Fragile X syndrome’s link to autism, explained
Fragile X syndrome is a leading genetic cause of autism. People who have either condition often share certain traits, such as difficulties in social situations.
Fragile X syndrome is a leading genetic cause of autism. About one in three people with the syndrome also has autism. But even those who do not have autism often share certain autistic traits, such as avoidance of eye contact and difficulties in social situations. Mutations in the gene FMR1, which cause fragile X syndrome, account for up to 5 percent of autism cases.
For these reasons, research on fragile X can provide insights into the biology of autism and its treatment. Here is what scientists know about the mechanisms that underlie fragile X and some research angles they are pursuing.
What is fragile X syndrome?
Fragile X syndrome is the most common cause of intellectual disability. It affects roughly 1 in 4,000 men and about half as many women1. People with the syndrome also tend to have unusual physical features, such as a long face, large ears and flat feet. Some men have large testes, and some people with the condition have seizures.
What is the relationship between fragile X syndrome and autism?
Almost 50 percent of men and 16 percent of women with fragile X also have autism, according to the U.S. Centers for Disease Control and Prevention. Other studies have hinted that up to 90 percent of men with fragile X have some autism traits, such as a tendency to avoid eye contact2. Studies indicate that these traits may present differently in the two conditions. For instance, people with fragile X may show a few classic repetitive behaviors, such as hand-flapping, whereas autistic people typically have a broad range of repetitive behaviors, restricted interests or both. People with fragile X and those with autism may also have divergent developmental trajectories: For instance, social problems may worsen more, or more rapidly, in autistic people than in those with both autism and fragile X.
What causes fragile X?
In most cases, the syndrome is caused by a mutation in FMR1, located on the X chromosome. People with fragile X have more than 200 repetitions of a sequence of three nucleotides, ‘CGG,’ at the start of the gene; typical people have 54 or fewer of these repeats. Under a microscope, this CGG expansion can cause the tip of the X chromosome to appear ‘fragile.’
The expanded repeats can silence the production of a protein called FMRP. This protein serves critical functions, such as controlling the production of proteins at synapses, the junctions between neurons.
The leading theory of fragile X holds that when FMRP is missing, protein synthesis can run rampant and disrupt cognitive processes. A study published last month, however, has complicated scientists’ understanding of the syndrome: It hints that loss of FMRP instead causes a dearth of proteins.
What is the fragile X syndrome ‘premutation’?
The fragile X ‘premutation’ is defined as having 55 to 200 CGG repeats in FMR1. The premutation tamps down production of FMRP but does not silence it. Because premutation carriers may not show outward signs, the prevalence of premutations is unknown. Estimates range from 1 in 148 to 1 in 291 in women and from 1 in 290 men to 1 in 855 in men in the United States.
Some women with the premutation develop a condition called fragile X-associated primary ovarian insufficiency, which can trigger early menopause. Both men and women with the premutation may develop a condition called fragile X-associated tremor/ataxia syndrome, which causes tremors and cognitive problems. The risk of developing this condition increases with age: Estimates suggest 30 percent of affected men and 8 to 16.5 percent of affected women over age 50 have it1.
The repeats of the premutation can sometimes expand in future generations to the full syndrome. The more repeats in the mother’s premutation, the greater the chance the child will have a full mutation.
Some people have between 45 and 54 CGG repeats — a so-called ‘gray zone’ mutation. Little is known about the effects of this mutation, although evidence suggests it can lead to some features of fragile X-associated tremor/ataxia syndrome.
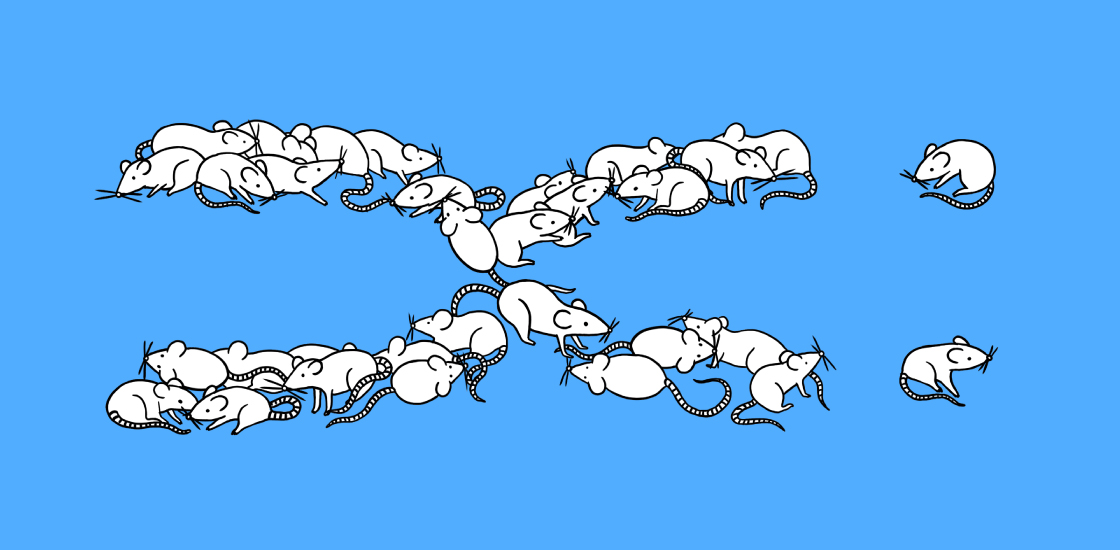
Are there animal models available to study fragile X?
Researchers have developed mouse and rat models of fragile X syndrome by deleting FMR1. The brains of these mice respond abnormally to social stimuli, such as meeting a new mouse. The mutant mice also show alterations in a brain circuit involving the prefrontal cortex, which plays a role in social cognition.
Whether insights from the mice apply to people with the condition is unclear. The behaviors seen in mice that lack FMR1 are often inconsistent — and in many cases do not resemble those in people. For instance, the mutant mice do not show cognitive problems, one of the core features of fragile X. An animal model that faithfully mimics the syndrome would help researchers test treatments and trace the syndrome’s origins.
Are there treatments for fragile X syndrome?
A range of available behavioral therapies may improve speech and language abilities in people with fragile X. But there are no approved drugs for the syndrome.
Researchers are investigating many candidate drugs, including several that block a protein called mGluR5. Some of the candidates, such as arbaclofen and mavoglurant, have been shown to restore protein production and ease problems with learning and memory in the mutant mice. But none of the drugs has fared well in clinical trials.
That may be because the trials used the wrong markers to measure the drugs’ effectiveness. Or it may because the trials involved adolescents and adults, whose brains may no longer respond to intervention. One team is testing mavoglurant in young children and using a test of language learning to measure its effectiveness. They plan to pair the drug with an intensive language intervention.
Other teams are testing a drug called lovastatin, which is used to treat high cholesterol levels and has been shown to reduce seizures in fragile X mice. Researchers are also testing a drug that targets the enzyme PDE4D and seems to improve social behaviors in the mutant mice3.
What are the next steps for the field?
Researchers are pushing to develop good outcome measures for clinical trials and to investigate promising drug candidates. Other efforts aim to clarify the functions of FMRP or to repair the mutation. In a March study, for example, researchers used a gene-editing tool to remove chemical tags from CGG repeats in cells from a person with fragile X. The treatment restored FMRP expression to 90 percent of normal levels.
References:
Recommended reading

Developmental delay patterns differ with diagnosis; and more

Split gene therapy delivers promise in mice modeling Dravet syndrome

Changes in autism scores across childhood differ between girls and boys
Explore more from The Transmitter

‘Natural Neuroscience: Toward a Systems Neuroscience of Natural Behaviors,’ an excerpt

