Many clinicians say they prescribe the drug for a year or longer. Unlike risperidone, though, aripiprazole has not been shown to work long term in children with autism. Neither Otsuka nor Bristol-Myers Squibb responded to repeated requests from Spectrum for comment.
From 2014 to 2016, more than 500,000 children were prescribed aripiprazole in the United States. And among children with autism, the number taking antipsychotic medications overall is about one in six, according to one 2016 study. “That is concerning and suggests possible over-prescription or overuse,” says Matthew Siegel, director of the Developmental Disorders Inpatient Research Collaborative at Spring Harbor Hospital in Westbrook, Maine. “Those are our most powerful, potentially most problematic drugs. Should that really be the most common [type of] drug we use?
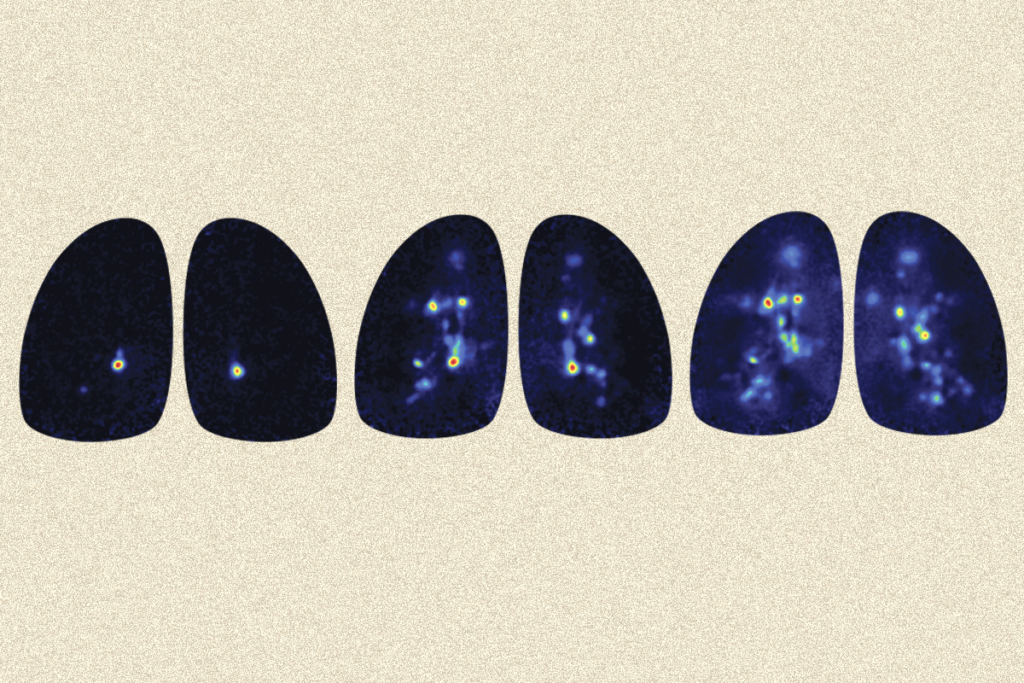
The most common adverse events reported in autistic children who took aripiprazole, according to data collected by the U.S. Food and Drug Administration. The agency does not verify these reports, and many other adverse events may go unreported.
| Category | Term | Count |
|---|---|---|
| Gastrointestinal | Gastrointestinal problems | 11 |
| Gastrointestinal | Nausea and vomiting | 20 |
| General | Fatigue | 21 |
| Metabolic | Appetite conditions | 18 |
| Metabolic | Diabetes | 14 |
| Metabolic | Other hyperglycemic conditions | 10 |
| Metabolic | Weight gain | 44 |
| Musculoskeletal | Atypical muscle tone | 7 |
| Musculoskeletal | Muscle-related problems | 6 |
| Musculoskeletal | Musculoskeletal conditions | 7 |
| Neurological | Changes in consciousness | 25 |
| Neurological | Dystonias | 7 |
| Neurological | Headache | 11 |
| Neurological | Mental impairment | 7 |
| Neurological | Movement conditions | 35 |
| Neurological | Neurological problems | 15 |
| Neurological | Tremor | 8 |
| Psychiatric | Anxiety | 24 |
| Psychiatric | Atypical behavior | 18 |
| Psychiatric | Behavior problems | 33 |
| Psychiatric | Mood problems | 24 |
| Psychiatric | Self-injury | 12 |
| Psychiatric | Sleep problems | 14 |
Source: U.S. Food and Drug Administration. Analysis by Jaclyn Jeffrey-Wilensky. Graphic by Krista Fuentes.
High hopes:
A
ripiprazole was discovered decades before it was approved for use in children with autism. Scientists at Otsuka Pharmaceutical, based in Tokyo, Japan, started work on the compound in the late 1970s and teamed up with Bristol-Myers Squibb more than a decade later to develop it into pill form. In 2002, the two big companies together brought that pill to market under the brand name Abilify, originally branding it as a novel antipsychotic to treat schizophrenia.Many doctors say they had high hopes for the drug at first — in part because it purported to work differently from all of its predecessors. Whereas other atypical antipsychotics, including risperidone, inhibit the neurotransmitter dopamine, aripiprazole blocks dopamine only some of the time (the exact mechanism is unknown). For that reason, the drug was expected to cause fewer side effects than risperidone. Because it also acts on the neurotransmitter serotonin, from 2004 to 2016 the FDA signed off on its use for a laundry list of other conditions tied to either dopamine or serotonin, including bipolar disorder, depression and Tourette syndrome.
The agency approved risperidone for autistic children in 2006, and soon after, Bristol-Myers Squibb and Otsuka started testing aripiprazole for that same use. In a 2009 study of 218 children with autism, they found that those who took the drug for eight weeks significantly improved on a standard test of irritability compared with controls. A second 2009 study in 98 children reinforced those results. Both studies hinted that children treated with aripiprazole may gain weight and have severe muscle tremors, but they concluded that the drug is safe and well tolerated overall.
Based on those trials, in 2009 the FDA approved aripiprazole to treat irritability in autistic children. Some researchers say they remember that soon after, drug representatives were touting aripiprazole as safer and at least as effective as risperidone. “When the sales reps came or when [aripiprazole] was presented, it was presented as, you know, ‘It’s an effective drug but has less weight gain compared to risperidone,’” says Antonio Hardan, professor of psychiatry and behavioral sciences at Stanford University in California. He says he does not remember specific interactions with drug representatives but recalls discussing the new approval with his colleagues. “People were excited about it,” he says.
Sales of aripiprazole skyrocketed. In 2013, it was the highest grossing medication in the U.S. But it also drew lawsuits from thousands of people over side effects. The companies also faced lawsuits over how they marketed the drug. According to charges brought by the U.S. Department of Justice, drug representatives had visited doctors’ offices to promote aripiprazole’s use in children before the FDA had approved it for that use. Otsuka and Bristol-Myers Squibb both denied any wrongdoing, but both agreed to settlements: In 2007, Bristol-Myers Squibb agreed to pay $515 million to the U.S. Department of Justice, and Otsuka agreed to pay the department more than $4 million a year later. Bristol-Myers Squibb also settled a 2016 suit for $19.5 million that alleged it had marketed the drug for off-label use — that is, for conditions the drug was not approved to treat. In 2016, the FDA compelled Otsuka and Bristol-Myers Squibb to update the drug’s warning labels.
According to Michael Oldani, a medical anthropologist at Concordia University in Mequon, Wisconsin, the companies’ aggressive marketing helped to expand aripiprazole’s use to conditions such as autism. By merely conducting studies to extend the drug’s use to children, its makers also became eligible under FDA rules to extend the life of their patent for at least six months from the original expiration date of October 2014. That extension allowed the companies to retain exclusive rights to the drug — and to continue pricing it at about $800 a month for a typical dose. By contrast, generic versions of the drug now available run to about $15 a month.
The companies overplayed the drug’s safety from the outset, Oldani says. He worked as a drug representative for Pfizer from 1989 to 1998. He also served as an expert witness in a 2013 case against Bristol-Myers Squibb related to Abilify’s off-label promotion and side effects. “The big thing for me is always side effects,” Oldani says. “The mythology with [aripiprazole prescriptions] is they were super-duper safe.”
Risky reaction:
A
t least one thing has become clear after a decade of aripiprazole’s use: The drug’s effects can vary dramatically between people. That’s something Vida Penikas, who has three autistic children, learned firsthand.When Penikas’ son J. was a toddler, he rarely spoke and was obsessed with anything that could spin. He was diagnosed with autism around age 5. He did well in school and was reasonably happy until he entered middle school, his mother says, when he spiraled into a dark depression. (Spectrum is using the boys’ first initials to protect their privacy.)
Penikas brought J. to their nurse practitioner. It was 2008, the year before aripiprazole was approved for autistic children, but the nurse practitioner recommended the drug “right off the bat,” Penikas says. “He said they’ve seen that Abilify works well with autistic kids.” Almost immediately, J. calmed down. His depression lifted and his outbursts waned. The drug worked so well that J. took aripiprazole until he turned 21 three years ago and no longer seemed to need it.
J.’s younger brother T. had an entirely different experience. He was diagnosed with autism after he started school, and by the time he was 9, he was having intense anxiety attacks. At first, the doctor prescribed several drugs that did little to ease the boy’s anxiety. Based on J.’s experience, Penikas thought aripiprazole might help and suggested it.
It turned out to be a nightmare, she says. Within months, T. became newly obsessed with random objects — at first Tic Tac candies, then duct tape. Soon after, he became aggressive, the opposite of the drug’s intended effect. One day about 10 weeks after he started taking aripiprazole, T. put a kitchen knife to his neck and threatened to stab himself if Penikas kept him from attending a friend’s sleepover. Penikas called 911, and T. was admitted to a psychiatric hospital, where doctors decided to wean him off aripiprazole. When he stopped taking the drug, his aggression waned.
“I would say [aripiprazole] works pretty well for a lot of people,” says Sarah Cheyette, a pediatric neurologist at Sutter Health in San Carlos, California. But there are notable exceptions, she says. Without research to identify who the likely responders are, clinicians have relied largely on their own judgement about when and to whom to prescribe aripiprazole. Some say they prescribe risperidone for children who are hyperactive, compulsive or have erratic sleep patterns, and turn to aripiprazole if a child has a family history of obesity or diabetes, presuming it is associated with less weight gain.
But a growing body of research is beginning to suggest aripiprazole and risperidone may not be as different as doctors have assumed when it comes to side effects. One 2016 analysis of 11 randomized controlled studies of aripiprazole and risperidone found that they are about equally effective. That same year, a head-to-head comparison of the drugs found that weight gain from each is “uncannily similar,” says Craig Erickson, associate professor of psychiatry at the Cincinnati Children’s Hospital in Ohio, who led the study.
Prior to that study, “myself and others would go around the country … and we’d say, ‘Hey, we think there’s less weight gain [with aripiprazole].’ But then we really came around to this understanding,” Erickson says. “We think in true clinical practice over long-term treatment that we cannot differentiate weight gain between [the two drugs].” Similarly, although physicians have widely used aripiprazole to address self-injury, the drug may work best for children whose aggression comes from autistic meltdowns, according to a reanalysis of the original results.
Erickson says two trials he was involved in at around the same time as the original clinical trials in children might yield additional insight. But results from those trials are not fully available. Data from one of the studies appear on the government’s trial registry, but the results are “not in a level of detail that scientists in the field expect or can fully utilize,” he says. The other study has no public results; the lead investigators of both studies did not respond to multiple requests for comment.
One outstanding question about aripiprazole is how well it works in the long term. Otsuka completed a small study in 2014, the results of which suggested the drug has limited value past 28 weeks of use; the FDA then required the drug’s makers to add this detail to its label. But many researchers say the study was too small for them to draw conclusions about the drug’s usefulness over a long period. The study also hinted that girls fare worse on aripiprazole than do boys, although the reasons for these differences are unclear. Many researchers say these findings in particular warrant further study.
| Year | U.S. Spending in Billions | Annotation |
|---|---|---|
| 2006 | $1.9 billion | |
| 2007 | $2.3 billion | |
| 2008 | $3 billion | |
| 2009 | $4 billion | FDA approves Abilify to treat irritability in autistic children. |
| 2010 | $4.6 billion | |
| 2011 | $5.3 billion | |
| 2012 | $5.7 billion | |
| 2013 | $6.5 billion | |
| 2014 | $7.6 billion | Abilify’s patent expires. |
| 2015 | $4.4 billion | |
| 2016 | $1.3 billion | |
| 2017 | $675.2 million | |
| 2018 | $507.3 million | |
| 2019 | $222.7 million |
Source: IQVIA National Sales Perspectives. Graphic by Krista Fuentes.
Emerging concerns:
I
n 2017, the FDA tasked an independent advisory committee — comprising pediatricians from a range of specialties — with reviewing aripiprazole’s side effects in children.The committee examined a report the FDA had prepared earlier that year highlighting 78 serious cases of adverse events, based on data from the agency’s national drug surveillance program. According to the report, 14 children, including one with autism, had died — 5 of them by suicide. The drug’s label warns that aripiprazole is associated with “suicidal thoughts and behaviors,” but the FDA report concluded that aripiprazole could not directly be linked to any of the deaths.
The report also concluded that no new safety warnings were warranted. In half of the non-fatal cases, the drug had stopped being effective. For the other half, the report said, “there were no clear patterns or trends for a new safety signal.”
The committee’s conclusions after reviewing the report, however, were less reassuring. The members expressed concern about weight gain associated with aripiprazole, and other adverse reactions that can be related to weight gain, such as stroke and heart problems, neither of which appears on the drug’s label for use in children. The FDA’s surveillance data, for instance, included five cases of stroke. One 10-year-old boy had developed coronary artery stenosis, a condition normally seen in adults.
“I understand the child had underlying congenital heart disease, but congenital heart disease at 10 years old does not cause coronary artery stenosis or ischemic cardiomyopathy. That, to me, was like, really?” committee member and pediatrician Christy Turer said during a meeting in Rockville, Maryland, in 2017, according to the meeting’s minutes.
Turer argued that the heart problems, stroke and metabolic issues were all “new safety events” worthy of new warning labels and further study. Another member agreed with her, but the remaining 12 did not. Turer requested that the FDA follow up on her concerns over cardiovascular side effects, but she says she never heard back from agency officials. “[They are] not held to doing that or communicating back to us if they looked into it,” she says.
In response to questions about these concerns, an FDA spokesperson told Spectrum that the agency had decided not to pursue any inquiry into an association between aripiprazole and an increased risk of cardiovascular problems in children. “We did not receive any follow-up information on the cases that provided additional information suggesting that aripiprazole caused the events,” the spokesperson said.
Despite these concerns, some clinicians say that having aripiprazole as an option is better than nothing — at least until research suggests otherwise. “When you are in the clinic, you have people with real problems,” London says. “You can’t just throw your hands up and say, ‘Go home, I have nothing to do for you because the studies don’t work.’”
Amber Lesovoy, though, has a different perspective: She says doing nothing would have been better than using aripiprazole. She still blames the drug for Jaymes’ “unnecessary suffering.”
Jaymes is now 16. He has continued to gain weight, and he has become increasingly violent. His family moved him to a group home about an hour away from their house. But he acts up when he is at the home — about a year ago, for example, he became angry and tried to swallow his hearing aid. Still, it is the safest option for Jaymes and the rest of the family, Lesovoy says.
“Medication is a necessary evil for Jaymes, and I understand that,” she says. “But I really regret certain ones, and Abilify is one of the ones I really regret.”
Syndication
This article was republished in The Scientist.
This article was republished in Popular Science.
Recommended reading

Too much or too little brain synchrony may underlie autism subtypes

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome
Explore more from The Transmitter

Proposed NIH budget cut threatens ‘massive destruction of American science’
Smell studies often use unnaturally high odor concentrations, analysis reveals