Genetic testing for autism, explained
No genetic test can say whether a person has autism, but it may point to a cause for the condition or for any related complications.

Autism is primarily a genetic condition: Most of the risk for autism comes from genes1. Mutations in more than 100 genes are known to lead to the condition.
There are four types of tests that can detect these mutations, as well as structural variations that may lead to autism. As researchers learn more about the genetics of autism, the tests have become more informative: More of the mutations they find have ties to autism and to known health consequences.
Here’s a primer on how genetic tests work, their value for autism and what to expect from the results.
Is there a genetic test for autism?
No. A genetic test cannot diagnose or detect autism. That’s because myriad genes along with environmental factors may underlie the condition. Roughly 100 genes have clear ties to autism, but no single gene leads to autism every time it is mutated.
For example, only about one in four people missing a stretch of chromosome 16 called 16p11.2 has autism. This and other mutations are also associated with other conditions, such as epilepsy or intellectual disability.
Why would an autistic person get a genetic test?
If a test reveals a harmful mutation with known ties to autism, the result could give the autistic person and her family an explanation for the condition. Some families also find emotional and practical support from others dealing with the same mutation.
There are no drugs tailored to particular autism mutations. But the mutations are often linked to other health problems, such as epilepsy, kidney problems or obesity, so having the information could help prevent or treat those problems.
What types of genetic tests are available?
There are four main types of tests. The oldest is karyotyping, the inspection of chromosomes under a microscope. This test reliably detects changes to segments larger than 10 million base pairs.
A test called chromosomal microarray analysis identifies duplications or deletions of DNA too small to show up on a karyotype. Still, a karyotype is necessary to identify instances in which chromosomes evenly trade a chunk of genetic material.
To detect even smaller duplications or deletions, and single base-pair swaps, clinicians must sequence or scan for mutations across single genes. Some clinicians use commercial autism tests that sequence a predetermined set of genes, but these panels often do not include top autism genes2.
An alternative is to sequence all of a person’s protein-coding DNA, or the exome. Clinicians may sequence the exomes of both parents as well as the child to find mutations present in only the child. These spontaneous mutations are more likely to contribute to autism than are inherited ones. Exome sequencing is expensive, however, and often not covered by insurance.
Sequencing the entire genome is the most thorough method. It reveals mutations in any part of a person’s genome, not just the 1 percent that includes genes. It is still only a research tool, but as its price falls and it becomes more widely available, it could replace the other tests.
For now, American medical academies recommend only karyotyping or chromosomal microarray analysis for autism. They also advise looking for point mutations in FMR1, MECP2 or PTEN, but only when a child shows other signs of the syndromes associated with mutations in these genes.
What proportion of autistic people find answers from genetic tests?
Relatively few. Karyotyping finds a relevant mutation in 3 percent of autistic people, and microarray analysis in 10 percent3. Sequencing the three genes associated with syndromes could identify an autism mutation in 14 percent of autistic people
Combining these methods with sequencing the exome could yield results in as much as 40 percent of people with autism.
In one 2015 study, microarrays found mutations that could explain autism in 9 percent of children with the condition. Sequencing exomes revealed mutations in another 8 percent4.
The likelihood of finding a known genetic variant increases if the autistic person also has intellectual disability, seizures or unusual facial features.
What if a genetic test turns up nothing?
A negative result does not mean the person does not have a mutation that can cause autism. The test in question might not pick up that particular mutation, or perhaps the mutation does not yet have a known connection to autism.
Many of the genes linked to autism today were not associated with the condition five years ago. Most genetic testing facilities reanalyze results once a year based on the latest findings.
References:
Corrections
A previous version of this article incorrectly stated the size of the DNA segments karyotyping can detect.
Recommended reading

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys

PTEN problems underscore autism connection to excess brain fluid
Explore more from The Transmitter
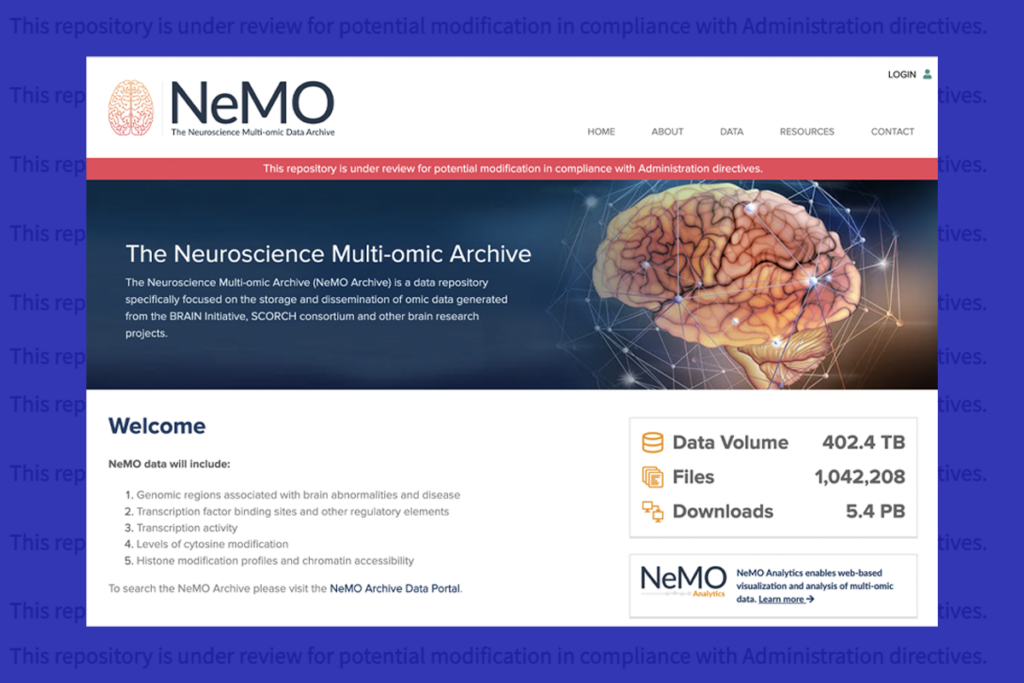
U.S. human data repositories ‘under review’ for gender identity descriptors